IVF 4X more successful for white women with lots of vitamin D – many studies
Note: This page needs to be merged with In vitro fertilization and Vitamin D – many studies
Summary of IVF and Vitamin D - Perplexity AI PRO Feb 2025
Does increasing vitamin D levels in both the man and women decrease the need for IVF?
Use the attached file and the web
Vitamin D plays a significant role in fertility for both men and women,
potentially reducing the need for IVF treatments through several mechanisms:
Impact on Natural Fertility
For Women:
Each 1 ng increase in blood vitamin D levels increases fertility by 1% [VDW-IVF]
Women with sufficient vitamin D levels (>30 ng/mL) show significantly higher rates of natural conception [VDW-IVF]
Vitamin D deficiency is found in 67-85% of women with fertility issues 8
For Men:
Vitamin D increases fertility in men by improving sperm quality and motility [VDW-IVF]
Calcium deficiency associated with low vitamin D can affect sperm motility and fertilization 5
IVF Success Rates
When IVF is needed, vitamin D status significantly impacts outcomes:
Clinical Evidence:
White women with sufficient vitamin D levels are 4X more likely to achieve pregnancy through IVF [VDW-IVF]
Live birth rates are 1.7X higher in vitamin D replete women undergoing IVF [VDW-IVF]
Women with sufficient vitamin D levels show 52.5% clinical pregnancy rates compared to 34.7% in those with insufficient levels [VDW-IVF]
Cost Considerations
The financial implications are substantial:
IVF costs at least $10,000 per cycle [VDW-IVF]
Vitamin D supplementation costs approximately $5 [VDW-IVF]
43% of US insurance plans do not cover any part of IVF treatment [VDW-IVF]
Recommendations
Before Pursuing IVF:
Both partners should achieve vitamin D sufficiency (>30 ng/mL) several months before attempting conception [VDW-IVF]
Supplementation should be maintained throughout the conception process [VDW-IVF]
Regular monitoring of vitamin D levels is recommended to maintain optimal fertility [VDW-IVF]
This evidence suggests that addressing vitamin D deficiency in both partners could potentially improve natural fertility and reduce the need for expensive IVF treatments.
Perplexity includes link to the following 14 minute YouTube video made in 2024
Don’t Miss Out on the Power of Vitamin D for Your Fertility and Immune Health? Dr Lora Shahine
[VDW-IVF] =📄 PDF of this VitaminDWiki page before the Perplexity summary
Are there any studies on the impact of vitamin D levels on male fertility
Multiple studies have investigated the relationship between vitamin D and male fertility, revealing complex and sometimes contradictory findings:
Clinical Evidence
Impact on Sperm Quality
Vitamin D supplementation shows a positive effect on sperm motility, particularly progressive motility 1 2
Men with vitamin D deficiency demonstrate significantly lower sperm motility compared to those with normal levels 1
Higher vitamin D levels correlate with better sperm morphology, though the relationship isn't always statistically significant 8
Pregnancy Outcomes
In a study of 330 vitamin D-deficient men with fertility issues, those receiving vitamin D supplementation had higher natural pregnancy rates (7.3%) compared to the placebo group (2.4%) 7
Men with oligozoospermia who received vitamin D supplementation showed nearly double the live birth rates (35.6%) compared to the placebo group (18.3%) 8
Biological Mechanisms
Testicular Function
Vitamin D receptors and metabolizing enzymes are present in various reproductive tissues, including Sertoli cells, germ cells, and Leydig cells 6
The testicular tissue can synthesize and degrade vitamin D independently from systemic vitamin D metabolism 6
Hormonal Effects
Evidence regarding vitamin D's impact on testosterone levels remains inconclusive 2
Vitamin D may influence fertility through calcium homeostasis in reproductive tissues 6
Recent Findings
A 2024 study presents contrasting evidence:
No significant association was found between vitamin D levels and male infertility or seminal fluid parameters 3
The study recommends larger multi-center investigations for more definitive conclusions 3
Laboratory Evidence
Animal studies support vitamin D's role in fertility:
Male rats with vitamin D deficiency showed 45-55% decreased successful mating rates 4
Vitamin D-deficient males exhibited lower testicular and epididymal sperm counts 4
Studies demonstrate vitamin D's involvement in ATP synthesis and sperm motility through the cAMP/PKA pathway 4
See also VitaminDWiki
Infertility treatment needs to achieve at least 30 ng of vitamin D – May 2019
Assisted Reproduction – 5 studies concluded vitamin D repletion helps – Review March 2015
Each 1 ng increase in blood level of vitamin D increases clinical pregnancy by 6%
Overview Conception and vitamin D
Vitamin D increases fertility of BOTH the man and the woman.
Each 1 ng increase in blood level of vitamin D increases fertility by 1%.
How 60 ng of vitamin D enabled pregnancy - a personal story in VitaminDWiki
Vitamin D and fertility and birth problems with dark skin – Jan 2011
Vitamin D and fertility: a systematic review – May 2012 which includes the following graphic
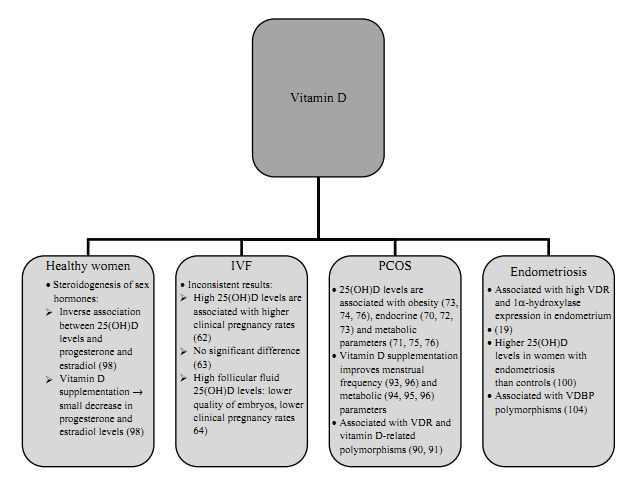
15 VitaminDWiki pages with IVF or IN VITRO FERTILIZATION in title
This list is automatcially updated
{LIST()}
IVF cycle 8X less successful if low vitamin D (Middle East) – Feb 2025
Vitamin D status, polymorphisms, and clinical outcomes in couples undergoing assisted reproductive technologies: exploring the role of 25(OH)D levels
Middle East Fertility Society Journal Volume 30, article number 1, (2025)
Rana Jreij, Rania Jounblat, Youmna Mrad, Elie Hajj Moussa, Maria Abdallah, Chadi Fakih, Fadia Najjar & Aline Hamade
Purpose
Vitamin D status has been recognized as an important factor in human health, and its relevance in the context of couples utilizing assisted reproductive technologies is of particular interest.
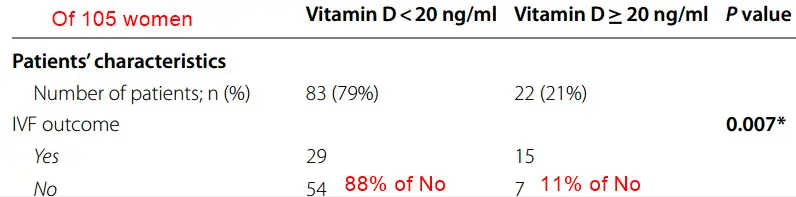
Methods
This study aimed to assess the levels of 25(OH)D by ELISA in the biological fluids (serum, semen, and follicular fluid) of 105 couples undergoing in vitro fertilization or intracytoplasmic sperm injection. Additionally, the association among 3 vitamin D receptor polymorphisms (Apa1, Fok1, and Taq1) and vitamin D status, as well as the clinical pregnancy rate after in vitro fertilization, were investigated.
Results
The results revealed a high rate of hypovitaminosis in the women’s group. Furthermore, a significant difference was observed in the fertilization rate (P = 0.007). Correlations were found between Apa1 polymorphism and the number of collected oocytes (P = 0.014), the number of embryos (P = 0.001), the number of 2 pronuclear (P = 0.001), and the frequency of clinical pregnancies (P = 0.046). Additionally, correlations were found between Taq1 SNP and the number of embryos (P = 0.046) and the serum vitamin D level (P = 0.042). The Fok1 polymorphism showed correlations with semen concentration (P = 0.044) and clinical outcome (P = 0.032).
Conclusion
These results suggest the importance of systemic vitamin D for women prior to pregnancy. The findings emphasize the potential benefits of vitamin D supplementation in women before pregnancy and call for cautious interpretation of data regarding the impact of vitamin D on pregnancy.
📄 Download the PDF from VitaminDWiki
IVF perhaps 2X average more successful if 36 ng of Vitamin D - May 2024
Association Between Vitamin D Level and Clinical Outcomes of Assisted Reproductive Treatment: A Systematic Review and Dose-Response Meta-Analysis
Reproductive Endocrinology: Review
Chenhao Xu, Xinqi An, Xiumei Tang, Yunxiao Yang, Qi Deng, Quanling Kong, Ying Hu & Dongzhi Yuan
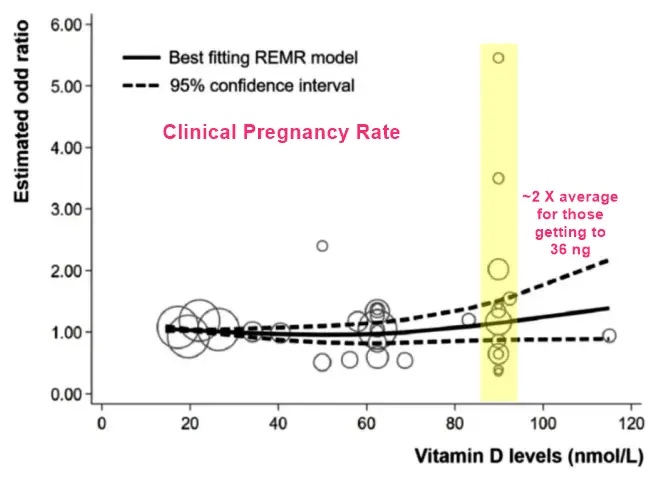
The investigation about association between vitamin D level and clinical outcomes of assisted reproductive treatment showed various outcomes. This study aimed to review the correlation between vitamin D and outcomes of assisted reproductive treatment. The search was registered on the PROSPERO database (CRD42023458040). PubMed, Embase, Medline, ClinicalTrials.gov, and Cochrane databases were searched up to July 2023. Twenty-three observational studies were selected for meta-analysis. Comparing groups with deficient and ‘insufficient + sufficient’ vitamin D level, meta-analysis showed positive correlation between clinical pregnancy rate and vitamin D (OR 0.81, 95%CI: 0.70, 0.95, P = 0.0001). Comparing groups with ‘deficient + insufficient’ and sufficient vitamin D level, meta-analysis showed positive correlation between vitamin D and clinical pregnancy rate (OR 0.71, 95%CI: 0.55, 0.91, P = 0.006), vitamin D and live birth rate (OR 0.69, 95%CI: 0.54, 0.89, P = 0.003). Subgroup analysis did not show the source of high heterogeneity. No correlation was found in biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate and implantation rate. In dose-response meta-analysis, a nonlinear association was found between vitamin D levels and outcomes when levels are below approximately 24 ng/L. The study shows that vitamin D level is associated with clinical pregnancy rate and live birth rate. Low vitamin D level does not influence biochemical pregnancy rate, ongoing pregnancy rate, miscarriage rate and implantation rate. Furthermore, 24 ng/L may be a possible threshold of vitamin D concentration in assisted reproduction therapy.
📄 Download the PDF from VitaminDWiki
43% of US insurances do not pay for any part of IVF - Sept 2023
- "Their data suggest that approximately 38% of patients who freeze eggs return to use them two to five years later."
VitaminDWiki suspects more IVF success if supplement both the man and the woman with Vitamin D months before the egg is made and, perhaps years later, for the mother months before the egg is transplanted
IVF women with good vitamin D were 1.7 X more likely to have a live birth - meta-analysis Aug 2020
Women’s vitamin D levels and IVF results: a systematic review of the literature and meta-analysis, considering three categories of vitamin status (replete, insufficient and deficient)
Human Fertility https://doi.org/10.1080/14647273.2020.1807618
Florina Iliuta,Jose Ignacio Pijoan,Lucía Lainz,Antonia Exposito &Roberto; Matorras

To investigate the influence of vitamin D status on in vitro fertilisation (IVF) results, a meta-analysis of 15 cohort studies of 3711 women undergoing IVF was performed. Women were classified into three groups according their vitamin D levels (≥30 ng/mL considered replete/sufficient; 21–29 ng/mL insufficient and <20 ng/mL deficient). Three different meta-analyses were performed: (i) sufficient vs deficient; (ii) sufficient vs ‘insufficient + deficient’; (iii) ‘sufficient + insufficient’ vs deficient. Comparing IVF outcomes in sufficient versus deficient groups (considering autologous and donor oocyte cycles together), we found women with
sufficient vitamin D had significantly higher
biochemical pregnancy (OR = 1.43 [1.06–1.95]),
ongoing pregnancy (OR = 1.29 [1.02–1.64]), and
live birth (OR = 1.74 [1.31–2.31]) rates,
with a non-significant trend to a higher clinical pregnancy rate (OR = 1.31 [0.94–1.82]), whereas implantation and miscarriage rates were similar. When the meta-analysis was restricted to autologous oocytes, the parameters which had been significant in the joint analysis remained significant, and differences in implantation (OR = 1.64, [1.17–2.29]) and clinical pregnancy (OR = 1.47 [1.2–1.69]) rates became significant. No significant differences were found when considering only cycles with donor oocytes. The sufficient + insufficient vs deficient and sufficient vs ‘insufficient + deficient’ comparisons identified significant differences in live birth rate. The meta-analysis shows that sufficient vitamin D status is associated with better outcomes in IVF. Nonetheless, there are many demographic, geographic and clinical parameters that may be related to vitamin D status that need to be ascertained before concluding that the better results are due to the higher levels of vitamin D.
📄 Download the PDF from VitaminDWiki
IVF 20-40% more succesful when eggs were collected in the summer - July 2023
IVF 4X more successful for white women with lots of vitamin D – Oct 2012
Characterizing the influence of vitamin D levels on IVF outcomes
Oxford Journals Medicine Human Reproduction Volume 27, Issue 11Pp. 3321-3327.
B. Rudick1,*, S. Ingles2,†, K. Chung3, F. Stanczyk3, R. Paulson3 and K. Bendikson3,†
1 Center for Women's Reproductive Health, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, Columbia University, 1790 Broadway 2nd Floor, New York, NY 10019, USA
2 Department of Preventative Medicine, Keck School of Medicine, University of Southern California, Los Angeles, CA 90033, USA
3 Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, University of Southern California, 2020 Zonal Avenue, Room 534, Los Angeles, CA 90033, USA
?*Correspondence address. E-mail: briana.rudick@gmail.com
Received August 29, 2011; Revision received June 13, 2012; Accepted June 21, 2012.
BACKGROUND Vitamin D plays a role in reproductive capacity. Recently, several investigators have demonstrated higher IVF pregnancy rates in vitamin D replete women. The objective of this study was to validate these findings and to further elucidate the role of vitamin D in reproduction among a diverse group of women.
METHODS This was a retrospective cohort study in an academic tertiary care center of 188 infertile women undergoing IVF. Serum levels of vitamin D (25OH-D) were measured in previously frozen serum samples. The main outcome measure was clinical pregnancy, defined as sonographic presence of a heartbeat following IVF.
RESULTS The relationship between vitamin D status and pregnancy rates differed by race (P < 0.01). Among non-Hispanic whites, pregnancy rates declined with progressively lower levels of vitamin D, while in Asians, the reverse was true. Adjusting for age and number and quality of embryos transferred among non-Hispanic whites, the odds of pregnancy were four times higher in vitamin D replete versus deficient patients . Live birth rates mirrored pregnancy rates. Vitamin D status was not associated with ovarian stimulation parameters or with markers of embryo quality.
CONCLUSIONS Vitamin D deficiency is associated with lower pregnancy rates in non-Hispanic whites, but not in Asians, possibly due to their lower IVF success rates . Vitamin D deficiency was not correlated with ovarian stimulation parameters or with markers of embryo quality, suggesting its effect may be mediated through the endometrium.
PDF is attached at the bottom of this page
Another study found In vitro fertilization 2X less successful if low vitamin D – Nov 2013
Influence of vitamin D levels on in vitro fertilization outcomes in donor-recipient cycles.
Fertil Steril. 2013 Nov 5. pii: S0015-0282(13)03154-3. doi: 10.1016/j.fertnstert.2013.10.008.
Rudick BJ, Ingles SA, Chung K, Stanczyk FZ, Paulson RJ, Bendikson KA.
Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility, Center for Women's Reproductive Health, Columbia University, New York, New York. Electronic address: briana.rudick@gmail.com.
OBJECTIVE: To elucidate the role of vitamin D in reproduction by examining the relationship between recipient vitamin D levels and pregnancy rates in donor-recipient IVF cycles.
DESIGN: Retrospective cohort study.
SETTING: Academic tertiary care center.
PATIENT(S): Ninety-nine recipients of egg donation at University of Southern California Fertility.
INTERVENTION(S): Serum was collected from egg donor recipients before ET and was tested for vitamin D levels [25(OH)D].
MAIN OUTCOME MEASURE(S): Clinical pregnancy as defined by sonographic presence of a heartbeat at 7-8 weeks of gestation.
RESULT(S): In a diverse population of 99 recipients (53% Caucasian, 20% Asian, 16% Hispanic, 7% African American), adjusted clinical pregnancy rates were lower among vitamin D-deficient recipients than among vitamin D-replete recipients ( 37% vs. 78% ).
Live-birth rates were 31% among vitamin D-deficient recipients, compared with 59% among vitamin D-replete recipients. There were no differences in adjusted clinical pregnancy and live-birth rates among recipients who were vitamin D deficient [25(OH)D<20 ng/mL] vs. among those who were vitamin D insufficient [20 ng/mL ≤ 25(OH)D<30 ng/mL].
CONCLUSION(S): Nonreplete vitamin D status [25(OH)D<30 ng/mL] was associated with lower pregnancy rates in recipients of egg donation. Since the oocyte donor-recipient model is able to separate the impact of vitamin D on oocyte vs. endometrium, these data suggest that the effects of vitamin D may be mediated through the endometrium.
References
Hewison M. Vitamin D and immune function: an overview. M Proc Nutr Soc. 2012;71:50–61
Ozkan S, Jindal S, Greenseid K, Shu J, Zeitlian G, Hickmon C, et al. Replete vitamin D stores predict reproductive success following in vitro fertilization. Fertil Steril. 2010;94:1314–1319 AbstractFull Text Full-Text PDF (278 KB)
Rudick B, Ingles S, Chung K, Stanczyk F, Paulson R, Bendikson K. Characterizing the influence of vitamin D levels on IVF outcomes. Hum Reprod. 2012;27:3321–3327
Porter RN, Smith W, Craft IL, Abdulwahid NA, Jacobs HS. Induction of ovulation for in vitro fertilization using buserelin and gonadotropins. Lancet. 1984;324:1284–1285
Oliviennes F, Fanchin R, Bouchard P, de Ziegler D, Taieb J, Selva J, et al. The single or dual administration of the gonadotropin-releasing hormone antagonist Cetrorelix in an in vitro fertilization–embryo transfer program. Fertil Steril. 1994;62:468–476
Hollis BW, Kamerud JQ, Selvaag SR, Lorenz JD, Napoli JL. Determination of vitamin D status by radioimmunoassay with an 125 I-labeled tracer. Clin Chem. 1993;39:529–533
Holick MF. Vitamin D deficiency: review. N Engl J Med. 2007;357:266–281
Hosmer DW, Lemeshow S. Goodness-of-fit tests for the multiple logistic regression model. Commun Stat. 1980;A9:1043–1069
Long JS, Freese J. 2006. Regression models for categorical dependent variables using Stata. Stata Press.
Vigano P, Lattuada D, Mangioni S, Ermellino L, Vignali M, Caporizzo E, et al. Cycling and early pregnant endometrium as a site of regulated expression of the vitamin D system. J Mol Endocrinol. 2006;36:415–424
Daftary GS, Taylor HS. Endocrine regulation of HOX genes. Endocr Rev. 2006;27:331–355
Evans KN, Nguyen L, Chan J, Innes BA, Bulmer JN, Kilby MD, et al. Effects of 24-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 on cytokine production by human decidual cells. Biol Reprod. 2006;75:816–822
Evans KN, Bulmer JN, Kilby MD, Hewison M. Vitamin D and placental-decidual function. J Soc Gynecol Investig. 2004;11:263–271
Tavakoli M, Jeddi-Tehrani M, Salek-Moghaddam A, Rajaei S, Mohammadzadeh A, Sheikhhasani S, et al. Effect of 1,25(OH)2 vitamin D3 on cytokine production by endometrial cells of women with recurrent spontaneous abortion. Fertil Steril. 2011;96:751–757 AbstractFull Text Full-Text PDF (660 KB)
Whitsett JA, Ho M, Tsang RC, Norman EJ, Adams KG. Synthesis of 1,25-dihydroxyvitamin D3 by human placenta in vitro. J Clin Endocrinol Metab. 1981;53:484–488
Barrera D, Avila E, Hernández G, Méndez I, González L, Halhali A, et al. Calcitriol affects hCG gene transcription in cultured human syncytiotrophoblasts. Reprod Biol Endocrinol. 2008;6:3
Barrera D, Avila E, Hernandez G, Halhali A, Biruete B, Larrea F, et al. Estradiol and progesterone synthesis in human placenta is stimulated by calcitriol. J Steroid Biochem Mol Biol. 2007;103:529–532
Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92:3517–3522
Should We Be Monitoring Vitamin D Levels In Our Infertile Patients? comment on the study
Clinical pregnancy 1.5 X more likely after IVF when vitamin D level > 30 ng - June 2013
Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization.
CMAJ Open. 2013 Jun 28;1(2):E77-82. doi: 10.9778/cmajo.20120032. eCollection 2013.
Garbedian K1, Boggild M2, Moody J3, Liu KE1.
1 Department of Obstetrics and Gynecology, Mount Sinai Hospital, University of Toronto, Toronto, Ont.
2 Faculty of Medicine, University of Toronto, Toronto, Ont.
3 Samuel Lunenfeld Research Institute, Mount Sinai Hospital, Toronto, Ont.
BACKGROUND:
Recent studies suggest that vitamin D may play a role in human reproduction. Our goal was to investigate whether vitamin D levels are predictive of implantation and clinical pregnancy rates in infertile women following in vitro fertilization (IVF).
METHODS:
We prospectively evaluated vitamin D status, as determined by serum 25-hydroxy-vitamin D (25[OH]D) levels, in a cohort of 173 women undergoing IVF at Mount Sinai Hospital, Toronto, Ontario. Serum 25(OH)D samples were collected within 1 week before oocyte retrieval. We classified patients as having sufficient (≥ 75 nmol/L) or insufficient (or deficient; hereafter referred to as "insufficient"; < 75 nmol/L) serum levels of 25(OH)D. We compared patient demographics and IVF cycle parameters between groups. The primary outcome measure was clinical pregnancy (intrauterine sac visible on ultrasound performed 4-5 weeks after embryo transfer).
RESULTS:
Of the included women, 54.9% had insufficient 25(OH)D levels and 45.1% had sufficient levels.
Women with sufficient levels had significantly higher rates of clinical pregnancy per IVF cycle started (52.5%) compared with women with insufficient levels (34.7%; p < 0.001).
Implantation rates were also higher in the sufficient 25(OH)D group, but the results were not statistically significant. Multivariable logistic regression analysis (adjusted for age, body mass index and day 5 [v. day 3] embryo transfer) showed that serum 25(OH)D level may be a predictor of clinical pregnancy (adjusted odds ratio 1.01, 95% confidence interval 1.00-1.03).
INTERPRETATION:
Our findings suggest that women with sufficient levels of vitamin D are significantly more likely to achieve clinical pregnancy following IVF. Vitamin D supplementation could provide an easy and cost-effective way of improving pregnancy rates; this merits further investigation.
Vitamin D levels NOT associated with IVF success - Sept 2014 (disagrees with all previous studies)
Impact of circulating levels of total and bioavailable serum vitamin D on pregnancy rate in egg donation recipients
Alberta Fabris, M.D.a, Alberto Pacheco, Ph.D.a, María Cruz, Ph.D.a, Jose Manuel Puente, M.D.a, Human Fatemi, M.D.b, Juan A. Garcia-Velasco, M.D., Ph.D.a, ,
a IVI-Madrid, Rey Juan Carlos University, Madrid, Spain
b Nova IVI Fertility, Abu Dhabi, United Arab Emirates
Objective: To investigate the correlation between total and bioavailable serum 25-OH vitamin D and the pregnancy rate in recipients of donated oocytes.
Design: Retrospective study.
Setting: University-affiliated private IVF center.
Patient(s): A total of 267 patients who were referred to our clinic for oocyte donation from June 2013 to December 2013.
Intervention(s): Serum analysis of vitamin D and bioavailable vitamin D and reproductive outcomes.
Main Outcome Measure(s): Pregnancy and implantation rate.
Result(s):Among all patients, 15.3% (n = 41) were vitamin D replete (vitamin D >30 ng/mL), 50.2% (n = 134) had vitamin D deficiency (20–30 ng/mL), and 34.4% (n = 92) had insufficient vitamin D (<20 ng/mL). Implantation rates were similar among patients with normal, insufficient, or deficient total serum 25-OH vitamin D levels (61%, 63.4%, and 65.2%, respectively).
Pregnancy rates did not differ among the three groups (70%, 69.9%, and 73.9%).
Ongoing pregnancy rates were also comparable among the three groups (55.9%, 52.7%, and 60.7%).
The predictive value of total vitamin D regarding pregnancy rate was analyzed by the receiver operating characteristic curve, and the area under the curve (AUC) was 0.468.
The AUC for bioavailable 25-OH vitamin D was 0.499, showing that the analysis of the AUC for vitamin D or bioavailable vitamin D was not informative.
Conclusion(s): Vitamin D insufficiency and deficiency are frequent conditions in our southern European infertile population. In contrast to previous studies, patients who are not vitamin D replete do not have a decreased chance of becoming pregnant with egg donation.
Bioavailable 25-OH vitamin D, which is a better marker of the status than total 25-OH vitamin D, does not correlate with pregnancy rate in recipients of donated oocytes.
Thus, at this stage, there is insufficient evidence to recommend vitamin D screening in patients undergoing egg donation.
See also web
2X increase in stoke in 1 year after IVF treatments
in the month after giving birth: 37 strokes per 100,000 IVF related births
"About 2 percent of births in the United States involve infertility treatment of some kind, according to the paper."
Note: Decreased vitamin D is linked to both increased risk of strokes and increased need for infetility treatment
More details on the above information from Natural-Fertility-Info.com
60 second video on improving fertility of the women and the man with vitamin D
Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization CMAJ Open, June 2013
- 52% more likely to become pregnant if >25 ng than if < 25ng
- PDF is attached at the bottom of this page
- Vitamin D deficiency and infertility: insights from in vitro fertilization cycles Nov 2014
- 2.2X more likely to get pregnant if > 20 ng of vitamin D PDF is free to patients
