Metastatic Cancer probably reduced by vitamin D - many studies
Stage IV Cancer appears to be the same as Metastatic Cancer
Cancers can spread to bone if low Vitamin D, poor VDR or poor CYP24A1 - Nov 2022
Bone Metastases of Diverse Primary Origin Frequently Express the VDR (Vitamin D Receptor) and CYP24A1
J. Clin. Med. 2022, 11(21), 6537; https://doi.org/10.3390/jcm11216537
Active vitamin D (1,25(OH)D3) is known to exert direct anti-cancer actions on various malignant tissues through binding to the vitamin D receptor (VDR). These effects have been demonstrated in breast, prostate, renal and thyroid cancers, which all have a high propensity to metastasise to bone. In addition, there is evidence that vitamin D catabolism via 24-hydroxylase (CYP24A1) is altered in tumour cells, thus, reducing local active vitamin D levels in cancer cells. The aim of this study was to assess VDR and CYP24A1 expression in various types of bone metastases by using immunohistochemistry. Overall, a high total VDR protein expression was detected in 59% of cases (39/66). There was a non-significant trend of high-grade tumours towards the low nuclear VDR expression (p = 0.07). Notably, patients with further distant metastases had a reduced nuclear VDR expression (p = 0.03). Furthermore, a high CYP24A1 expression was detected in 59% (39/66) of bone metastases. There was a significant positive correlation between nuclear VDR and CYP24A1 expression (p = 0.001). Collectively, the VDR and CYP24A1 were widely expressed in a multitude of bone metastases, pointing to a potential role of vitamin D signalling in cancer progression. This is of high clinical relevance, as vitamin D deficiency is frequent in patients with bone metastases.
📄 Download the PDF from VitaminDWiki
VitaminDWiki - Cancers might alter CYP24A1 gene
{include}
Cancer spreads via leaky blood vessels, vitamin D reduces leaks
"In cancer, tumors need to create new vessels in order to continue to grow, but the vessels they create are often leaky, allowing tumor cells to penetrate into the circulation and metastasize to other parts of the body." 2015
Significance of Blood Vessel Leakiness in Cancer - 2002 FREE PDF
Chemo Creates Leaky Blood Vessels Helping Cancer Cells To Spread - 2021
Supposedly inactive form of vitamin D3 may actually reduce blood vessel leakage – Oct 2015 VitaminDWiki
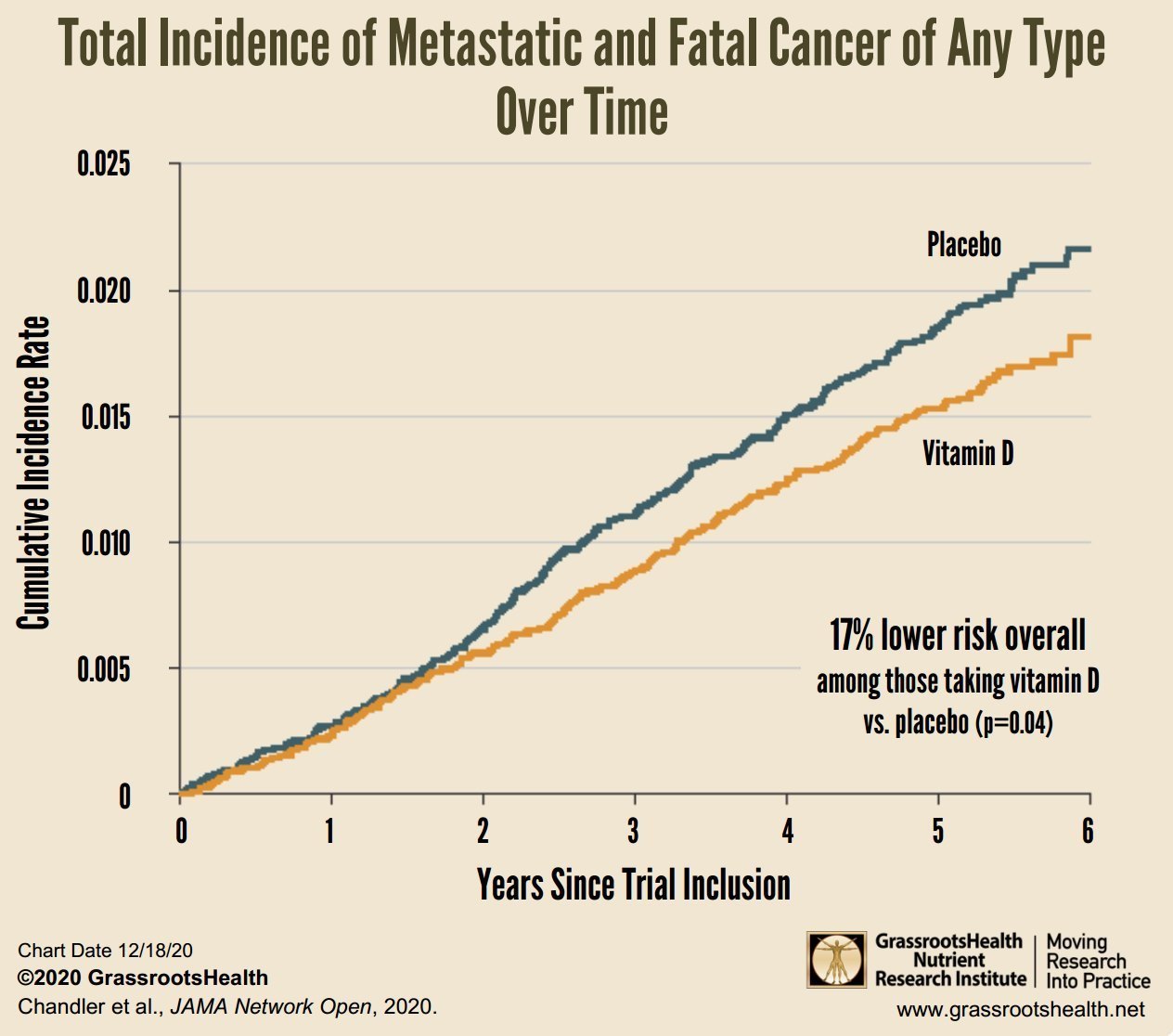
17% less risk of metastatic cancer with just 2,000 IU daily Vitamin D - GRH Oct 2022
Lower Rates of Metastatic Cancer and Cancer Death with Vitamin D - GrassrootsHealth
Only a fraction of the blog post is on metastatic cancer
Started wondering about vitamin D and metastases after reading the following article in 2010
Only 5 percent of cancer research funds are spent on metastases, yet it kills 90 percent of all cancer patients
June 1, 2010
On average, about five percent of total cancer research funding is spent on investigating metastases (the spread of cancer cells around the body) in Europe, yet metastatic disease is the direct or indirect cause of 90 percent of all cancer deaths, according to an editorial in the European Journal of Cancer (EJC). { appears to have been in European Journal of Cancer Volume 46, Issue 7, Pages 1177-1290 May 2010: Stopping Cancer in its Tracks: Metastasis as a Therapeutic Target }
The authors of the editorial, which introduces a special EJC issue on metastasis ("Stopping cancer in its tracks: metastasis as a therapeutic target"), highlight this discrepancy in funding and they believe that, although it is difficult to obtain accurate figures, the situation is probably similar in other countries such as the USA and Japan.
It has been known for some time that metastasis is the key problem in cancer and the main reason why people die from the disease. Until recently, the reasons why some people developed metastases and other did not had been unclear, but, as this special issue of the EJC shows, at last there are models and scientific hypotheses that have begun to unravel this process and the EJC reviews the state of the art in this respect. However, research into metastasis has not necessarily attracted the recognition it deserves from funding organisations.
Professor Jonathan Sleeman, one of the two guest editors of the EJC special issue and head of microvascular pathobiology research at the University of Heidelberg (Germany), said: "Metastasis is a process in cancer that is very poorly understood; it kills patients and therefore we believe that it should be funded better. Yet at the European level and, indeed, worldwide, comparatively little emphasis is placed on tackling metastases and in providing appropriate levels of funding for research."
He continued: "Given the clinical importance of metastasis for cancer patients, the limited treatment options for metastatic disease and the open question of how metastasis works, we need to know how much research funding is being directed at the problem and what proportion of funding for cancer research ends up focused on metastases? I have found it hard to obtain reliable figures, but although there is considerable variation between European countries, I estimate that the average spent on metastasis research is around 5% of total cancer research funding. Given that metastasis is of central importance to the prognosis and outcome of cancer patients, we could argue that in many countries more funding should be directed toward metastasis research."
Metastasis is the process by which cancer cells split off from the original, primary tumour and travel to other parts of the body via the blood or lymph systems. This leads to the growth of secondary tumours in places such as the bones, brain, lungs and liver, and it is usually these that end up killing the patient.
"Metastatic disease, therefore, represents a major public health problem, affecting cancer patients and their families, as well as health care systems and the broader economy. Despite this, progress in developing treatments for metastatic disease remains slow," write Prof Sleeman and the second guest editor, Professor Patricia Steeg (chief of the Women's Cancers Section, Laboratory of Molecular Pharmacology at the National Cancer Institute, Bethesda, USA) in their editorial.
In addition to adequate funding, they call for:
effective translational research for metastatic disease, which will take discoveries made in the laboratory quickly into new and better treatments for cancer patients;
clinical trials to be designed so that they include information on metastases;
clinicians and scientists to work more closely together to design clinical trials that assess the development of new metastases.
"In summary, combating metastasis formation and growth is the key to successfully treating cancer," they conclude. "Traditional growth control approaches are inadequate and can even be detrimental in the long term: new therapies built upon a solid understanding of the process of metastatic disease are urgently required. In turn, this demands an increased pre-clinical knowledge base that capitalises on major conceptual advances made in recent years, as well as a rational approach to the design of clinical trials with the inclusion of metastasis as an end-point. Together these observations speak for the necessity of increasingly close interactions between basic and clinical scientists, as well as the enhanced levels of research funding required to alleviate this major clinical problem."
The EJC special issue on metastasis consists of a number of articles looking at the state of current knowledge about the disease and outlining promising areas of research. Prof Steeg said: "We hope that this special issue will highlight the fact that metastasis should be an important consideration during drug development. If more attention was paid to it, we could really improve treatments for cancer patients."
More information: "Cancer metastasis as a therapeutic target" by Jonathan Sleeman and Patricia S. Steeg. European Journal of Cancer. Volume 46, issue 7, pages 1177-1180 (May 2010).
Provided by ECCO-the European CanCer Organisation
VitaminDWiki - Breast Cancers with the lowest Vitamin D levels were more likely to metastasize – Sept 2022
12+ VitaminDWiki pages have METASTATIC OR METASTASIZE OR METASTASIS in the title
This list is automatically updated
{LIST()}
Vitamin D Deficiency Masquerading as Metastatic Cancer: A Case Series - 2009
The American Journal of the Medical Sciences: April 2009 - Volume 337 - Issue 4 - pp 245-247; doi: 10.1097/MAJ.0b013e3181898525
Clinical Investigation
Khokhar, Jawaad S. MD; Brett, Allan S. MD; Desai, Ami MD
Patients with vitamin D deficiency can present with nonspecific bone pain and findings on radionuclide bone scanning that may suggest metastatic malignancy. In this report, we present 4 such cases, in which clinicians initially pursued diagnoses of metastatic malignancy and did not consider vitamin D deficiency and osteomalacia in the differential diagnosis. Eventual recognition of vitamin D deficiency and provision of supplementation resulted in prompt resolution of symptoms for each patient. In appropriate cases, timely consideration of a diagnosis of vitamin D deficiency can mitigate the anxiety associated with undergoing an evaluation for cancer.
Vitamin D May Reduce Prostate Cancer Metastasis by Several Mechanisms Including Blocking Stat3 - 2008
(American Journal of Pathology. 2008;173:1589-1590.)
© 2008 American Society for Investigative Pathology DOI: 10.2353/ajpath.2008.080579
Correspondence: William B. Grant, Sunlight, Nutrition, and Health Research Center, San Francisco, CA
This correspondence relates to "Stat3 promotes metastatic progression of prostate cancer (AmJPathol 2008, 172:1717–1728)."
To the Editor-in-Chief:
The recent article by Abdulghani and colleagues1 in reporting that Stat3 promotes metastatic progression of prostate cancer opens the door to new approaches to fight this cancer. This letter proposes that vitamin D might be beneficial in reducing the risk of prostate cancer mortality by inhibiting the action of Stat3.
Solar UVB and vitamin D have long been hypothesized to reduce the risk of prostate cancer mortality.2 Whereas solar UVB is correlated with increased survival for those diagnosed with prostate cancer,3 serum 25-hydroxyvitamin D (calcidiol) measured 1 to 8 years before detection of prostate cancer generally does not show a significant correlation with incidence, although higher calcidiol levels are significantly correlated with more aggressive forms of prostate cancer.4 These findings suggest that vitamin D is more effective at reducing metastasis than progression of prostate cancer. Similar results have been found for many other cancers, based on the dependence of cancer survival on season in Norway5 and that solar UVB is more highly correlated with cancer mortality rates than cancer incidence rates for many cancers in the United States.6
Laboratory studies with the hormonal metabolite of vitamin D, 1,25-dihydroxyvitamin D (calcidiol), indicate that calcidiol might be effective in combating prostate cancer. One study found that calcitriol inhibits the synthesis and actions of pro-inflammatory prostaglandins by three mechanisms.7 Another study identified calcitriol as a negative regulator of androgen inactivation in prostate cancer LNCaP cells.8 With respect to Stat3, it was reported that in vitro treatment of activated T cells with calcidiol inhibited the interleukin-12-induced tyrosine phosphorylation of Stat3.9 Several studies have reported that inhibiting phosphorylation of Stat3 impairs the role of Stat3 in carcinogenesis. In one study, decreased phosphorylation decreased induction of Stat3 target genes and increased apoptosis10 ; in another, decreased phosphorylation decreased transforming growth factor-?-mediated invasion and metastasis in pancreatic cancer cells.11
To date the beneficial role of calcidiol in reducing the risk of death from prostate cancer3 is stronger than that of calcitriol.12 Prostate cells express vitamin D-25-hydroxylase (25-OHase) and can convert calcidiol to calcitriol.13 Thus, making sure that those diagnosed with prostate cancer have high calcidiol levels might be appropriate.
In conclusion, the findings by Abdulghani and colleagues1 might help to explain the benefit of vitamin D in increasing the survival rate for prostate cancer, and the findings by Muthian and colleagues9 might help lead to a therapeutic way to reduce the role of Stat3 in leading to metastasis of prostate cancer.
Footnotes; WBG receives funding from the UV Foundation (McLean, VA), the Vitamin D Society (Canada), and the European Sunlight Association.
References
Abdulghani J, Gu L, Dagvadorj A, Lutz J, Leiby B, Bonuccelli G, Lisanti MP, Zellweger T, Alanen K, Mirtti T, Visakorpi T, Bubendorf L, Nevalainen MT: Stat3 promotes metastatic progression of prostate cancer. Am J Pathol 2008, 172:1717-1728[Abstract/Free Full Text]
Schwartz GG, Hulka BS: Is vitamin D deficiency a risk factor for prostate cancer? (Hypothesis). Anticancer Res 1990, 10:1307-1311[Medline]
Lagunova Z, Porojnicu AC, Dahlback A, Berg JP, Beer TM, Moan J: Prostate cancer survival is dependent on season of diagnosis. Prostate 2007, 67:1362-1370[CrossRef][Medline]
Ahn J, Peters U, Albanes D, Purdue MP, Abnet CC, Chatterjee N, Horst RL, Hollis BW, Huang WY, Shikany JM, Hayes RB: Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial Project Team: serum vitamin D concentration and prostate cancer risk: a nested case-control study. J Natl Cancer Inst 2008, 100:796-804[Abstract/Free Full Text]
Porojnicu AC, Dahlback A, Moan J: Sun exposure and cancer survival in Norway: changes in the risk of death with season of diagnosis and latitude. Adv Exp Med Biol 2008, 624:43-54[Medline]
Boscoe FP, Schymura MJ: Solar ultraviolet-B exposure and cancer incidence and mortality in the United States, 1993–2002. BMC Cancer 2006, 6:264[CrossRef][Medline]
Krishnan AV, Moreno J, Nonn L, Swami S, Peehl DM, Feldman D: Calcitriol as a chemopreventive and therapeutic agent in prostate cancer: role of anti-inflammatory activity. J Bone Miner Res 2007, 22(Suppl 2):V74-V80
Kaeding J, Bélanger J, Caron P, Verreault M, Bélanger A, Barbier O: Calcitrol (1alpha,25-dihydroxyvitamin D3) inhibits androgen glucuronidation in prostate cancer cells. Mol Cancer Ther 2008, 7:380-390[Abstract/Free Full Text]
Muthian G, Raikwar HP, Rajasingh J, Bright JJ: 1,25 Dihydroxyvitamin-D3 modulates JAK-STAT pathway in IL-12/IFNgamma axis leading to Th1 response in experimental allergic encephalomyelitis. J Neurosci Res 2006, 83:1299-1309[CrossRef][Medline]
Herrmann A, Vogt M, Mönnigmann M, Clahsen T, Sommer U, Haan S, Poli V, Heinrich PC, Müller-Newen G: Nucleocytoplasmic shuttling of persistently activated STAT3. J Cell Sci 2007, 120:3249-3261[Abstract/Free Full Text]
Zhao S, Venkatasubbarao K, Lazor JW, Sperry J, Jin C, Cao L, Freeman JW: Inhibition of STAT3 Tyr705 phosphorylation by Smad4 suppresses transforming growth factor beta-mediated invasion and metastasis in pancreatic cancer cells. Cancer Res 2008, 68:4221-4228[Abstract/Free Full Text]
Beer TM, Ryan CW, Venner PM, Petrylak DP, Chatta GS, Ruether JD, Redfern CH, Fehrenbacher L, Saleh MN, Waterhouse DM, Carducci MA, Vicario D, Dreicer R, Higano CS, Ahmann FR, Chi KN, Henner WD, Arroyo A, Clow FW: ASCENT Investigators: double-blinded randomized study of high-dose calcitriol plus docetaxel compared with placebo plus docetaxel in androgen-independent prostate cancer: a report from the ASCENT Investigators. J Clin Oncol 2007, 25:669-674[Abstract/Free Full Text]
Flanagan JN, Young MV, Persons KS, Wang L, Mathieu JS, Whitlatch LW, Holick MF, Chen TC: Vitamin D metabolism in human prostate cells: implications for prostate cancer chemoprevention by vitamin D. Anticancer Res 2006, 26:2567-2572[Abstract/Free Full Text]
High vitamin D levels and improved quality of life in a patient with metastatic colorectal cancer: case report.- 2009
Tenn Med. 2009 Oct;102(10):37-8.
Miller CW, Marino A, Moukharskaya J, Peiris AN.
Division of Endocrinology, Department of Internal Medicine, Mountain Home VA Medical Center, East Tennessee State University, Johnson City, TN, USA. cwt-miller@yahoo.com.br
Promise of vitamin D analogues in the treatment of hyperproliferative conditions.- 2006
Mol Cancer Ther. 2006 Apr;5(4):797-808.
Masuda S, Jones G.
Department of Biochemistry, Queen's University, Kingston, Ontario, Canada K7L 3N6.
1Alpha,25-dihydroxyvitamin D3 [1alpha,25-(OH)2D3; calcitriol] is best known as a hormone involved in calcium homeostasis but is also a potent antiproliferative agent in many cell types, particularly epithelial cells. 1Alpha,25(OH)2D3 mediates its actions through a classic steroid hormone-like transcriptional mechanism by influencing the expression of hundreds of genes. Effects of 1alpha,25(OH)2D3 have been observed on expression of cell cycle regulators, growth factors and their receptors, apoptotic machinery, metastatic potential, and angiogenesis; all of which have some effect on hyperproliferative conditions. This minireview focuses on the anticancer potential of 1alpha,25(OH)2D3 and its analogues by summarizing the promising data from animal and human trials of 1alpha,25(OH)2D3 and some of the more interesting synthetic vitamin D analogues in the treatment of a variety of different animal cancer models and in human patients with advanced cancer. Optimal administration of vitamin D analogues is only just being achieved with high-dose intermittent administration overcoming bioavailability and hypercalcemia problems and combination therapy with cytotoxic agents (taxols and cisplatins), antiresorptive agents (bisphosphonates), or cytochrome P450 inhibitors being attempted. Although the potential of vitamin D as an antiproliferative drug has been realized in the treatment of psoriasis and in parathyroid cell hyperplasia associated with secondary hyperparathyroidism, the search for an anticancer treatment incorporating a vitamin D analogue remains elusive.
Low serum levels of vitamin D in metastatic cancer patients: a case–control study -2014
Medical Oncology volume 31, Article number: 861 (2014) https://doi.org/10.1007/s12032-014-0861-3
Ahmet Taner Sümbül, Ahmet Sezer, Gamze Kavvasoğlu, Celal Yücel Batmacı, Erhan Yengil, Abdullah Erman Yağız, İlhami Gültepe, Hüseyin Abalı, İhsan Üstün & Cumali Gökçe
Accompanying comorbidities observed during the cancer treatment usually affect the course and outcome of the therapy. Hypovitaminosis D, which is one of these conditions, is a resolvable problem, if recognized. In this study, we investigated whether the serum 25(OH)D levels of the patients who were presented to our outpatient clinic were different from the serum levels of the healthy population living in the same area. Our study included 90 patients who were presented to the Medical Oncology outpatient clinic and 90 age, gender, body mass index and ethnic origin matched controls without a known disease, who were presented to the outpatient clinics of the Departments of Internal Diseases and Family Medicine for routine controls. Blood count tests, detailed biochemistry tests (including serum levels of Cr, Ca and P), measurement of serum 25(OH)D levels and C-reactive protein were performed in serum samples of all of the patients and controls. Mean serum levels of 25(OH)D were 13.5 ng/ml (SD 5.1) in all cancer patients, 13.1 ng/ml (SD 4.2) in the patients who were presented for adjuvant therapy, 13.8 ng/ml (SD 5.5) in the patients who were presented at metastatic stage and 18.4 ng/ml (SD 12.5) in the controls. Mean serum CRP levels were 5.4 mg/dl (SD 1.2) in the control group, 8.4 mg/dl (SD 4.3) in the adjuvant therapy group and 20.3 (SD 16.8) in the patients with metastatic disease.
Generally, all cancer patients (p 0.003) and the patients with metastatic cancer (p 0.004) had lower serum 25(OH)D levels compared to controls, and there was an inverse correlation between serum 25(OH)D and CRP levels in patients with metastatic cancer (p 0.036). In metastatic cancer patients, hypovitaminosis D may be a comorbidity and it is recommended to consider during initial evaluation and follow-up. Because it might improve these patients quality of life and chemotherapy adherence.11
Vitamin D Supplementation and Survival in Metastatic Colorectal Cancer - March 2017 (2,000 IU not help)
Nutrition and Cancer https://doi.org/10.1080/01635581.2018.1445766
Background: Some studies have demonstrated that higher baseline plasma levels of 25-hydroxivitamin D [25(OH)D] are associated with a significant reduction in colorectal cancer (CRC) incidence. Patients with metastatic CRC (mCRC) tend to be vitamin D insufficient, but the effect of vitamin D on the survival of mCRC patients still remains uncertain. In this study, we evaluated the association between cholecalciferol 2,000 IU daily supplementation and survival of mCRC patients.
Methods: Seventy-two patients with mCRC were included. Seventy-one patients with 25(OH)D levels <75 nmol/l were randomized to receive standard chemotherapy or standard chemotherapy with cholecalciferol 2,000 IU daily. The primary endpoint was overall survival (OS) and the secondary endpoint was progression-free survival (PFS). The follow-up period was 46 mo.
Results: All but one patient (98.6%) was vitamin D insufficient. There was no statistically significant difference in OS or PFS between those who received vitamin D supplements and controls.
Conclusions: The majority of patients with mCRC are vitamin D insufficient at the time of diagnosis. In our study, adding 2,000 IU of cholecalciferol daily for 2 yr to standard chemotherapy did not show any benefit in OS or PFS.
Metastatic Cancers deaths reduced by Vitamin D (2,000 IU daily) plus Omega-3 - Nov 2020
Effect of Vitamin D3 Supplements on Development of Advanced Cancer A Secondary Analysis of the VITAL Randomized Clinical Trial
"In this randomized clinical trial, supplementation with vitamin D reduced the incidence of advanced (metastatic or fatal) cancer in the overall cohort, with the strongest risk reduction seen in individuals with normal weight."
https://doi.org/doi:10.1001/jamanetworkopen.2020.25850 FREE PDF
Risk of metastatic cancer reduced 73% by high-intensity exercise (which increases vitamin D to cells) Nov 2022
An Exercise-Induced Metabolic Shield in Distant Organs Blocks Cancer Progression and Metastatic Dissemination
https://doi.org/10.1158/0008-5472.CAN-22-0237 FREE PDF
https://VitaminDWiki.com/Intense+exercise+increases+vitamin+D+receptor+activation
The lingering mysteries of metastatic recurrence in breast cancer - Nov 2020
British Journal of Cancer volume 124, pages13–26 (2021) https://doi.org/10.1038/s41416-020-01161-4 FREE PDF
Alessandra I. Riggio, Katherine E. Varley & Alana L. Welm
Despite being the hallmark of cancer that is responsible for the highest number of deaths, very little is known about the biology of metastasis. Metastatic disease typically manifests after a protracted period of undetectable disease following surgery or systemic therapy, owing to relapse or recurrence. In the case of breast cancer, metastatic relapse can occur months to decades after initial diagnosis and treatment. In this review, we provide an overview of the known key factors that influence metastatic recurrence, with the goal of highlighting the critical unanswered questions that still need to be addressed to make a difference in the mortality of breast cancer patients.
