Aging of the Immune system (Immunosenescence): micronutrients and gut microbiota
Nutrition, Immunosenescence, and Infectious Disease: An Overview of the Scientific Evidence on Micronutrients and on Modulation of the Gut Microbiota
Adv Nutr . 2022 Oct 2;13(5):S1-S26. doi: 10.1093/advances/nmac052.
Philip C Calder 1 2 , Edwin Frank Ortega 3 , Simin N Meydani 3 , Yuriko Adkins 4 5 , Charles B Stephensen 4 5 , Brice Thompson 6 , Heather Zwickey 7

The immune system is key to host defense against pathogenic organisms. Aging is associated with changes in the immune system, with a decline in protective components (immunosenescence),
increasing susceptibility to infectious disease, and a
chronic elevation in low-grade inflammation (inflammaging),
increasing the risk of multiple noncommunicable diseases.
Nutrition is a determinant of immune cell function and of the gut microbiota. In turn, the gut microbiota shapes and controls the immune and inflammatory responses. Many older people show changes in the gut microbiota. Age-related changes in immune competence, low-grade inflammation, and gut dysbiosis may be interlinked and may relate, at least in part, to age-related changes in nutrition. A number of micronutrients ( vitamins C, D, and E and zinc and selenium ) play roles in supporting the function of many immune cell types. Some trials report that providing these micronutrients as individual supplements can reverse immune deficits in older people and/or in those with insufficient intakes. There is inconsistent evidence that this will reduce the risk or severity of infections including respiratory infections.
Probiotic, prebiotic, or synbiotic strategies that modulate the gut microbiota, especially by promoting the colonization of lactobacilli and bifidobacteria, have been demonstrated to modulate some immune and inflammatory biomarkers in older people and, in some cases, to reduce the risk and severity of gastrointestinal and respiratory infections, although, again, the evidence is inconsistent. Further research with well-designed and well-powered trials in at-risk older populations is required to be more certain about the role of micronutrients and of strategies that modify the gut microbiota-host relationship in protecting against infection, especially respiratory infection.
Vitamin D section in the PDF
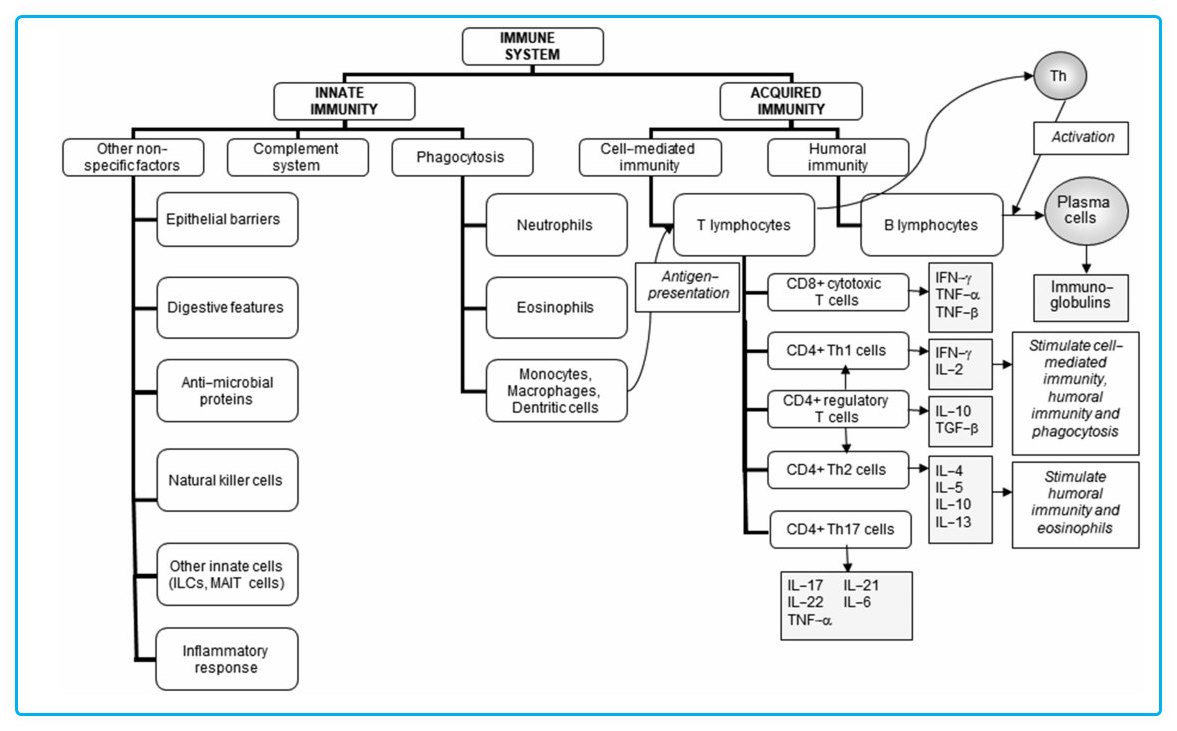
The precursor to the active form of vitamin D canbe acquired from the diet or be produced via UVB irradiation of the skin. Subsequent hydroxylation reactions involving the enzymes 25-hydroxylase and 1-a-hydroxylase, located in the liver and kidney, respectively, produce the active form, 1-a,25- dihydroxyvitamin D, also known as calcitriol. Some immune cells, including macrophages and dendritic cells, also express 1-a-hydroxylase activity, and so can produce calcitriol (106, 107). Calcitriol binds to the vitamin D receptor, which is a transcription factor acting to regulate cellular gene expression. Many immune cell types express the vitamin D receptor and respond to vitamin D, including dendritic cells, monocytes, macrophages, T cells, and B cells, and so vitamin D is now considered to also be an important regulator of immune function and inflammation (108-115).
Vitamin D enhances epithelial integrity and induces antimicrobial peptide (e.g., cathelicidin) synthesis in epithelial cells and macrophages (108, 116), directly enhancing host defense. The effects of vitamin D on the cellular components of immunity are rather complex. Vitamin D promotes differentiation of monocytes to macrophages and increases phagocytosis, superoxide production, and bacterial killing by innate immune cells (81). It also promotes antigen processing by dendritic cells, although antigen presentation may be impaired (117-119); this has been interpreted as a pro-tolerogenic role for vitamin D. Vitamin D is also reported to inhibit CD4+ and CD8+ T-cell proliferation and production of cytokines by Th1 lymphocytes and of antibodies by B lymphocytes (120-122), highlighting the paradoxical nature of its effects. Effects on Th2 responses are not clear, but vitamin D seems to increase the number of regulatory T lymphocytes (119, 123, 124). Incubation of human memory T cells with vitamin D promoted a switch from a proinflammatory to an anti-inflammatory phenotype (125). Incubation of blood mononuclear cells from older people with vitamin D resulted in higher IL-10 production in response to LPS (126). An RCT of a vitamin D analog in older adults (mean age: 73 y) reported an increase in LPS- induced production of IL-10 by isolated blood mononuclear cells, an increased ratio of CD4+ to CD8+ cells in the blood, and a decrease in the number of CD8+CD28- cells (127); LPS-induced production of IL-6 and IFN-y was not affected (127). A cross-sectional study identified that older men (but not women) who were replete in vitamin D had a lower risk of having very low NK activity, in comparison to older men with low vitamin D (128). Low-dose vitamin D (10 ug/d) in healthy adults (40-55 y) did not affect the blood regulatory T-cell population but attenuated the seasonal increase in IFN-y production by T cells (129). Several studies have investigated the association between vitamin D status and response to seasonal influenza vaccination, with inconsistent findings: a meta-analysis of 4 studies identified that vitamin D deficiency reduces seroprotection to the H3N2 and B components, but not to the H1N1 component, but has no effect on seroconversion to any of the components (130).
If vitamin D is needed to support the immune system, then vitamin D deficiency would lead to increased susceptibility to, and severity of, infectious disease. In the 19th and early 20th centuries it was found that cod liver oil and exposure to the sun helped treat tuberculosis (131), although the role of vitamin D itself was not immediately evident. Niels Ryberg Finsen was awarded the Nobel Prize for Medicine in 1903 for demonstrating the benefits of UV light to patients with tuberculosis of the skin—lupus vulgaris—which either cured or improved the disease in approximately 95% of patients (132), and by 1920, phototherapy was routinely used to treat pulmonary tuberculosis. While UV therapy can affect immune function in the skin, independent of the effect on vitamin D synthesis, these early studies had findings that are consistent with the later-demonstrated effects of vitamin D on immune function. Research in the early 21st century showed that TLR activation of macrophages upregulates the vitamin D receptor and vitamin D-1-a-hydroxylase genes, which, in turn, induce the expression of the antimicrobial peptide cathelicidin, which has activity against Mycobacterium tuberculosis (108, 116, 133). Furthermore, there is a positive relation between circulating vitamin D and cathelicidin, consistent with the idea that sufficient vitamin D status supports this antibacterial mechanism (134). Clinical trials have examined the efficacy of vitamin D intervention on treatment of tuberculosis, often using the rate of sputum conversion from a positive to a negative culture result as the key outcome, during the lengthy antimicrobial treatment period for patients with active pulmonary tuberculosis. In a meta-analysis of RCTs (135), high-dose vitamin D supplementation given after the initiation of antimicrobial treatment did not speed the recovery in patients infected with tuberculosis, but recovery was more rapid in those who were infected with the multidrug-resistant strains of M. tuberculosis where drug therapywould have been ineffective, thus allowing the benefit of vitamin D treatment to, perhaps, become more apparent.
Observational findings have linked low concentrations of vitamin D to increased risk of viral acute respiratory infection. For example, Berry et al. (136) described an inverse linear relation between serum 25-hydroxyvitamin D concentrations and respiratory tract infections in a crosssectional study of 6789 British adults. Similarly, data from the US Third NHANES, which included 18,883 adults, showed an independent inverse association between serum 25-hydroxyvitamin D and recent upper respiratory tract infection (URTI) (137). Other studies also reported that individuals with low vitamin D status have a higher risk of viral respiratory tract infections (138, 139). A recent metaanalysis of RCTs involving 48,488 participants (140) examined the relation between vitamin D supplementation and the prevention of acute respiratory infections and found a small, but significant, protective effect of daily administration of 400 to 1000 IU vitamin D taken for 12 mo or less against 1 or more acute respiratory infection compared with the placebo (OR: 0.70; 95% CI: 0.55, 0.89). Baseline vitamin D status was not associated with a protective benefit, although the authors speculated that the heterogeneity of the studies examined may have masked a potentially greater benefit for supplement use in those with vitamin D insufficiency or deficiency at baseline (140).
There has been significant interest in vitamin D and COVID-19 (141, 142). Numerous trials report associations between low vitamin D status and increased susceptibility to, and severity of, COVID-19 [e.g., (143)] and meta-analyses of such studies report that vitamin D deficiency is associated with increased risk of severe COVID-19, hospitalization with COVID-19, and mortality from COVID-19 [e.g., (144, 145)]. A prospective study from the UK Biobank involving 8297 adults who had COVID-19 test results and records of their use of vitamin D supplements, serum 25- hydroxyvitamin D, and a number of covariates found a 34% lower risk of COVID-19 infection associated with the habitual use of vitamin D supplements, although there was no association with baseline vitamin D status (146). One large-scale retrospective study suggests a possible role of vitamin D in suppressing CRP and proinflammatory cytokine production implicated during the cytokine storm in COVID-19 infections, thus reducing COVID-19 severity (147). A study in an Italian residential care home reported that a bolus of vitamin D reduced mortality from COVID-19 (147) in patients hospitalized with COVID-19 reduced COVID- 19 severity (e.g., need for intensive care unit admission, mortality) (149, 150), although not all such studies reported benefits from vitamin D (151). Further studies are needed to determine whether inadequate vitamin D status is associated with a higher risk of more severe COVID-19 and whether vitamin D can be used to reduce disease severity.
Vitamin D summary
Vitamin D has pleiotropic effects on immunity, but it does support many aspects of both innate and acquired immunity, promoting antibacterial and antiviral defenses while also promoting a pro-tolerogenic environment. Supplemental vitamin D seems to reduce the risk, and perhaps severity, of respiratory tract infections. The effects of vitamin D may be useful to prevent or reduce the severity of respiratory diseases in groups most at risk for severe disease, such as older adults, and/or those who have low concentrations of vitamin D; this is important since, globally, vitamin D intake and status are low, especially in older people (78, 79). Future work should aim to confirm or refute the proposed benefits of vitamin D on respiratory disease in older adults through conduct of well-designed and adequately powered studies. In terms of understanding the effects of supplemental vitamin D and in the design of trials, consideration should be given to the genetic polymorphisms found in the vitamin D binding protein and the vitamin D receptor, as they have been associated with respiratory disease outcomes (152-154), as well as sex-related differences in how vitamin D might affect immune responses (128,155).
📄 Download the PDF from VitaminDWiki
VitaminDWiki - studies in both categories Seniors and Immunity
This list is automatically updated
{category}
VitaminDWiki pages with MICROBIOTA in title (11 as of Oct 2022)
This list is automatically updated
{LIST()}
VitaminDWiki pages with PROBIOTICS in title (30 as of Sept 2022)
This list is automatically updated
{LIST()}
