Most people with Long-Haul COVID-19 have low Vitamin D
Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection
Nutrients 2021, 13(7), 2430; https://doi.org/10.3390/nu13072430
by Liam Townsend 1,2,*OrcID,Adam H. Dyer 3OrcID,Patrick McCluskey 4,Kate O’Brien 5,Joanne Dowds 5,Eamon Laird 3,6OrcID,Ciaran Bannan 1,2,Nollaig M. Bourke 3,Cliona Ní Cheallaigh 1,2OrcID,Declan G. Byrne 2,4OrcID andRose Anne Kenny 6,7
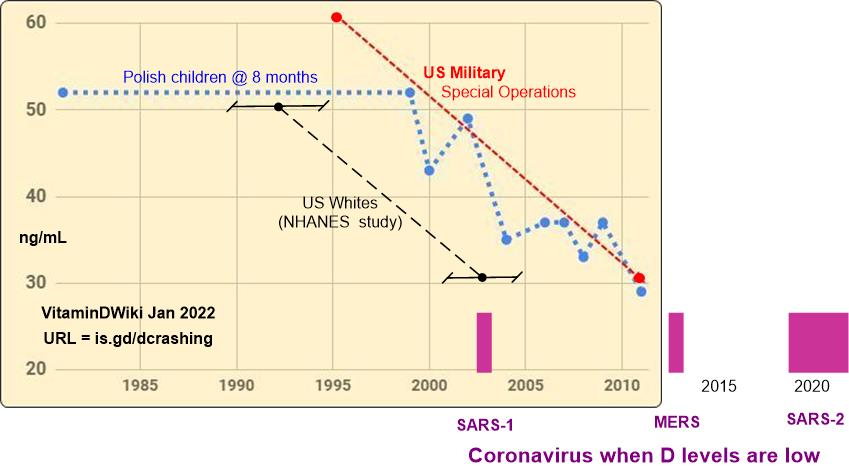 Click on chart for details
1. Pages in both of the categories Virus and Vitamin D Receptor:
{category}
The risk of 44 diseases at least double with poor Vitamin D Receptor as of Oct 2019
{FONT(size="18")}Omega-3, Magnesium, Zinc, Quercetin, non-daily Vit D, Curcumin, intense exercise, Ginger, Essential oils, etc{FONT} Note: The founder of VitaminDWiki uses 10 of the 12 known VDR activators__
1. See "long-haul" in VitaminDWiki titles
{LIST()}
Click on chart for details
1. Pages in both of the categories Virus and Vitamin D Receptor:
{category}
The risk of 44 diseases at least double with poor Vitamin D Receptor as of Oct 2019
{FONT(size="18")}Omega-3, Magnesium, Zinc, Quercetin, non-daily Vit D, Curcumin, intense exercise, Ginger, Essential oils, etc{FONT} Note: The founder of VitaminDWiki uses 10 of the 12 known VDR activators__
1. See "long-haul" in VitaminDWiki titles
{LIST()}
📄 Download the PDF from VitaminDWiki
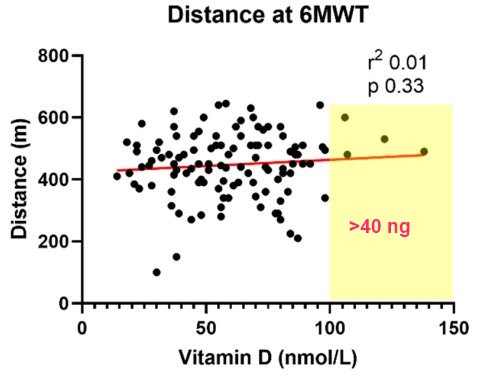
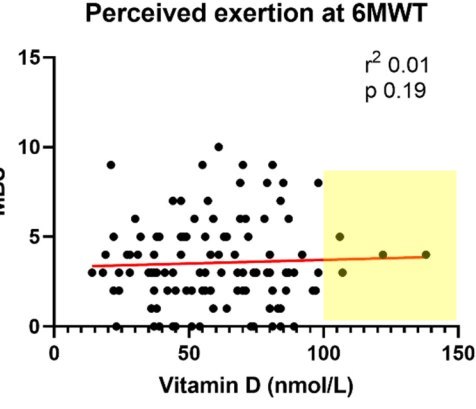
The emergence of persistent symptoms following SARS-CoV-2 infection, known as long COVID, is providing a new challenge to healthcare systems. The cardinal features are fatigue and reduced exercise tolerance. Vitamin D is known to have pleotropic effects far beyond bone health and is associated with immune modulation and autoimmunity. We hypothesize that vitamin D levels are associated with persistent symptoms following COVID-19. Herein, we investigate the relationship between vitamin D and fatigue and reduced exercise tolerance, assessed by the Chalder Fatigue Score, six-minute walk test and modified Borg scale. Multivariable linear and logistic regression models were used to evaluate the relationships. A total of 149 patients were recruited at a median of 79 days after COVID-19 illness. The median vitamin D level was 62 nmol/L, with n = 36 (24%) having levels 30–49 nmol/L and n = 14 (9%) with levels <30 nmol/L. Fatigue was common, with n = 86 (58%) meeting the case definition. The median Borg score was 3, while the median distance covered for the walk test was 450 m. No relationship between vitamin D and the measures of ongoing ill-health assessed in the study was found following multivariable regression analysis. These results suggest that persistent fatigue and reduced exercise tolerance following COVID-19 are independent of vitamin D.
