Vitamin D supplementation fights COVID-19 – 11th meta-analysis
Vitamin D supplementation, COVID-19 & Disease Severity: A meta-analysis
QJM . 2021 Jan 24;hcab009. doi: 10.1093/qjmed/hcab009
Komal Shah 1, Deepak Saxena 1, Dileep Mavalankar 1
Study from indian focused on Icu and mortality - discussion is at the bottom of this page
📄 Download the PDF from VitaminDWiki
Virus meta-analyses
{category}
Mortality and Virus studies
{category}
COVID-19 treated by Vitamin D - studies, reports, videos
{include}
Discussion:
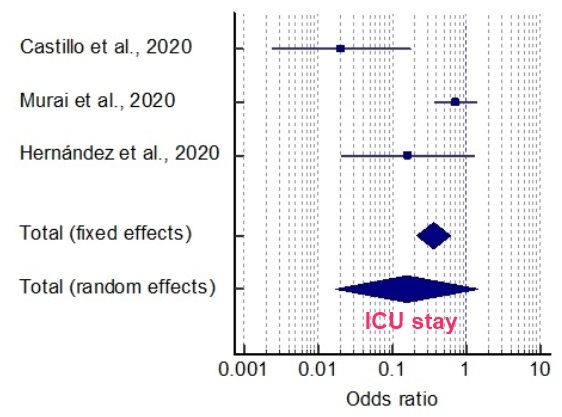
To the best of our knowledge this is the first meta-analysis that synthesized cumulative evidences assessing impact of vitamin D supplementation on intensive care needs and mortality in hospitalized COVID-19 patients. It was observed that as compared to conventional care, vitamin D reduces severity of the disease; however, the results regarding improving mortality statistics could not reach to a statistically significant conclusion.
1. 1
The first study conducted by Castillo et al.16 randomized 76-consecutive hospitalized COVID-19 patients in intervention to control group in ratio of 2:1 in Spain. The patients in the intervention arm received soft capsules of calcifediol (0.532 mg) on the day of admission through oral route and continued with the oral calcifediol (0.266 mg) on day 3, 7, and then weekly until discharge or ICU admission. Whereas the patients in the control arm followed the standard treatment protocol with combination of hydroxychloroquine (400 mg every 12 h on the first day, and 200 mg every 12 h for the following 5 days), azithromycin (500 mg orally for 5 days). Though baseline characteristics of patients in both the arms were matched, controls were more hypertensive (57.69% vs 24.19%; p=0.002). To adjust the effect of the confounders such as hypertension and diabetes, authors applied multivariate logistic regression analysis and found that the lower probability of ICU admission in intervention still remained significant [odds ratio=0.03 (95 % CI: 0.003- 0.25)] as compared to control. Similarly, the mortality rates were also lower in patients treated with calciferol, however it could not reach to a statistically significant level possibly due to extremely lower number of patients with adverse outcome. However, authors also acknowledged potential confounding effect of obesity and pre-existing deficiency of vitamin D as limitation of study. They recommended need of more extensive research with appropriately matched arms.
1. 2
A double-blind, randomized, placebo-controlled trial in Brazil conducted by Murai et al.,17 showed an effect of a single dose of 200,000 IU of vitamin D3 supplementation to hospital stay in severely ill COVID-19 patients. During the trial, 240 patients were equally randomized either in vitamin D supplementation or placebo arm. The baseline demographic and clinical characteristics were comparable between both the arms. Though the supplementation was found to be safe and it improved serum 25-hydroxyvitamin D levels, it did not translate into any clinical benefits to the patient in the form of reduced hospital stay, the requirement of ICU support or mortality rate. Hence the authors recommended against the use of vitamin D as adjuvant therapy in hospitalized COVID patients. Though it was found that requirement of oxygen therapy was low in patients treated with vitamin D as compared to placebo group (65.5% vs 85.9%; p=0.008). Removal of this study from overall analysis resulted in lowering of heterogeneity in cumulative findings of metaanalysis and yielded beneficiary effect on ICU needs with vitamin D.
1. 3
Hernandez et al.,18 retrospectively assessed the role of vitamin D supplementation on 216 hospitalized COVID-19 positive patients in Spain. It was observed that 19 patients who were on vitamin D supplementation, had drastically low requirement of ICU care as compared to their counterparts (5.3% vs 25.4%), however similar to other studies there was no difference in mortality (10.5% vs 10.4%) between both the groups. The study also compared the serum levels of 25- hydroxyvitamin D in hospitalized COVID patients and compared it with the population-based controls of similar age and sex. It was found the patients had significantly low levels of serum 25- hydroxyvitamin D as compared to population based-controls even in the presence of main confounding factors. However, the observational nature of the study was accepted as one of the important limitations. One important finding emerged from the study was that unlike other reports there was no relationship between serum 25-hydroxyvitamin D levels and the parameters of COVID-19 severity, such as ICU admission, the need for mechanical ventilation, or mortality. This might be due to smaller number of events in the groups. However, it also highlights the need to assess Vit D supplementation's effect in a prospective manner using the randomized controlled trial study design.
1. 4
SHADE study19, a randomized controlled trial assessed effect of high-dose vitamin D supplementation (60 000 IU of cholecalciferol - oral nano-liquid droplets) on 21-days recovery in COVID-19 patients. The authors found that greater proportion of vitamin D-deficient individuals with SARS-CoV-2 infection turned COVID-19 negative with a significant decrease in fibrinogen on high-dose cholecalciferol supplementation. However, they did not assess the role of supplementation on ICU requirement and mortality and hence were not included in the current meta-analysis.
Despite this heterogeneity among the studies, cumulative findings of the meta-analysis favored vitamin D supplementation for reduction of COVID-19 severity. However, more trials are required to substantiate the findings on other outcomes, especially community based and in-hospital trials should also be conducted in developing countries to assess potential of vitamin D supplementation in reducing hospitalization-, ICU- and ventilation needs and mortality rates.
