Thyroid Cancer 1.4 X higher risk if low vitamin D– meta-analysis
Risk of thyroid cancer increases 1.5 X times if Vitamin D deficient - meta-analysis June 2024
Association between vitamin D status and thyroid cancer: a meta-analysis
Front Nutr. 2024 Jun 18:11:1423305. doi: 10.3389/fnut.2024.1423305
Yue Hu # 1 2, Chongxiang Xue # 3 4, Shumeng Ren 2, Lishuo Dong 5, Jiaqi Gao 1 6, Xiuyang Li 1
Background: Cumulative evidence has suggested that vitamin D deficiency is related with an increased susceptibility to various types of cancers. However, the association between vitamin D and thyroid cancer (TC) has remained to be unknown. Thus, there has been an urgent need for a meta-analysis to summarize existing evidence on vitamin D levels and the risk of TC.
Objective: This meta-analysis aimed to figure out the association between vitamin D level and the risk of TC.
Methods: A systematic search was performed for eligible articles on the association between vitamin D and TC based on PubMed, Embase, Web of Science, Cochrane, and ClinicalTrials.gov. Outcomes were the vitamin D level of cases with TC and the incidence of vitamin D deficiency in cases with TC comparing with the controls. The effect measures included standardized mean difference (SMD), ratio of means (RoM), and odds ratio (OR). A dose-response meta-analysis was performed to assess the correlation between vitamin D level and the risk of TC. Subgroup analyses and meta-regressions were conducted to explore the source of heterogeneity. And publication bias was evaluated through Begg's and Egger's tests.
Results: Results of the meta-analysis revealed lower levels of vitamin D in TC cases comparing with those in control [SMD = -0.25, 95% CI: (-0.38, -0.12); RoM = 0.87, 95% CI: (0.81, 0.94)] and the levels of 1,25 (OH)D in cases with TC were also lower than controls [SMD = -0.49, 95% CI: (-0.80, -0.19); RoM = 0.90, 95% CI: (0.85, 0.96)].
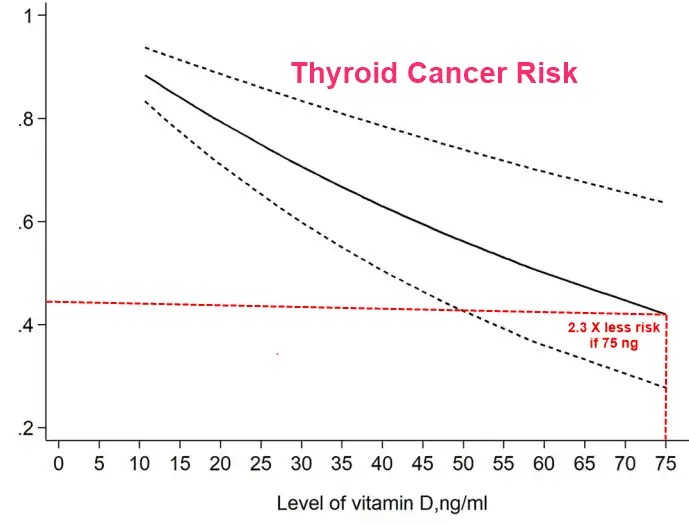
And vitamin D deficiency was associated with the increased risk of TC [OR = 1.49, 95% CI: (1.23, 1.80)]. Additionally, results from the dose-response meta-analysis showed that there is a 6% increase in the risk of TC for each 10 ng/ml decrease in 25 (OH)D levels [OR = 0.94; 95% CI: (0.89, 0.99)].
Conclusions: Individuals with TC had lower levels of vitamin D compared to controls, and vitamin D deficiency was correlated with an increase risk of TC.
📄 Download the PDF from VitaminDWiki
Thyroid Cancer outcomes greatly improved with Vitamin D supplementation – Aug 2023
Systematic vitamin D supplementation is associated with improved outcomes and reduced thyroid adverse events in patients with cancer treated with immune checkpoint inhibitors: results from the prospective PROVIDENCE study
Cancer Immunol Immunother . 2023 Aug 28. doi: 10.1007/s00262-023-03522-3
Melissa Bersanelli # 1 2, Alessio Cortellini # 3 4, Alessandro Leonetti 1 2, Alessandro Parisi 5, Marcello Tiseo 1 2 6, Paola Bordi 1, Maria Michiara 1, Simona Bui 1, Agnese Cosenza 1, Leonarda Ferri 1, Giulia Claire Giudice 1 6, Irene Testi 1 6, Elena Rapacchi 1, Roberta Camisa 1, Bruno Vincenzi 7, Giuseppe Caruso 1, Antonio Natale Rauti 6, Federica Arturi 6, Marco Tucci 8, Valentina Santo 7, Valentina Ricozzi 7, Vanessa Burtet 9, Paolo Sgargi 10, Renata Todeschini 2, Fable Zustovich 11, Luigia Stefania Stucci 12, Daniele Santini 13, Sebastiano Buti 1 2 6

Background: Hypovitaminosis D can have a negative prognostic impact in patients with cancer. Vitamin D has a demonstrated role in T-cell-mediated immune activation. We hypothesized that systematic vitamin D repletion could impact clinical outcomes in patients with cancer receiving immune-checkpoint inhibitors (ICIs).
Methods: We planned a prospective observational study (PROVIDENCE) to assess serum vitamin D levels in patients with advanced cancer receiving ICIs (cohort 1 at treatment initiation, cohort 2 during treatment) and the impact of systematic repletion on survival and toxicity outcomes. In an exploratory analysis, we compared the clinical outcomes of cohort 1 with a control cohort of patients followed at the participating centers who did not receive systematic vitamin D repletion.
Results: Overall, 164 patients were prospectively recruited in the PROVIDENCE study. In cohort 1, consisting of 101 patients with 94.1% hypovitaminosis (≤ 30 ng/ml) at baseline, adequate repletion with cholecalciferol was obtained in 70.1% at the three months re-assessment. Cohort 2 consisted of 63 patients assessed for vitamin D at a median time of 3.7 months since immunotherapy initiation, with no patients having adequate levels (> 30 ng/ml). Even in cohort 2, systematic supplementation led to adequate levels in 77.8% of patients at the three months re-assessment. Compared to a retrospective control group of 238 patients without systematic vitamin D repletion, PROVIDENCE cohort 1 showed longer overall survival (OS, p = 0.013), time to treatment failure (TTF, p = 0.017), and higher disease control rate (DCR, p = 0.016). The Inverse Probability of Treatment Weighing (IPTW) fitted multivariable Cox regression confirmed the significantly decreased risk of death (HR 0.55, 95%CI: 0.34-0.90) and treatment discontinuation (HR 0.61, 95%CI: 0.40-0.91) for patients from PROVIDENCE cohort 1 in comparison to the control cohort. In the context of longer treatment exposure, the cumulative incidence of any grade immune-related adverse events (irAEs) was higher in the PROVIDENCE cohort 1 compared to the control cohort. Nevertheless, patients from cohort 1 experienced a significantly decreased risk of all grade thyroid irAEs than the control cohort (OR 0.16, 95%CI: 0.03-0.85).
Conclusion: The PROVIDENCE study suggests the potential positive impact of early systematic vitamin D supplementation on outcomes of patients with advanced cancer receiving ICIs and support adequate repletion as a possible prophylaxis for thyroid irAEs.
Download the PDF from VitaminDWiki
Italian Guidelines for Vitamin D supplementation in hospital (clipped from PDF)
At enrollment, vitamin D supplementation was systematically offered to patients starting within 28 days from the assessment, following the guidelines of the Italian Society of Osteoporosis, Mineral Metabolism, and Bone Disease (SIOMMMS [18]) as follows:
Adequate level group: no supplementation.
Insufficiency group: cholecalciferol (vitamin D3) at the loading dose of 300,000 International Units (IU) over 4 weeks, maintenance dose of 820 IU daily.
Deficiency group: cholecalciferol at the loading dose of 600,000 International Units (IU) over 4 weeks, maintenance dose of 1000 IU daily.
Severe deficiency group: cholecalciferol at the loading dose of 1,000,000 International Units (IU) over 4 weeks, maintenance dose of 2000 IU daily.
- Comment by VitaminDWiki: loading dose seems correct, maintenance doses are too small
Association between vitamin D deficiency and risk of thyroid cancer: a case-control study and a meta-analysis - Feb 2018
J Endocrinol Invest. 2018 Feb 20. doi:10.1007/s40618-018-0853-9
Hu MJ1, Zhang Q1, Liang L1, Wang SY2, Zheng XC2, Zhou MM1, Yang YW1, Zhong Q1, Huang F3.
PURPOSE: Although vitamin D is reportedly associated with various cancers, the association between vitamin D and thyroid cancer is indefinite. We aimed to investigate whether this association applies to thyroid cancer (TC).
METHODS:
A total of 276 Chinese Han people were recruited in a current matched case-control study. Multivariable conditional logistic regression was computed to estimate the association between plasma 25(OH)D and papillary thyroid cancer (PTC). In addition, we searched relevant studies in PubMed and Web of Science databases before December 2017 to conduct a meta-analysis.
RESULTS:
In our case-control study, plasma 25(OH)D concentration was inversely associated with PTC risk (highest tertile vs lowest tertile: adjusted OR = 0.25; 95% CI 0.10, 0.61; Ptrend = 0.003). This association was independent of body mass index and physical activity (all adjusted Pinteraction > 0.05).
A total of 11 studies were included in the meta-analysis, among which ten studies have been published and one was our case-control study. Compared with 25(OH)D non-deficient group, the pooled OR of TC was 1.42 (95% CI 1.17, 1.73) in the deficient group. Similarly, blood 25(OH)D levels in patients with TC were tend to be lower than those in the controls (SMD = - 0.20, 95% CI - 0.36, - 0.03).
CONCLUSIONS: A high level of circulating 25(OH)D was associated with a decreased TC risk. This association has important significance in public health and should, therefore, be further studied.
Vitamin D-Related Genes and Thyroid Cancer—A Systematic Review - Nov 2022 (no associations found)
Int. J. Mol. Sci. 2022, 23(21), 13661; https://doi.org/10.3390/ijms232113661
by Adam Maciejewski and Katarzyna Lacka
Department of Endocrinology, Metabolism and Internal Diseases, Poznan University of Medical Sciences, 60355 Poznan, Poland
Vitamin D, formerly known for its role in calcium-phosphorus homeostasis, was shown to exert a broad influence on immunity and on differentiation and proliferation processes in the last few years. In the field of endocrinology, there is proof of the potential role of vitamin D and vitamin D-related genes in the pathogenesis of thyroid cancer—the most prevalent endocrine malignancy. Therefore, the study aimed to systematically review the publications on the association between vitamin D-related gene variants (polymorphisms, mutations, etc.) and thyroid cancer. PubMed, EMBASE, Scopus, and Web of Science electronic databases were searched for relevant studies. A total of ten studies were found that met the inclusion criteria.
Six vitamin D-related genes were analyzed (
VDR—vitamin D receptor,
CYP2R1—cytochrome P450 family 2 subfamily R member 1,
CYP24A1—cytochrome P450 family 24 subfamily A member 1,
CYP27B1—cytochrome P450 family 27 subfamily B member 1,
DHCR7—7-dehydrocholesterol reductase and
CUBN—cubilin).
Moreover, a meta-analysis was conducted to summarize the data from the studies on VDR polymorphisms (rs2228570/FokI, rs1544410/BsmI, rs7975232/ApaI and rs731236/TaqI). Some associations between thyroid cancer risk (VDR, CYP24A1, DHCR7) or the clinical course of the disease (VDR) and vitamin D-related gene polymorphisms were described in the literature. However, these results seem inconclusive and need validation. A meta-analysis of the five studies of common VDR polymorphisms did not confirm their association with increased susceptibility to differentiated thyroid cancer. Further efforts are necessary to improve our understanding of thyroid cancer pathogenesis and implement targeted therapies for refractory cases
📄 Download the PDF from VitaminDWiki
VitaminDWiki - Thyroid Cancer rate has increased 3X in 3 decades, Vitamin D Receptor decreases, Calcium increases – Aug 2017
VitaminDWiki: Cancer- Other category with THYROID in title (7 as of Oct 2022)
This list is automatically updated
{LIST()}
