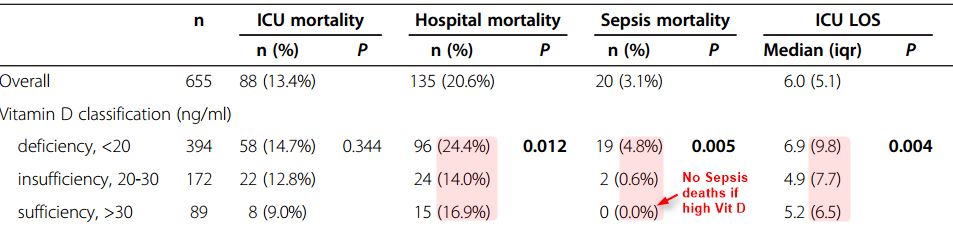
Increased Hospital, Sepsis deaths if low vitamin D
Vitamin D status and its association with season, hospital and sepsis mortality in critical illness.
Crit Care. 2014 Mar 24;18(2):R47. doi: 10.1186/cc13790.
Amrein K, Zajic P, Schnedl C, Waltensdorfer A, Fruhwald S, Holl A, Purkart T, Wünsch G, Valentin T, Grisold A, Stojakovic T, Amrein S, Pieber TR, Dobnig H.
📄 Download the PDF from VitaminDWiki
Subset of Table 3
INTRODUCTION:
Vitamin D plays a key role in immune function. Deficiency may aggravate the incidence and outcome of infectious complications in critically ill patients. We aimed to evaluate the prevalence of vitamin D deficiency and the correlation between serum 25-hydroxyvitamin D (25(OH) D) and hospital mortality, sepsis mortality and blood culture positivity.
METHODS:
In a single-center retrospective observational study at a tertiary care center in Graz, Austria, 655 surgical and nonsurgical critically ill patients with available 25(OH) D levels hospitalized between September 2008 and May 2010 were included. Cox regression analysis adjusted for age, gender, severity of illness, renal function and inflammatory status was performed. Vitamin D levels were categorized by month-specific tertiles (high, intermediate, low) to reflect seasonal variation of serum 25(OH) D levels.
RESULTS:
Overall, the majority of patients were vitamin D deficient (<20 ng/ml; 60.2%) or insufficient (≥20 and <30 ng/dl; 26.3%), with normal 25(OH) D levels (>30 ng/ml) present in only 13.6%. The prevalence of vitamin D deficiency and mean 25(OH) D levels was significantly different in winter compared to summer months (P <0.001). Hospital mortality was 20.6% (135 of 655 patients). Adjusted hospital mortality was significantly higher in patients in the low (hazard ratio (HR) 2.05, 95% confidence interval (CI) 1.31 to 3.22) and intermediate (HR 1.92, 95% CI 1.21 to 3.06) compared to the high tertile. Sepsis was identified as cause of death in 20 of 135 deceased patients (14.8%). There was no significant association between 25(OH) D and C-reactive protein (CRP), leukocyte count or procalcitonin levels. In a subgroup analysis (n = 244), blood culture positivity rates did not differ between tertiles (23.1% versus 28.2% versus 17.1%, P = 0.361).
CONCLUSIONS:
Low 25(OH) D status is significantly associated with mortality in the critically ill. Intervention studies are needed to investigate the effect of vitamin D substitution on mortality and sepsis rates in this population.
