COPD fought by Vitamin D - many studies
Severe COPD exacerbations 3.4 X more likely if low vitamin D – Jan 2025
The Role of Severe Vitamin D Deficiency in Predicting the Risk of Severe Exacerbation in Patients With Chronic Obstructive Pulmonary Disease
Int J Chron Obstruct Pulmon Dis. 2025 Jan 22:20:171-179. doi: 10.2147/COPD.S489650
Li Zhou 1 2 3 4, Cunqiao Han 5, Yue Zhou 1 2 3 4
Background: This study aims to investigate the association between vitamin D levels and the risk of severe acute exacerbations of chronic obstructive pulmonary disease (AECOPD).
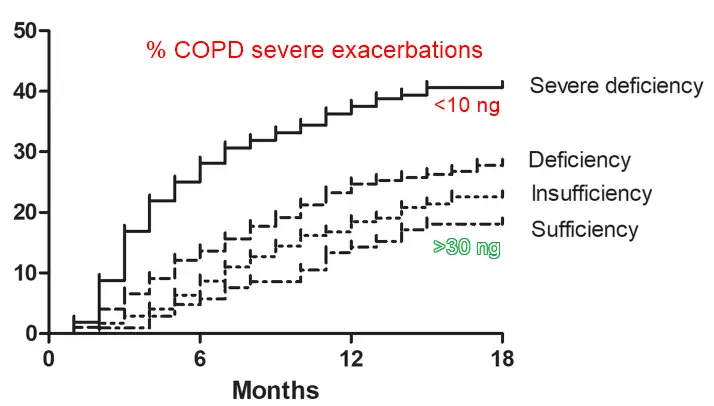
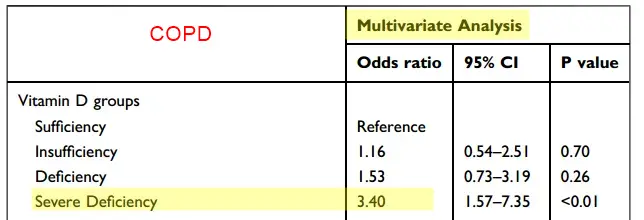
Methods: We conducted a prospective observational study with 636 COPD patients admitted for exacerbations between January 2021 and December 2022. Patients were categorized based on serum 25-hydroxyvitamin D levels: severe deficiency (<10 ng/mL), deficiency (10-20 ng/mL), insufficiency (20-30 ng/mL), or sufficiency (>30 ng/mL). Severe exacerbation was defined when the patient visits an emergency room or is hospitalized due to COPD exacerbation. Multivariate Cox regression was used to evaluate the risk associated with vitamin D deficiency.
Results: Over an 18-month follow-up, 178 (28.0%) patients experienced at least one severe exacerbation. The severe deficiency group had the highest exacerbation rate (40.6%), followed by deficiency (27.8%), insufficiency (22.5%), and sufficiency (18.1%) groups (P<0.01). Multivariate Cox regression analysis showed that severe vitamin D deficiency was significantly associated with an increased risk of severe exacerbations (HR=2.74, 95% CI: 1.55-4.84; P<0.01) compared to vitamin D sufficiency.
Conclusion: Severe vitamin D deficiency is a significant predictor of severe COPD exacerbations, highlighting the importance of routine vitamin D assessment and supplementation in COPD management.
📄 Download the PDF from VitaminDWiki
COPD in ICU 1.8 X less likely to die if had been taking any vitamin D for >7 days - April 2024
_Vitamin D supplementation may be beneficial in improving the prognosis of patients with chronic obstructive pulmonary disease in the intensive care unit: a retrospective study
Front. Med., 22 March 2024 https://doi.org/10.3389/fmed.2024.1334524
Qian He † Song Hu † Jun Xie Yunqi Ge Chong Li *
Department of Respiratory and Critical Care Medicine, Third Affiliated Hospital of Soochow University, Changzhou, China
ICU COPD Mortality
People with COPD who had been taking a lot of vitamin D probably did not even enter the hospital or ICU
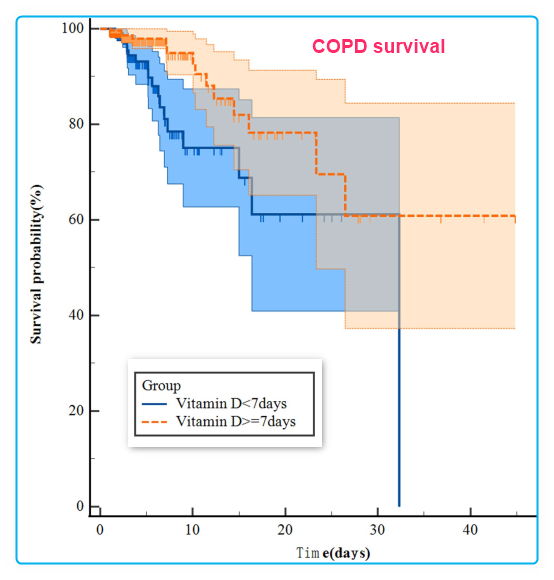
Background: Vitamin D is a crucial fat-soluble vitamin that has garnered significant attention due to its potential impact on respiratory health. It is noteworthy that many patients with chronic obstructive pulmonary disease (COPD) often experience deficiencies or insufficiencies of vitamin D. To address this issue, our retrospective study aimed to explore the potential association between serum 25-hydroxyvitamin D concentration and the prognoses of COPD patients in the Intensive Care Unit (ICU).
Methods: This study utilised data from the Medical Information Marketplace in Intensive Care IV (MIMIC-IV), a database of patients admitted to the Intensive Care Unit at Beth Israel Deaconess Medical Center (BIDMC) in the United States of America, with a focus on patients with a diagnosis of COPD. These patients were categorized into two groups: those who received vitamin D supplementation during their ICU stay and those who did not. We assessed in-hospital mortality and ICU mortality outcomes. Our analysis involved various analytical tools, including Kaplan–Meier survival curves, Cox proportional risk regression models, and subgroup analyses, to investigate the relationship between vitamin D supplementation and these outcomes. Additionally, we employed propensity-score matching (PSM) to enhance the reliability of our findings.
Results: The study included a total of 3,203 COPD patients, with 587 in the vitamin D group and 2,616 in the no-vitamin D group. The Kaplan–Meier survival curve demonstrated a significant difference in survival probability between the two groups. After adjusting for potential confounders using Cox regression models, the vitamin D group exhibited a substantially lower risk of in-hospital and ICU mortalities compared to the no-vitamin D group. The hazard ratios for in-hospital and ICU mortalities in the vitamin D group were 1.7 (95% CI: 1.3, 2.3) and 1.8 (95% CI: 1.2, 2.6), respectively. Propensity-score matching (PSM) estimation yielded consistent results. Furthermore, in the subgroup analysis, female patients who received vitamin D supplementation showed a reduced risk of in-hospital mortality.
Conclusion: The study suggests that vitamin D supplementation may be linked to a reduction in in-hospital and ICU mortalities among COPD patients in the ICU. Of particular note is the potential benefit observed in terms of in-hospital mortality, especially for female patients.
📄 Download the PDF from VitaminDWiki
See also VitaminDWiki
Vitamin D is one of the alternate COPD therapies – March 2021
COPD quality of life improved by 400,000 IU Vitamin D loading dose – RCT July 2019
COPD exacerbations 2X less often if low vitamin D then supplemented – meta-analysis Jan 2019
Worse breathing with COPD is related to lower Vitamin D – June 2018
COPD ICU stay is 2.4 days longer if low vitamin D – Oct 2015
Those with Asthma or COPD had half the response to Vitamin D – March 2020
26 health factors increase the risk of COVID-19 – all are proxies for low vitamin D
- CDC list of high-risks for COVID-19 includes COPD
60+ VitaminDWiki pages have COPD OR CHRONIC OBSESIVE in the title
This list is automatcially updated
{LIST()}
5X more likely to have low Vitamin D if have COPD - Nov 2020
Vitamin D deficiency is associated with chronic obstructive pulmonary disease and exacerbation of COPD
Clin Respir J. . 2020 Nov 20. doi: 10.1111/crj.13310
Komarla Sundararaja Lokesh 1, Sindaghatta Krishnarao Chaya 1, Biligere Siddaiah Jayaraj 1, Praveena Attahalli Shivanarayanprasad 2, Murali Krishna 3 4, Purnima Madhivanan 5 6 7, Mahesh Anand Padukudru 1 7 8
Introduction: Low Vitamin D levels have been associated with Chronic Obstructive Pulmonary Disease (COPD) and acute exacerbations.
Objectives: There is paucity of data on vitamin D and COPD, its severity and exacerbations in populations that are exposed to sunlight regularly with high levels of physical activity most of their lives.
Methods: Serum levels of 25-OH-Vitamin-D was assessed in 100 COPD subjects and 100 age- and gender-matched controls from the rural community based MUDHRA cohort in South India. Levels of <20ng/ml was defined as Vitamin D deficiency. Smoking habits, occupation, Charlson co-morbidity index, Standard of living index(SLI), body mass index(BMI), 6-minute walking distance were examined for associations with by logistic regression between controls and COPD subjects. Unconditional logistic regression was used to examine the association with exacerbation of COPD.
Results: Vitamin D deficiency was observed in 64.5%(95%CI 57.7-70.8) of the subjects in spite of regular exposure to sunlight. Subjects with COPD had higher risk of Vitamin D deficiency (Adjusted OR: 5.05 ; 95%CI 1.4-17.8) as compared to controls.
Among subjects with COPD, Vitamin D deficient subjects were 3 times more likely to have exacerbations in the previous year (Adjusted OR:3.51; 95%CI 1.27-9.67) as compared to COPD subjects without Vitamin D deficiency. Levels of Vitamin D below 20.81 ng/ml and below 18.45 ng/ml had the highest levels of combined sensitivity and specificity for COPD and exacerbations respectively.
Conclusion: In a rural population exposed to sunlight many hours in a day throughout their lives, low Vitamin D levels were associated with COPD and exacerbations of COPD.
Emphysema (COPD) worsens 3X faster if less than 10 ng of Vitamin D – Jan 2020
Severe Vitamin D Deficiency Is Associated With Emphysema Progression in Male Patients With COPD
Respir Med, 163, 105890 2020 Jan 30, DOI: 10.1016/j.rmed.2020.105890
Changhwan Kim 1, Yousang Ko 2, Ji Ye Jung 3, Jae Seung Lee 4, Chin Kook Rhee 5, Jin Hwa Lee 6, Ji-Hyun Lee 7, Ji-Yong Moon 8, Seong Yong Lim 9, Kwang Ha Yoo 10, Joon Beom Seo 11, Yeon-Mok Oh 12, Sang-Do Lee 13, Yong Bum Park 14
Background: Patients with chronic obstructive pulmonary disease (COPD) have an increased risk of vitamin D deficiency. Vitamin D levels also correlate with lung function in patients with COPD. However, there are few reports on vitamin D deficiency and emphysema severity in COPD. This study aimed to investigate the effects of plasma 25-hydroxyvitamin D (25-OHD) level on emphysema severity in male COPD patients.
Methods: A total of 151 male subjects were selected from the Korean Obstructive Lung Disease (KOLD) cohort. Subjects were subdivided into four subgroups according to their baseline plasma 25-OHD level: sufficiency (≥20 ng/ml), mild deficiency (15-20 ng/ml), moderate deficiency (10-15 ng/ml), and severe deficiency (<10 ng/ml).
Results: Baseline computed tomography (CT) emphysema indices revealed significant differences among the subgroups (p = 0.034). A statistically significant difference was also observed among the subgroups regarding change in the CT emphysema index over 3 years (p = 0.047). The annual increase in emphysema index was more prominent in the
severe deficiency group (1.34% per year)
than in the other groups (0.41% per year) (p = 0.003).
Conclusions: This study demonstrates that CT emphysema indices were different among the four subgroups and supports that severe vitamin D deficiency is associated with rapid progression of emphysema in male patients with COPD.
Small Vitamin D doses not help COPD - meta-analysis Oct 2023
📄 Download the PDF from VitaminDWiki
50,000 IU weekly - 17X more likely to improve breathing - 2014
Efficiency of supplemental vitamin D in patients with chronic obstructive pulmonary disease.
British Journal of Medicine and Medical Research 2014 Vol. 4 No. 16 pp. 3031-3041
IHeidari, B.; Monadi, M.; Asgharpour, M.; Firouzjahi, A.; Tilaki, K. H.; Monadi, M.
📄 Download the PDF from VitaminDWiki
Aims: To investigate the impact of supplemental vitamin D on pulmonary function in patients with stable chronic obstructive pulmonary disease (COPD).
Study Design: Case-control study Place and Duration of Study: Department internal medicine, Rouhani hospital, Babol university of medical sciences, Babol, Iran.
Over six months from September 2011 through February 2012
Methodology: Patients with COPD allocated to the treatment or control group intermittently. Thirty patients in the treatment group received 50.000 IU oral cholecalciferol weekly for two months plus routine treatment and 28 patients who served as controls received only their usual medications. The serum 25-hydroxyvitamin D (25-OHD) and FEV1% was measured at baseline and two months later. The primary objective was to determine treatment response defined as 5% or greater increase from baseline in FEV1% and the secondary objective was to determine the association between vitamin D supplementation and treatment response. In statistical analysis Spearman's correlation coefficient was used to determine correlation and logistic regression analysis with calculation of odds ratio (OR) was used to determine association.
Results: Mean age of the patients and controls was 67.1±10.5 years and 66.±12.2 years respectively (P=0.83).
Thirteen patients (43.3%) versus 3 (10.7%) controls responded to treatment (P=0.009).
Treatment response was positively correlated with mean serum 25-OHD changes from baseline (Spearman's correlation coefficient=0.358, P=0.026).
Mean 25-OHD change from baseline in the responders was significantly higher than in no responders (P=0.031).
Mean 25-OHD changes were positively correlated with FEV1% (P=0.013).
Vitamin D supplementation increased the treatment response by OR=6.37 (95% CI, 1.57-25.8).
After adjustment for inhaled bronchodilator, corticosteroid therapy, age, weight, smoking, ESR and CRP the odds of treatment response in vitamin D group increased to 17.1 (95%CI, 2.39-122, P=0.005).
Conclusion: The findings of this study indicate that, two months vitamin D supplement to the drug regimen of COPD confers small pulmonary function improvement as compared with controls and justify serum 25-OHD measurement in COPD. Raising serum 25-OHD to sufficient levels with longer duration of treatment may exert further benefits
50,000 IU helped COPD in many ways - Jan 2015
Effect of vitamin D replacement in chronic obstructive pulmonary disease patients with vitamin D deficiency
Egyptian Journal of Chest Diseases and Tuberculosis, doi:10.1016/j.ejcdt.2015.01.002
Nasef Abdel Salam A. Rezka, , Nasser Yehia A. Alyb, Asem Abdel Hamid Hewidya
Introduction
Vitamin D deficiency is prevalent among patients with chronic obstructive pulmonary disease (COPD) and comes to be more frequent with increased disease severity. We aimed to assess the role of vitamin D supplementation in patients with severe COPD.
Patients and methods
We studied 30 patients with severe COPD and vitamin D deficiency. All patients received oral vitamin D3 50,000 IU once weekly for 8 weeks, followed by a daily dose of 800 IU thereafter.
Pulmonary function tests,
six minute walk test (6MWT),
maximum inspiratory pressure (MIP),
maximum expiratory pressure (MEP),
C-reactive protein (CRP), and
serum vitamin D level
were assessed at the start of the study and 1 year later.
The frequency of exacerbations was recorded a year before and a year after vitamin D supplementation.
Results
The mean serum vitamin D level was 11.80 ± 2.40 ng/dl and reached 55.30 ± 5.65 ng/dl a year after vitamin D intake (p < 0.001).
We found a significant improvement in
dyspnea scale (p < 0.003),
6MWT (p < 0.001) (six minute walk test )
MVV (p < 0.001),
MIP (p = 0.006) (maximum inspiratory pressure )
MEP (p < 0.001), (maximum expiratory pressure ) coupled with a
decrease in disease exacerbations (p < 0.001) and
(decrease) CRP (p < 0.001)
a year after vitamin D replacement. However, the FEV1 and FVC did not differ significantly.
Conclusion: Vitamin D replacement improved dyspnea, physical performance and decreased the frequency of exacerbation in severe COPD patients with vitamin D deficiency.
📄 Download the PDF from VitaminDWiki.
50,000 IU weekly helped elderly with COPD tolerate exercise - 2013
High Dose Vitamin D3 Improves Exercise Tolerance in Elderly Patients with Chronic Obstructive Pulmonary Disease
Obstructive Pulmonary Disease. J Gerontol Geriat Res 2: 127. doi:10.4172/2167-7182.1000127
Mehrnaz Asadi Gharabaghi1*, Mehrnoush Asadi Ghrabaghi2, Mohsen Arabi3, Mohammad Reza Zahedpour Anaraki1 and Gholamreza Derakhshan Deilami1
1Department of Pulmonary Medicine, Tehran University of Medical Sciences, Tehran, Iran 'Department of Pharmacy, Maharashtra Institute of Technology, Pune, India 3Department of Medicine, Iran University of Medical Sciences, Tehran, Iran
•Corresponding author: Dr. Mehrnaz Asadi Gharabaghi, Department of Pulmonary Medicine, Imam Khomeini Hospital, Tehran, Iran, Tel: +982161192646; E-mail: asadi_m@tums.ac.ir
Background: In addition to airflow limitation, peripheral muscle dysfunction is a limiting factor in physical performance of patients with chronic obstructive pulmonary disease (COPD).Any measure to improve global muscle function in COPD patients such as vitamin D replacement seems to enhance exercise tolerance of these patients.
Aim: The aim of present study was to study the effect of vitamin D replacement therapy on exercise tolerance of a group of stable COPD patients with vitamin D deficiency or insufficiency.
Methods: It was an experimental, unblended open-label trial. A total number of 25 stable COPD patients were enrolled in the study in the period between March 2012 and OCT 2012 and received 50,000 IU vitamin D weekly for 4-8 weeks in addition to their standard medical therapy as before. They were also subdivided into two subgroups based on serum 25 hydroxy vitamin D,25(OH)D( <10 ng/ml and 10-30 ng/ml).Pulmonary function tests, six-minute walk distance test(6MWD) were measured at baseline and three months after the enrollment.
Results: By the end of study, there was significant improvement in the distance walked during 6-minute walk test. This improvement was documented in both subgroups of patients. However, the perceived dyspnea during test did not differ from baseline value by the end of the study. Also, only patients with serum 25(OH) D, 10 -30 ng/ml showed the significant increase in their mean value of FEV1 by the end of the study.
Conclusion: Vitamin D replacement therapy is an effective measure to improve exercise tolerance of stable COPD patients with vitamin D deficiency or insufficiency
Clipped from Discussion
The present study explored the effect of vitamin D replacement therapy in exercise capacity of COPD patients. Field tests are commonly used to evaluate exercise tolerance of patients with various cardio respiratory diseases. Six-minute walk (6MWT) and shuttle walking tests are commonly used with this aim as they are easy to perform and need minimal equipment. We utilized 6MW test and found that vitamin D supplementation significantly improved distance walked during 6MWT, signifying improvement in the exercise tolerance of COPD patients with vitamin D insufficiency/deficiency. Six minute walk test is a simplified exercise test assessing overall functional capacity of patients. It is influenced by many factors including cardio respiratory function, comorbid disorders, age, BMI, height, nutrition and peripheral muscle strength [10]. Lower limb muscle strength has been reported to have significant and positive relationship with the distance walked during 6MWT [21]. Peripheral muscle dysfunction is a well-known complication in COPD patients and vitamin D insufficiency that is common in COPD, contributes to its development. Therefore, it is prudent to assume that insufficient vitamin D store in COPD patients reduces their maximum distance walked during 6MWT .As a supportive evidence, Ringbaek et al., [9]. showed that COPD patients with vitamin D deficiency who undergo PR have poorer outcome in training programs compared with patients with enough vitamin D reservoir [9]. There is also a strong document stating vitamin D supplementation improves exercise capacity of COPD patients receiving pulmonary rehabilitation [22]. Vitamin D receptors exist on various organs including skeletal muscles. Vitamin D affects muscle metabolism in different pathways. For instance, after binding to its receptor, 1, 25(OH) D3 causes both voltage-dependent calcium channels and calcium-release-activated channels to be opened and facilitates calcium entry to the cells to initiate myosin and actin interaction and finally muscle contraction. Therefore, it is not surprising that vitamin D insufficiency causes proximal muscle weakness even in the presence of normocalcemia [23]. The exact mechanisms that vitamin D improves exercise tolerance in COPD patients are not known. Improvement in oxidative capacity of musculoskeletal tissues, reducing anaerobic threshold are areas of uncertainty that need to be addressed in future studies [18].
Yet, there are controversies about contribution of vitamin D deficiency to muscle dysfunction in COPD patients. Jackson et al. studied the correlation between vitamin D status , muscle strength and quadriceps endurance in a group of COPD patients and reported no significant correlation, and attributed their finding to muscle resistance to vitamin D [24]. There are few studies evaluating the effect of vitamin D supplementation on six -minute walk test as a primary outcome in COPD patients. But in a double-blind randomized controlled trial in patients with heart failure, vitamin D supplementation did not improve exercise tolerance, muscle strength and six minute walk distance [25].
There are few reports investigating the contribution of vitamin D status to respiratory muscle strength in COPD patients. Also, there is little study to address the optimal level of 25 (OH) D in COPD patients to achieve maximum exercise capacity. Based on large cross-sectional data, when serum level of 25(OH) D increases from 9 ng/ml to 37 ng/ml, muscle strengths increases too and higher level of 25 (OH) D associated with better lower extremity function [26]. According to the statement of International osteoporosis Foundation in 2010, the target serum level of 25(OH) D of 30ng/ml should be maintained in all elderly patients [27]. In our study, the serum level of 25(OH) D after three months was correlated positively with distance walked during 6MW test at the end of study. All patients achieved serum level of 25(OH) D more than 30 ng/ by the end of the study with mean serum level of 62.7 ± 16 ng/ml. Similarly, the increase in 6MWD in insufficiency group was more than deficient patients by the end of the study. As mentioned, higher serum level of 25 (OH) D correlates with better skeletal muscle function and may enhance exercise tolerance. We treated our patients with almost the same regimen, irrespective of being insufficient or deficient in vitamin D that means 50,000 IU orally weekly for 4-8 weeks. Therefore, we assumed that the percentage of patients whose improvement in 6MWT was more than MCID would differ significantly in two subgroups but data analysis showed that was not the case. We attributed this finding to the small number of patients in each subgroup as the measured P value was only 0.06.
Patients with COPD often experience increased dyspnea during exercise that limits their exercise performance further. Ventilatory demands increase during exercise, and expiratory flow limitation causes progressive hyperinflation, so greater respiratory muscle activity is needed to overcome the increased elastic work at high lung volumes. The increased work of breathing translates into increased perception of dyspnea [28]. However, this exertional dyspnea might be in some part due to increased respiratory drive secondary to peripheral muscle dysfunction [29]. We assumed that vitamin D replacement would decrease perceived dyspnea during 6-minute walk distance test at least by improving peripheral muscle dysfunction. We used Borg category scale to rate the dyspnea. However, the mean Borg scale score during walk test before and after the intervention showed no significant improvement in perceived dyspnea while there was significant difference in distance before and after vitamin D replacement. The observed discrepancy between dyspnea score and the distance may be due to inability of elderly patients to discriminate easily between terms such as slight dyspnea and somewhat sever dyspnea (2 vs.4 score respectively). Based on the documentations by Muza et al., [30] psychometric measures such as visual analogue and Borg scale have good reproducibility but the proximity of verbal descriptors might be confusing and discouraging for patients with COPD. Therefore, rating dyspnea by Borg scale might not be highly sensitive [30,31].
Mean FEV1 value increased from baseline value at the three months in our study. But, the increase in deficient patients [25(OH) D<10 ng/ ml] did not reach statistically significant value. However, in patients with vitamin D insufficiency; the increase in mean value of FEV1 was significant. Black et al., [32] surveyed the relationship between vitamin D status and pulmonary function tests and showed men and women with serum level of 25(OH) D above 35ng/ml had FEV1 values 176 milliliter more than their matched controls [32]. However, Lehouk et al., [33] showed that high dose vitamin D administration to COPD patients with vitamin D insufficiency did not affect the FEV1 or the time to first exacerbation [33]. Also in a randomized clinical trial, severe COPD patients did not show any significant change in their physical performance or respiratory health status despite receiving 2000 vitamin D daily for 6 weeks [34]. In Hertfordshire Cohort Study, UK, the investigators did not find any significant relationship between serum 25(OH) D and FEV1 in COPD patients [35]. In addition Kunisaki et al., [36] showed that vitamin D status has no relationship with short term response of FEV1 to inhaled steroid [36].The observed increase in mean FEV1 in the patients with vitamin D insufficiency in our study may not reflect the positive effect of vitamin supplementation on lung function test but may rather signify the seasonal and biologic variations of lung function tests in COPD patients.
There were limitations in our study. First; we did not study the effect of vitamin D replacement on end expiratory volume, inspiratory capacity and static dynamic hyperinflation during exercise. We did not measure muscle strength and quadriceps endurance before and after vitamin D supplementation. We did not follow patients beyond three months to evaluate their physical performance. Also, the number of matched COPD patients with sufficient vitamin D status was very small in our pulmonary clinic so we had no control group. Lastly, the sample size was very small.
In conclusion, it is worthy to state that to optimize medical treatment of patients with COPD and increase their exercise tolerance, not only airflow limitation but also peripheral muscle weakness needs to be treated appropriately. Functional capacity of COPD patients would not improve unless their lower limb muscle becomes more efficient in energy consumption.
📄 Download the PDF from VitaminDWiki.
Asthma & COPD combined - Sept 2015
Vitamin D deficiency is associated with impaired disease control in asthma-COPD overlap syndrome patients.
Int J Chron Obstruct Pulmon Dis. 2015 Sep 24;10:2017-25. doi: 10.2147/COPD.S91654. eCollection 2015.
Odler B1, Ivancsó I1, Somogyi V1, Benke K2, Tamási L1, Gálffy G1, Szalay B3, Müller V1.
INTRODUCTION:
The association between vitamin D and clinical parameters in obstructive lung diseases (OLDs), including COPD and bronchial asthma, was previously investigated. As asthma-COPD overlap syndrome (ACOS) is a new clinical entity, the prevalence of vitamin D levels in ACOS is unknown.
AIM:
Our aim was to assess the levels of circulating vitamin D (25-hydroxyvitamin D [25(OH)D]) in different OLDs, including ACOS patients, and its correlation with clinical parameters.
METHODS:
A total of 106 men and women (control, n=21; asthma, n=44; COPD, n=21; and ACOS, n=20) were involved in the study. All patients underwent detailed clinical examinations; disease control and severity was assessed by disease-specific questionnaires (COPD assessment test, asthma control test, and modified Medical Research Council); furthermore, 25(OH)D levels were measured in all patients.
RESULTS:
The 25(OH)D level was significantly lower in ACOS and COPD groups compared to asthma group (16.86±1.79 ng/mL and 14.27±1.88 ng/mL vs 25.66±1.91 ng/mL). A positive correlation was found between 25(OH)D level and forced expiratory volume in 1 second (r=0.4433; P<0.0001), forced vital capacity (FVC) (r=0.3741; P=0.0004), forced expiratory flow between 25% and 75% of FVC (r=0.4179; P<0.0001), and peak expiratory flow (r=0.4846; P<0.0001) in OLD patient groups. Asthma control test total scores and the 25(OH)D level showed a positive correlation in the ACOS (r=0.4761; P=0.0339) but not in the asthma group. Higher COPD assessment test total scores correlated with decreased 25(OH)D in ACOS (r=-0.4446; P=0.0495); however, this was not observed in the COPD group.
CONCLUSION:
Vitamin D deficiency is present in ACOS patients and circulating 25(OH)D level may affect disease control and severity.
📄 Download the PDF from VitaminDWiki
Meta-analyses of many studies of Breathing and Vitamin D:
{category}
Breathing and Vitamin D INTERVENTION studies
{category}
See also web
GLOBAL STRATEGY FOR PREVENTION, DIAGNOSIS AND MANAGEMENT OF COPD: 2022 Report
rejects Vitamin D COPD metalanalyses as they only studied people with lower than normal vitamin D
FDA Clears Olodaterol (Striverdi Respimat) for COPD July 2014
- improved lung function compared with placebo vs Vitamin D provides 17X better improvement
- Note: could not find the above quoted text when looked at again in Jan 2015
- The most common side effects in the clinical study were nasopharyngitis, upper respiratory tract infection, bronchitis, cough, urinary tract infection, dizziness, rash, diarrhea, back pain, and arthralgia.
olodaterol New drug report in UK - with all of the trial data
COPD clininical trials with Vitamin D intervention 20 as of Jan 2019
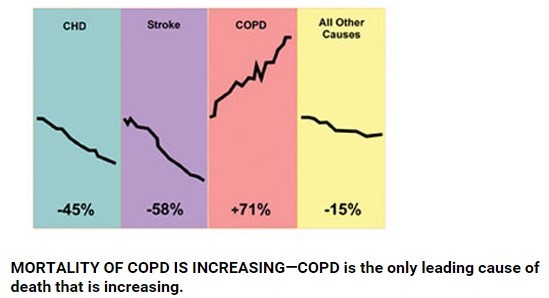
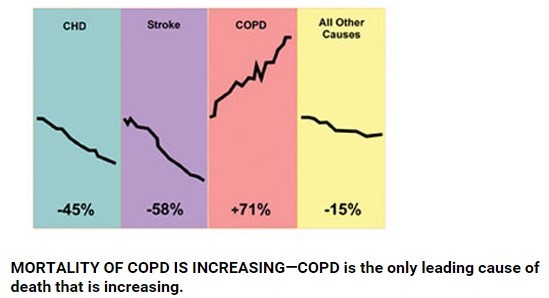
Charts of recent increase in COPD deaths
Big increase in COPD death rate (age adjusted)
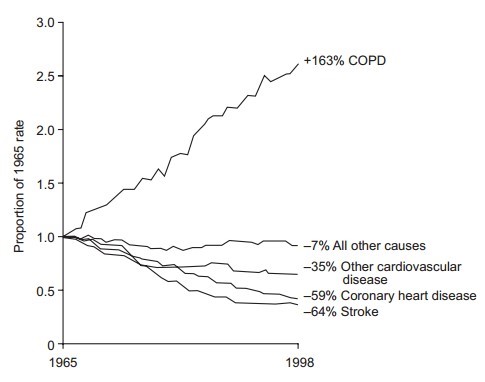
Give Them Comfort: Controlling COPD Symptoms at the End of Life Feb 2009 has the following chart
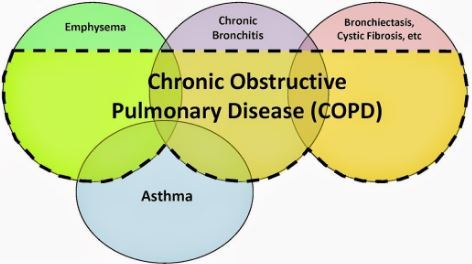
Venn diagrams of breathing problems
COPD has become the 3rd largest global cause of disability: ages 50-69
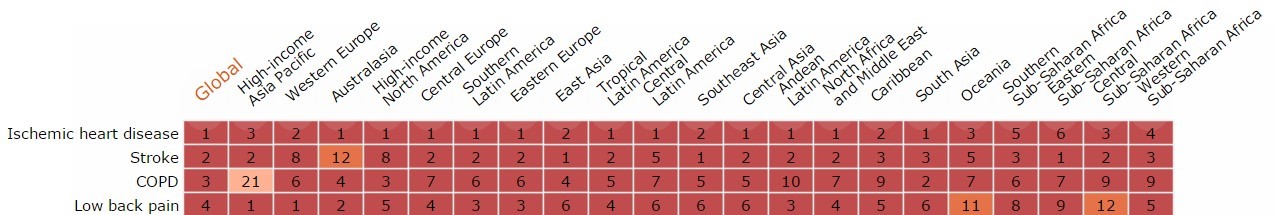
COPD is a major cause of employee death
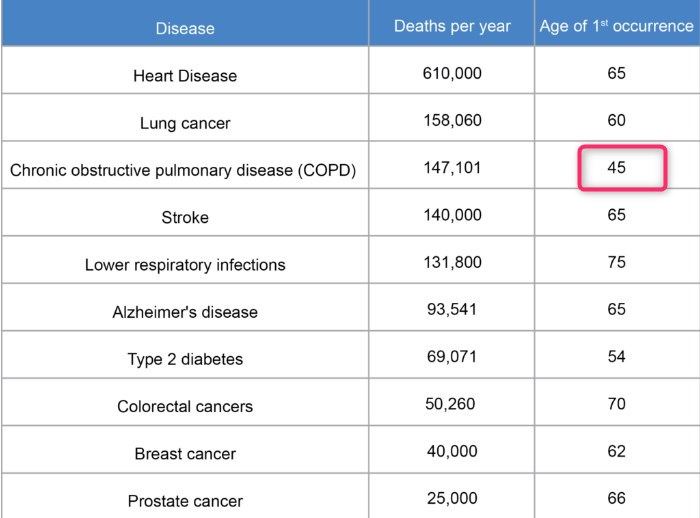
Healthspan Is More Important Than Lifespan, So Why Don’t More People Know About It? May 2017
Data taken from World Wealth Organizations
Chronic Obstructive Pulmonary Disease in London - 2017
Prevalence, determinants and clinical correlates of vitamin D deficiency in patients with Chronic Obstructive Pulmonary Disease in London, UK
Pages 138-145 📄 Download the PDF from VitaminDWiki
David A. Jolliffe, Wai Yee James, Richard L. Hooper, Neil C. Barnes, Claire L. Greiller, Kamrul Islam, Angshu Bhowmik, Peter M. Timms, Raj K. Rajakulasingam, Aklak B. Choudhury, David E. Simcock, Elina Hyppönen, Robert T. Walton, Christopher J. Corrigan, Christopher J. Griffiths, Adrian R. Martineau
Highlights
Vitamin D deficiency is common among UK adults with chronic obstructive pulmonary disease.
Classical environmental determinants of vitamin D status operate in this population.
Vitamin D status associated with clinical markers of lung function.
Genetic variation in the vitamin D pathway did not influence vitamin D status or measures of COPD severity.
COPD and Vitamin D review - Feb 2018
Vitamin D deficiency: What does it mean for chronic obstructive pulmonary disease (COPD)? a compherensive review for pulmonologists.
Clin Respir J. 2018 Feb;12(2):382-397. doi: 10.1111/crj.12588. Epub 2017 Jan 5.
Kokturk N1,2, Baha A1, Oh YM2, Young Ju J2, Jones PW3.
OBJECTIVES:
Vitamin D deficiency and Chronic Obstructive Pulmonary Disease (COPD) are both under-recognized health problems, world-wide. Although Vitamin D has long been known for calcemic effects it also has less known noncalcemic effects. Recent data have shown that Vitamin D deficiency is highly prevalent in patients with COPD and correlates with forced expiratory volume in one second (FEV1 ) and FEV1 decline. The objective of this work was to review the current literature on vitamin D deficiency in relation with COPD.
DATA SOURCE: A literature search, using the words "vitamin D" and "COPD", was undertaken in Pubmed database.
RESULTS:
The noncalcemic effects of vitamin D relating with COPD may be summarised as increasing antimicrobial peptide production, regulation of inflammatory response and airway remodelling. Vitamin D inhibits the production of several proinflammatory cytokines and leads to suppression Th1 and Th17 responses which may be involved in the pathogenesis of COPD. Vitamin D insufficiency may also contribute to chronic respiratory infections and airway colonization so returning vitamin D concentrations to an optimal range in patients with COPD might reduce bacterial load and concomitant exacerbations.Vitamin D is also important for COPD-related comorbodities such as osteoporosis, muscle weakness and cardiovascular diseases. Data about the effect of Vitamin D supplementation on those comorbidities in relation with COPD are been scarce.
CONCLUSION: Improving the blood level of Vitamin D into the desired range may have a beneficial effect bones and muscles, but more studies are needed to test to test that hypothesis.
📄 Download the PDF from VitaminDWiki
COPD patients who do not get summer sun should get Vitamin D - Aug 2018
Vitamin D status is associated with muscle strength and quality of life in patients with COPD: a seasonal prospective observation study.
Int J Chron Obstruct Pulmon Dis. 2018 Aug 28;13:2613-2622. doi: 10.2147/COPD.S166919. eCollection 2018.
Carson EL1, Pourshahidi LK1, Madigan SM2, Baldrick FR1, Kelly MG3, Laird E4, Healy M5, Strain JJ1, Mulhern MS1.
BACKGROUND: Owing to hospitalization, reduced functional capacity and consequently, less sunlight exposure, suboptimal vitamin D status (25-hydroxyvitamin D [25(OH)D]⩽50 nmol/L) is prevalent among COPD patients.
OBJECTIVE: This study aimed to investigate seasonal changes in vitamin D status and any associated changes in fat-free mass (FFM), muscle strength and quality of life (QoL) in COPD patients.
PATIENTS AND METHODS:
COPD patients living in Northern Ireland (n=51) completed study visits at the end of winter (March/April) and at the end of summer (September/October), corresponding to the nadir and peak of vitamin D status, respectively. At both time points, serum concentration of 25(OH)D was quantified by liquid chromatography-tandem mass spectrometry, FFM (kg) was measured using bioelectrical impedance and muscle strength (kg) was measured using handgrip dynamometry. QoL was assessed using the validated St George's Respiratory Questionnaire.
RESULTS:
Mean±SD 25(OH)D concentration was significantly higher at the end of summer compared to the end of winter (52.5±30.5 nmol/L vs 33.7±28.4 nmol/L, P<0.001); and house- bound patients had significantly lower 25(OH)D concentration compared to nonhousebound patients at the end of summer (42.9±4.2 vs 57.2±9.9 nmol/L; P⩽0.001). Muscle strength (at both time points) and QoL (end of summer only) were positively predicted by 25(OH)D concentration, independent of age, sex and smoking status.
CONCLUSION:
This study highlights the need for health policies to include a recommendation for year-round vitamin D supplementation in housebound COPD patients , and wintertime supplementation in nonhousebound patients, to maintain optimal 25(OH)D concentrations to protect musculoskeletal health. Furthermore, an optimal vitamin D status may have potential benefits for QoL in these patients.
COPD Review at JAMA- Feb 2019
COPD = 3.2% of all physician office visits annually
COPD is 4th leading cause of death (126 000 deaths per year).
COPD 75% due to smoke, atmospheric pollution
COPD self reported by 6.4% of the US population
COPD perhaps 29 million - Despite self-reported data, most with airflow obstruction have never been diagnosed
The word VITAMIN does not occur once in the JAMA review
📄 Download the PDF from VitaminDWiki
Future Impact of Various Interventions on the Burden of COPD in Canada:
A Dynamic Population Model - 2012
📄 Download the PDF from VitaminDWiki
