Cholesterol, Vitamins D3 and K2, heart disease, sulfates, LDL, – Masterjohn Interview
Mercola interviewed Dr. Chris Masterohn
Video is 15 minutes long
Transcript follows
Update Nutritional Adjuncts to the Fat-Soluble Vitamins A, D, and K Mercola March 2013
eventually earning a reputation as “the most toxic of all the vitamins. still in textbooks in 2010
Zinc added to vitamin A greatly reduced conjunctiva of the eye
See also VitaminDWiki
Price and Masterjohn on Vitamin A Vitamin D and Vitamin K – 2010
Interactions of Vitamins D, A, and K, should measure calcitriol, calcification – Masterjohn Aug 2013
See also some Masterjohn Dec 2012 - Jan 2013
- Un Upcoming Plasma Marker of Blood Vessel Vitamin K Status Jan 2013
- MGP/Vitamin K test becoming available in 2013
- Beyond Good and Evil Dec 2012
- Dietary Nutrients;METHIONINE, B VITAMINS, GLYCINE; VITAMINS A, D AND K2;Magnesium; and has the following chart
Here is the 73+ minute transcript
PDF is attached at the bottom of this page
A Special Interview with Chris Masterjohn Jan 2013
By Dr. Joseph Mercola
DM : Dr. Joseph Mercola CJ : Chris Masterjohn Introduction:
DM : Welcome, everyone. This is Dr. Mercola, and today I'm joined by Chris Masterjohn, who has recently received his PhD in nutritional sciences from the University of Connecticut (so he's Dr. Masterjohn at this point). He's published five peer-reviewed papers on vitamins and supplementation, and he's currently researching fat-soluble supplements - A, D, and K - at the University of Illinois (in our backyard).
He also maintains a blog, The Daily Lipid, and his website, Cholesterol-And-Health.com (put some hyphens in there), and he is very active with the Weston A. Price Foundation.
So, welcome and thank you for joining us today.
CJ : Thank you so much for having me, Dr. Mercola.
DM : Congratulations on finally getting your PhD.
CJ : Thank you.
DM : That's quite an achievement for you. CJ : Quite a relief for me.
DM : I can imagine. Okay, today we're going to talk a little bit about cholesterol, which is a major source of a load of confusion. It's been demonized for very long, especially by the conventional medicine and Ancel Keys' flawed research in the early 50s. Every year people spend tens of billions of dollars on statin drugs, because they want to lower this "dangerous" molecule.
The Weston A. Price Foundation has been a major leader in helping people understand the truth on this topic and is one of the primary science resources. I was wondering if you could provide your take on this, because I know you have quite a few. I've seen you lecture on this before, and you do a really good job. I'd like to have you share with our audience your perspective on this and help them provide sort of a perspective and a frame to better understand this important topic.
CJ : Sure. Thank you so much for asking about cholesterol. It's one of my favorite topics. Yeah. You know, the state of sort of thinking about cholesterol in our country is a little bit weird. We even have Nobel Prize-winning researchers who call themselves "cholesterol warriors" and say that they're making a war on cholesterol, and it should strike us as a little odd. Why should we make a war on a molecule? Science is about the pursuit of truth. Medicine is about the pursuit of health. It's not about making wars on molecules.
If we want to understand why cholesterol is really an incredibly important molecule and is really our friend rather than our enemy, I think what we should look at is the question, "What happens without cholesterol?"
A perfect sort of natural experiment to look at that question would be to look at Smith-Lemli-Opitz syndrome or SLOS, which is a symptom of genetic deficiency in cholesterol. It's when people can't make enough cholesterol on their own. In order to actually have this full-blown syndrome, it's a recessive trait, which means you need a defective gene for cholesterol synthesis from your father, and you need one from your mother as well.
Now, the number of people who carry this gene in the population - the defective gene -is about one to three percent of the population. However, the number of babies who are born with Smith-Lemli-Opitz syndrome is far lower than we would expect. It's about I think one in 60, 000 babies who are born with Smith-Lemli-Opitz syndrome. So, why are so few babies born? Well, it turns out that if you have both of these genes and the unborn child can't synthesize its own cholesterol, then this usually results in spontaneous abortion.
Right away we see that cholesterol is needed for life itself and for simply a healthy pregnancy for the child to be born. In the rare cases, where someone...
DM : Let me just clarify a little bit.
CJ : Sure.
DM : Even though the gene is, say, one percent (just to I guess approximate the terms), because it's a recessive gene, you have to have one percent times one percent, so it would be one in 10,000 (you'd normally expect), but you see it one in 60,000.
CJ : Right. DM : Okay.
CJ : Right. You [wouldn't 04:14] expect one to three percent of babies to be born with it. But you'd expect a lot more babies than are actually born to have it.
DM : Right.
CJ : But we don't see that. That shows that the majority of cases where you have both genes, the baby is not born. So, cholesterol is essential for life.
When you do have a rare case where someone is born with Smith-Lemli-Opitz syndrome, you have a wide variety of defects in basically all the systems of the body. You have mental defects. You have failure to thrive. You have autism or mental retardation. You have physical defects in the hands, feet, and internal organs. You have increased susceptibility to infection. You have serious problems with digestion. You have visual problems.
What we're seeing is that cholesterol deficiency impacts almost every aspect of health. Why would that be? Well, as it turns out cholesterol is a very important molecule in the cell membrane. We're composed of trillions of cells. These cells all need to interact with each other. Cholesterol makes that happen. Cholesterol is the precursor to bile acids, which help us digest fatty substances. We need cholesterol in order to have proper digestion of our food.
Cholesterol plays a role especially in the brain. You know, our brain is only two percent of our body weight, but it has about 25 percent of our body's cholesterol. That's because cholesterol plays a critical role in synapse formation, which is the connection between neurons. This is what helps us think, what helps us form memories, and what helps us learn. All of these different processes in our body are dependent on cholesterol.
Also, if you look at the word "sterol" in cholesterol, that looks an awful lot like "steroid." All of our steroid hormones, our sex hormones, hormones that regulate our mineral status, our blood pressure, and so on. A lot of these hormones are steroid hormones, and all of the steroid hormones are made from cholesterol. Basically, what we want in our body is to.
DM : And vitamin D.
CJ : Oh, yup. Vitamin D is synthesized not from cholesterol, but from a very close relative of cholesterol.
DM : 7-dehydrocholesterol.
CJ : 7-dehydroxycholesterol. It's also very similar to the steroid hormones.
What we want is for cholesterol to be playing all these positive roles. That doesn't just mean we want a lot of cholesterol; it also means we want to metabolize it properly. We want to make cholesterol, so we can synthesize it into those bile acids and those sex hormones, so we can make vitamin D, and so we can make synapse formations in our brain.
Cholesterol is not our enemy; cholesterol is our friend. But things are in working order not just when cholesterol is there, but when cholesterol is being healthily used for all these great processes in our body.
DM : Terrific. Can you maybe expand on the reason why it's been so vilified, and how it may likely have stemmed from some of Ancel Keys' research and then have been picked and continued throughout the years?
CJ : Sure.
DM : I think that's the crux of the challenge. I mean it's just been demonized and vilified so regularly.
CJ : Yup. The vilification of cholesterol took a long time. Right now the mainstream paradigm is that heart disease and maybe some other diseases like stroke and other things that involve atherosclerosis and so on, but especially heart disease is caused by high levels of cholesterol in the blood.
Where did we get that idea? Well, it really goes back to the cholesterol-fed rabbit in 1913, which was a model of atherosclerosis that was published in Russia. They had found that feeding rabbits cholesterol would increase atherosclerosis, whereas all kinds of other means were tried to induce atherosclerosis in the rabbit and they didn't work.
Now, if you look at the writings of Nikolai Anichkov, who published that cholesterol-fed rabbit model, he never took that to mean that you could feed humans cholesterol and get atherosclerosis. He didn't take it as a dietary model. He saw that the rabbit was quite different. Of course, we all know that rabbits don't eat meat, eggs, and so on like we do. They eat grass and other vegetable products.
DM : They're herbivores, not even an omnivore. Pretty much what they only eat are plant products.
CJ : Sure. Right. Rabbits are very different from us dietarily. And it's not a model of human diet. In fact, in these experiments, enormous quantities of cholesterol are fed to the rabbits, and the rabbits would get blood cholesterol levels that would go far higher than anything you see in humans. But what Anichkov was looking at was he saw this as a model of some kind of defect in cholesterol metabolism.
Now, as time went on, this didn't really sort of reach into the mainstream and make everyone think that cholesterol was the cause of heart disease.
But as you mentioned, later on, we had research in the 1950s with Ancel Keys who came up with the diet-heart hypothesis. That connected diet to high cholesterol to heart disease and said people are consuming too much fat. What Ancel Keys had done was he did some epidemiological research, where he looked at countries. He said the countries where they have the highest fat intake, they have the highest risk of heart disease.
There were some problems with his research. Among them, he didn't look at all of the data, and the strength of the correlation is a lot weaker if he had taken all the data into account.
[-----10:00-----]
But really, the most important point is, correlation doesn't prove causation. And just because a country has a higher fat intake and a higher incidence of heart disease, doesn't mean necessarily that fat intake causes heart disease.
But there were also experiments in that same time frame in the 1950s, where they were showing that if they fed people milkshakes but they took out the fat from the milkshake and they put in their own fat. They kept the butter fat in. They put in coconut oil. They put in corn oil, or they out in, you know, any of these different kinds of oils. They showed that when the oils were more saturated (for example, animal products or tropical oils like coconut oil), cholesterol levels were higher. But if they were more unsaturated like vegetable oils (for example, corn oil), the cholesterol levels would be lower.
Over the course of the 1950s and going into the 1960s, you start to tie these different elements of research together, where people start saying, "Heart disease is caused by eating too much fat or too much saturated fat (that means the high cholesterol), and then that leads atherosclerosis. You die of a heart attack."
In 1957, the American Heart Association rejected this idea on the basis that it was too speculative.
They said look, you can't just show that your increasing or decreasing the level of cholesterol in the blood. If you want to show that making a dietary change causes changes in the risk of heart disease, you need to do a trial where people are randomized to either eat a diet high in fat or high in saturated fat, or eat a diet that's low in fat or saturated fat, and see if it actually changes how many people get heart disease, how many people get stroke, or how many people... You know, what actually happens to the people's health, not to the surrogate marker of cholesterol.
A few years later in 1961, the American Heart Association totally changed its tune. And it wasn't because any of those trials had been done. The state of the evidence didn't changed.
Well, what happened was, a few people who wrote the original report left the committee. A few people joined the committee. One of them was Ancel Keys. And the new committee wanted to write the report a little bit differently. They said if you have heart disease in your family, if you have high blood pressure, cholesterol, and other risk factors for heart disease, if you "live lives of sedentary and relentless frustration" (that's a direct quote), if you have any of these risk factors - you should begin getting rid of saturated fat in your diet, replacing it with these vegetable oils.
That was the real beginning of the actual mainstream acceptance of the idea. Then in 1984, there was a drug trial called the Coronary Primary Prevention Trial. This was a national trial. And this was testing cholestyramine, a cholesterol-lowering drug. This trial did show that the risk of heart disease was lower in people who have received the drug compared to placebo. Of course, total mortality and whether it actually benefitted people; the big picture is a totally different question. But it did show that the risk of heart disease was lowered.
This was widely popularized, especially on the cover of Time magazine, where they had that famous cover. I think it was in March of 1984 where they had the sad face, where the frowning mouth was made of bacon and the eyes were made of eggs. They said that, "Cholesterol is finally proven deadly. The American Heart Association has been right for all these years. We finally have the proof that vegetable oils need to replace animal fats. We need to get rid of the meat, the eggs, and all of these animal foods that we have valued for so long in our diet. And we finally have that proof."
The problem, of course, was that the Coronary Primary Prevention Trial didn't have any eggs in it. It didn't have any butter. It didn't have any bacon. It didn't have any of these foods. It was a drug. The question is, "Does the drug work the same way as the foods?" And there's no reason to believe that.
In fact, numerous trials were done trying to see if you could substitute polyunsaturated vegetable oils for traditional saturated animal fats. They were miserable, miserable failures, some indicating that doing so would even increase the risk of heart disease. One trial is especially disturbing that it seems to indicate that getting rid of animal fats and including vegetable oils might contribute to cancer. These studies were kind of swept under the rug. No one wants to look at them, because the drug trials look so much better.
Then, of course, they came out with the statins . As you know, I'm sure, and as most of your listeners probably know, statins are incredibly profitable. Now this idea that high cholesterol causes heart disease is basically turned into an incredibly profitable concept, because it's the foundation of the statin empire.
DM : Yes, indeed. Lipitor, in fact, (the results were just released; it's no surprise) is the number one selling drug of 2011. And then Crestor is number eight, I believe. The conclusion that was posted all over Time magazine and generally shared throughout the entire media that really contradicted what we now know to be true. At least, most knowledgeable people about health understand that these vegetable oils are, in fact, one of the primary reasons - especially the processed vegetable oils - that cause our health to decline.
When they can come out with such a profoundly contrary pronouncement of health, typically you would believe that there has to be some there has to be some really profound and powerful conflict of interest that promotes that type of pronouncement that's so unrelated to truth. In your evaluation review, have you been able to identify any of those sources that could lead them to such a tragically wrong conclusion? I'm sort of at a loss for words this morning.
CJ : Yup. Well, I think sociology is a little complicated. So is psychology. I don't think it's just about money. I think there are a few factors going on. One of them is simply we can often get very wedded to our own ideas. When we have an idea and we really like it, oftentimes that can obstruct our objectivity, just as much as a source of money could.
But at the same time, you know, if you look at the NIH Consensus Conference in 1984. That was sort of the conference, where it was finally decided for everyone and once and for all that cholesterol was the cause of heart disease. There were I think 13 main panel presentations. Most of them were by scientists.
One of them was by General Mills, about what the food industry would do to step in and assist in lowering everyone's cholesterol. You can imagine that General Mills was probably happy that people would start eating breakfast cereals instead of eggs for breakfast.
So, definitely there powerful interests who wanted to benefit from these ideas - the drug interest, the food industry, and just the people who believe this stuff. But you know, it's complicated, because if there were...This obviously hurts some industries, too, like it hurt the animal product industry, for example. I don't think we should sort of simplify it down to it's-all-who-has-the-most-money. But definitely a lot of people have made a lot of money on these ideas.
DM : Yeah. Certainly, that's true for the drug companies. There's no question. I can recall even since the newsletter that I put together has been published, there was a. I believe it was in the early 2000s, where they changed the healthy normal ranges of cholesterol. They lowered them, so that they would have a larger target market for their drugs.
Because when I started practicing in 1985 (I was concerned about cholesterol at that time largely because I was ignorant to a lot of these nutritional principles), I remember very clearly explaining to my patients that their cholesterol needed to be addressed. Because I was a new doctor on the block, they would go back to their old doctor and say, "Oh, your cholesterol is fine. It's not over 300." I got a lot of pushback at that point, but then there was this transition that occurred in the mid to late 80s.
That all changed. You know, they lowered the standards. And then of course, in 2000, they lowered them again. The target market for these pharmaceutical interventions really increased quite dramatically.
CJ : Right.
DM : I'd like to just review another component of the benefit of cholesterol, before we go into how we'd measure and identify those who are at risk for these problems. But just to reinforce the importance of cholesterol, you had mentioned some of the biological functions of cholesterol, and I'm wondering if you're familiar with Dr. Stephanie Seneff's work , who also works with Weston A. Price.
One of her new theories is that cholesterol actually combines with sulfur to form cholesterol sulfate, and that this cholesterol sulfate actually provides a very profound benefit on thinning the blood. It may serve as a reservoir of the electron donations that we receive to stay healthy from grounding, and distribute that around the bloodstream to actually increase the electron negativity of the red blood cells to repel them from each other.
(Note added by VitaminDWiki: podcast of Stephanie Seneff Aug 2013 at Paleorunner
[-----20:00-----]
And by so doing - thinning the blood - essentially provide a decreased risk for heart disease, very similar actually to statins. It's her belief that statins don't work by lowering your cholesterol. Although they do, that's not the reason they lower your risk for heart disease. Other people believe that they have an anti-inflammatory component. She doesn't believe they work that way either. She believes the primary method of action is related to this biomimicry, where they're actually substituting for cholesterol sulfate, donating the electrons (which causes the blood to thin), providing a relatively short-term acute decrease of heart disease.
But in the long-term, of course, it's fraught with many dangers, as you are well familiar with. I'm wondering if you've heard her speak on that topic or if you have any comments on it.
CJ : Sure. I recently met her and saw a couple of talks she gave at a local Weston A. Price Foundation conference in Indianapolis called the Indy Groundwork Conference. I spoke at that as well. I haven't gotten a chance to review all of the primary literature and so on and look at the research myself, but I think that her ideas are pretty interesting and certainly thought-provoking. It's really great to meet her and to see some of her presentations. I think this is. They can get pretty technical.
One thing that is interesting (I've written about this on my website): she thinks that the enzyme nitric oxide synthase, it's primary purpose is to produce sulfate rather than nitric oxide, at least in certain cell types. It is interesting that statins have been shown to increase nitric oxide synthase activity through certain mechanism. I won't go into all the details. But if anyone wants to go to [Cholesterol-And-Health.com] and look up "Rho activation" on my website, you can find all the details there.
But basically, that might fit in to some of her ideas, too. If perhaps statins actually increase the synthesis of sulfate, I don't know.
DM : Yeah.
CJ : But it's certainly a fascinating topic.
DM : Yes, indeed. You know, the more that we learn about health, the more we realize we don't know. This has been my observation. Let's get into identifying risk factors for heart disease. Because clearly, it's one of the leading causes of death... Maybe not the leading cause; it kind of battles back and forth between that and cancer, which probably has similar mechanisms. But my guess is that if you can optimize your risk for heart disease, you'll optimize your risk for pretty much most all of the other significant chronic degenerative diseases.
If we can identify some tools that would show us that we're really having a lowered risk of heart disease based on our cholesterol profiles, that would be useful. Now traditionally, of course, I think you would support the fact that total cholesterol, unless it's really elevated (above 330 or so, which would be suggestive of familial hypercholesterolemia), that that really isn't a risk factor - total cholesterol.
But there are subtypes where you look at the cholesterol ratios between HDL and total cholesterol, HDL and triglycerides, and some of the lipoprotein profiles that could be a profound indicator of risk for heart disease. You know, you've studies this really carefully, and I'm wondering if you could review that topic and give us your impression as to what the best indicators for a risk for heart disease would be.
CJ : Sure. Conventionally, even in the mainstream, we tend not to look at total cholesterol as the main measure. We tend to look, like you said, at subtypes like LDL and HDL. LDL and HDL stand for low-density lipoprotein and high-density lipoprotein.
Lipoproteins, we talk about them as if they're different types of cholesterol, but what they actually - the lipoproteins - are basically carriers for cholesterol in the blood. They're kind of like the taxi cab or the bus that's carrying the cholesterol around, and the cholesterols are like the passengers on that taxi cab or bus.
DM : And that's because cholesterol is fat-soluble. It doesn't flow around well in the blood. It needs a carrier.
CJ : Right. Basically, although Stephanie Seneff points out that cholesterol sulfate can be transported in the blood, the lipoproteins are basically a way to carry the fat-soluble stuff including cholesterol through the blood, which is water-soluble.
In general, what the mainstream tends to look at is to say LDL cholesterol is the "bad cholesterol" and HDL cholesterol is the "good cholesterol." You want a really low LDL. We want a pretty moderately high HDL and so on.
I think there's some truth to this basic paradigm in terms of their predictive value and the ability of LDL and HDL cholesterol to let us know whether things need to be optimized in the body. But I think it's important to note that just because these markers tend to correlate with risk, does not mean that one thing is causing the other.
For example, one of the most powerful predictors that's been validated across dozens of studies using hundreds of thousands of people is the total to HDL cholesterol ratio, which is basically the same thing as looking at the LDL to HDL cholesterol ratio. Because most cholesterol that is not in HDL is in LDL.
Basically, the higher the total to HDL cholesterol ratio, the greater the risk of future heart disease. Now, does this mean that a high total to HDL cholesterol ratio causes heart disease? Well, the best way to put that to the test would be to come up with a drug that specifically changes the ratio of LDL to HDL cholesterol ratio and to see if that drug prevents heart disease. So far, we've tried to do studies on this, and they've been a miserable failure.
The most famous of these was the trials with Torcetrapib, which inhibited the enzyme that transfers cholesterol from HDL to LDL. By doing so, it specifically increased HDL cholesterol and decreased LDL cholesterol. But what happened? People started dying left and right after taking that drug. They have to cancel it early. Now what they've tried to do is say that the drug had off-target toxicity and that it did something else - we don't really know what - that killed people, but they didn't die because of the actual function of the drug.
Now they've come up with another drug, Anacetrapib, that does the same thing. But they're hoping it doesn't have the same off-target toxicity.
DM : Where these drugs ever released? Or they got nixed just in clinical trials?
CJ : I believe that Torcetrapib got nixed in the late-stage of the Phase III clinical trial. I would fact-check that, but I believe that was the case.
DM : Okay.
CJ : Anacetrapib, they've published a short-term early-phase trial, where they showed that it didn't have any negative effects. But they had shown the same thing with Torcetrapib in the early phases. I don't know why they're so confident about Anacetrapib. We'll see what happens. But there's a real positive that drug might kill people left and right, too.
Just because the total to HDL cholesterol ratio predicts heart disease doesn't mean that it causes heart disease. We need to be really careful and keep that in mind, because the same thing applies to any other marker we look at, whether it's, you know. Maybe later in the show we'll talk about particle size and these other things. We always have to keep in mind that just because it correlates, doesn't mean we can change it and change the risk of heart disease.
The way that I like to look at this is as metabolic markers. I try to understand why is the total to HDL cholesterol ratio correlated with heart disease, despite the fact that we don't really have any good evidence that it causes heart disease.
My personal view is this: these lipoproteins need to transport cholesterol through our body, so that the cholesterol can be used for all the good things that cholesterol does, like we want to make bile acids, we want to make sex hormones, and all these great things.
In order to do that, we need to have good metabolism and good turnover of LDL particles. We have a receptor called the LDL receptor. And the function of that receptor is to bring those lipoproteins into the cell, so that they can be used for all those good things. There are two primary governors of LDL receptor activity. One is the cell says, "How much cholesterol do I need?" When that individual liver cell, for example, needs some more cholesterol, it will take in more LDL particles from the blood, so it can use it.
The other key regulator is thyroid hormone.
[-----30:00-----]
Thyroid hormone isn't communicating a particular cell [inaudible 30:08]. It's communicating the state of the whole body. It's communicating to those cells. It's saying, "We are in a state of abundance. It's time to use cholesterol for all these goodies, so we can have a great reproductive success." For example, "Let's use that cholesterol. We've got so much cholesterol. We're living in a time of plenty. We're going to use it make lots of sex hormones."
When our body's communication signals are running correctly and our body recognizes that we're in a state of abundance - we have everything we need to use the cholesterol to promote health - then those lipoprotein particles turn over relatively quickly.
Now, what happens when the lipoprotein particle doesn't turn over very quickly? Well, as LDL spends a longer time in the blood, it entraps the HDL particles for a more extended period of time, and cholesterol is transferred from HDL to LDL. That causes the amount of HDL cholesterol to lower and the amount of LDL cholesterol to increase.
In my perspective, the total to HDL cholesterol ratio, when it's increased, that may indicate poor turnover and metabolism of the cholesterol. It means that we're not using the cholesterol for the things that we really need. Now, I don't think necessarily that that is causing heart disease. But what does happen when LDL particles sit around in the blood too long is that they tend to oxidize and be damaged. When those particles are damaged, then they become toxic to the cells in that line of blood vessels. The immune system comes along and cleans up those damaged particles by creating a plaque.
The way I view it, it's kind of like cleaning up a big mess or creating a Superfund site to clean up a toxic mess. Or it's sort of like, you know, quarantine these particles, cleaning up broken glass into a pile, or something like that. It's a good temporary measure. The problem is that later down the road, decades later, that plaque or debris can break and spill out factors into the blood. It could cause a blood clot, block an artery, and that can lead to a heart attack.
It's not the formation of the plaque itself that's bad. But what we really want to do is prevent these particles from being damaged. The best way to do that is [inaudible 32:47] metabolism, where we're taking those fat-soluble vitamins and cholesterol in fats into our cells and using them properly. That's the way I see why this acts is a marker.
DM : Thank you for mentioning the component about the arterial plaque and the importance of the cholesterol to that. But there's another important contributor, vitamin K2 , which I believe is responsible for the integration of the calcium into that plaque and producing it through proteins like matrix gla protein or MGP that facilitates that. I'm wondering if you can comment on the interaction and the integration of those two and how that plays into the role that progresses the heart disease. Because it seems to be another powerful source.
CJ : Sure. vitamin K2 is one of the two forms of vitamin K. We have vitamin K1, which is found primarily in leafy greens. Vitamin K2 is found primarily in fermented foods and animal fats. The best sources of it that most people consume are actually egg yolks and cheeses, especially hard cheeses.
We have some epidemiological evidence that the more vitamin K2 people eat - but not K1 - the lower their risk of heart disease, and the lower their risk of calcification of the heart valves. We also have a lot of evidence from animal experiments showing that vitamin K2 is important in protecting against calcification of the blood vessels in general. Calcification basically occurs in two ways in the blood vessels, and both of them we need vitamin K to protect against.
One is that in atherosclerosis, which basically happens in the innermost layer of the blood vessel that lines the actual passage of the blood, we have local deposits of calcium in advanced plaques. This is not a uniform distribution of calcium, but it happens in certain spots. Then we also have in a layer behind that the media, sort of the more interior layer of the blood vessel. We have a more uniform distribution of calcium that tends to occur as we get older and is especially accelerated in diabetes and kidney disease. In both cases, wherever we find the calcification, we find defective matrix gla protein or MGP.
MGP is a vitamin K-dependent protein that is responsible for protecting blood vessels and other soft tissues from calcification. If vitamin K is not present in sufficient quantities in the diet, it cannot activate MGP, so MGP is defective and MGP therefore cannot protect against calcification of the blood vessels, heart valves, and all their soft tissues.
It seems from that evidence that we have that insufficient intake of vitamin K2 leads to greater calcification in atherosclerosis and greater medial calcification, which in turn increases the risk for heart disease. This is particularly ironic, because in most people's diet, the best sources are eggs and cheese, which are high in cholesterol and we're told to avoid.
DM : Well, thank you for explaining that. Would it be fair to state from your perspective that the calcification that occurs in arterial plaque formation is really dependent upon two causes? One would be this decrease in antioxidant levels, which causes oxidation of the LDL cholesterol, and then the decrease or deficiency of vitamin K2. That you really need both of those conditions to develop significant levels of arterial plaque.
CJ : I think that it's a little bit more complicated than that. Sometimes you develop a plaque that becomes very vulnerable to rupture, because of high contents of oxidatively damaged products and high inflammatory activation, but it isn't necessarily very calcified. Whereas you might have other plaques that are highly calcified and are problematic, because they are highly calcified.
In all probability, what we are always saying is probably a combination of the two, where regardless of the specific plaque site - whether every plaque has both going on - most people probably aren't getting enough vitamin K2, and most people probably have too much oxidative stress and inflammation. I think you have all of that going on.
But it's important to note also that vitamin K2 plays a lot of roles besides protecting against calcification. It may play a role in improving cell survival.
One of the factors that you have in atherosclerosis is you have a lot of cells that are dying. When the cells die, they tend to accumulate all kinds of debris and that access sites for calcification and that access sites to attract inflammatory cells. And vitamin K2 seems to play a role in improving cell survival, which also prevents atherosclerosis, even besides the issue of calcification.
DM : Well, another powerful reason to make sure your vitamin K2 levels are up. My favorite source of vitamin K2 is fermented vegetables.
CJ : Yeah.
DM : Not taking a supplement. We've actually recently done a laboratory analysis that if you use a starter culture that really has bacterial strains that are optimized for this vitamin K2, you can get up to 500 or 600 micrograms in a serving of vegetables, which is way beyond the therapeutic range of what you would normally need per day to reach optimized levels.
CJ : Great. In the published literature, only natto - the fermented soy food - has been shown to have really high levels in terms of fermented plant foods. One of the things that's been speculated for a while is what it would take those bacterial strains and ferment something else. That's really great that you're doing that work.
DM : Yeah. We did the research. It was really just, you know, sent it out to a lab. Optimize the strains, send it out, and we can do it. But it's literally 10 times as much vitamin K2 that you would from fermenting the same vegetables with the traditional starter culture or the strains that are present typically in the environment.
CJ : Yeah.
DM : Like the Lactobacillus strains that are on cabbage that one typically uses. We're actually producing a product on that in the near future . Because not only do you get the benefits of all those bacterial concentrations (which are profound), it may even exceed the benefits of vitamin K2 - but it would be best to have them both. I mean, that's at least from my perspective.
Now, interestingly with the arterial plaque, there was a test 15 or 20 years ago I remember that actually was quite controversial and still exists.
[-----40:00-----]
It's called the coronary calcium scan or cardiac CT scan for calcium scoring. I'm sure you can comment. I know it's an X-ray test that actually measures the amount of calcification in the coronary arteries to give a predictive risk for heart disease. I know that was really quite controversial. I don't recall if it was a traditional X-ray or if it was a CT scan. I think it was a CT scan.
CJ : Yeah.
DM : Which, of course, has its own downside, because a CT scan has got a hundred times more radiation than a traditional chest X-ray. I'm wondering if you can comment on that and its predicted value for heart disease.
CJ : Sure. This isn't something I've studied in detail, but I've read a little bit about it. It is a CT scan . In general, people have tend to quantify just how much calcium is there in the coronary arteries. There have been a number of studies. I haven't looked at them all in detail, but my understanding is those studies have generally shown that it is a predictor of serious heart disease consequences. But there are a lot of other things that you can look at if you have a CT scan.
One of the things that's coming out more recently is, some people are saying, "You're getting this dose of radiation, so we should get the most information we possibly can." Doctors are encouraged to use the one CT scan to get a lot more information than just how much calcium is there. One of the things that you can look at is where is the calcium, what's the pattern, is it evenly distributed, is it spotty, or things like that.
You can actually look at a lot of other things in the individual's CT scan, like how much fat is there in the heart. You can look at liver fat, which is also a sign of some serious metabolic problems. And you can even look at some bone density and some other things.
There's actually a report that recently came out that was saying, "Look, to get the most out of this single dose of radiation, we should look at all of these stuff, because they can all really provide important information."
I think the thing to keep in mind, though, is that calcification tends to happen in a more advanced state of atherosclerosis. It's not an early sign of atherosclerosis . I think, you know, I'm not a clinician, and I don't have any personal experience with this. But I think it probably would be useful in certain scenarios, where you have someone. either you expect them to have atherosclerosis and you need to understand how severe is it.
I could imagine something like that might be useful periodically in the case of - say, you have someone with familial hypercholesterolemia. You find it very difficult to normalize their blood lipids with dietary approaches without severe drugs with adverse consequences and so on, and you're trying to manage the disease from a different perspective other than modifying blood lipids. I suppose looking at atherosclerosis more directly might be useful in those scenarios where those traditional preventative markers we want to look at just aren't good enough.
DM : Yeah.
CJ : But like you said, there is a dose of radiation, so it shouldn't be used carelessly.
DM : It's a huge dose. My memory might not be accurate. It may be a thousand times more radiation than a traditional chest X-ray.
CJ : That's right.
DM : It's not insignificant. We have enough negative exposures. And to electively use that as a diagnostic strategy, I think, is foolish beyond imagination, because CT scans should only be used as a method of last resort.
CJ : Yeah.
DM : I definitely want to delve into the. I think there are probably better predictive tests (that we'll talk about shortly) that you really have studied very well. But I just have another question about vitamin K2 from your perspective with respect to arterial plaque. Clearly, it's well-established that it's useful to prevent arterial plaque. But I'm wondering if you can comment on its use therapeutically to reverse plaque.
CJ : Yeah. Well, we don't have any studies in humans, but we have studies in animals, where it's been shown that you can reverse. That high dose of vitamin K2 can reverse arterial calcification. I don't know whether it would reverse atherosclerosis per se, in the sense of if you have an atherosclerotic plaque that's a complicated plaque and calcium is just part of it. I don't whether supplementing with high dose of vitamin K2 will reverse all of it.
But just with respect to calcification, animal experiments showed that calcification is reversible if you optimize vitamin K2 status.
DM : And my guess is if you also optimize other nutritional variables that we know tend to optimize your cholesterol profiles, such as eating cholesterol and reducing oxidized fat and vegetable oils.
CJ : Sure.
DM : Carbohydrates, insulin levels, and all of those.
CJ : Sure. Well, even going back to the cholesterol-fed rabbit model, one of the things that they showed - this is consistent across animal experiments of atherosclerosis, as far as I know - is that if you simply removed the cause of atherosclerosis (whatever is causing atherosclerosis in that particular animal model), atherosclerosis tends to naturally reverse on its own. Theoretically, optimizing the nutritional environment should be able to reverse atherosclerosis in general.
DM : It's a good support that the body wants to stay healthy as long as you allow it to. Don't sabotage it in some way. I'm wondering if you can expand now on some of the better new tests that are out there that even go beyond these cholesterol ratios that you referenced earlier, such as the NMR and some of the other lipoprotein profiles.
CJ : Sure. Well, what we have to keep in mind, of course, is that these are new tests. They're kind of in their state of infancy right now. But one of the things with particle size, for example, is that it's been shown that... This was sort of a surprise to people who thought that LDL was the "bad cholesterol." But it was shown quite a while ago - a decade or two ago by now - that if you look at simply how large is the LDL particle, people with smaller LDL particles have a much higher risk of heart disease than people with larger LDL particles.
This was a big surprise to people who just said LDL was the "bad cholesterol," because now it looked like there were good LDL particles and bad LDL particles. And things got more complicated.
I think we have to have the same critical analysis of particle size that we have of the ratios. There are reasons why we would say that "Perhaps small LDL particles are the cause of heart disease," but none of these ideas about small LDL particles have actually been shown definitively to be true.
If you imagine, the blood vessel have several layers, like my hands here. When you have inflammation, you tend to have larger openings in the first layer that allow LDL particles to go through. If you have smaller particles, they can more easily fit through those openings. Once they're behind there, the smaller particles tend to get stuck there more easily. They tend to be more vulnerable to oxidation and so on. There are a lot of theories about why small LDL particles might be the cause of heart disease.
However, the way that I look at this is like this. I think there is no better-supported hypothesis or theory about what causes heart disease in terms of lipids than that slow turnover of LDL particles (meaning, we're not using them efficiently) leads to spending a long time in the blood at a greater tendency toward oxidative damage.
What happens when LDL particles stay a long time in the blood? They don't just get higher levels of cholesterol taking it from HDL, but they also get smaller, and they get denser. So, small LDL particles may be just another marker for poor metabolism.
Right now, my current view is that the total to HDL cholesterol ratio and the particle size are probably communicating largely the same information that either one can be a sign of poor turnover in metabolism and use of the LDL-associated cholesterol. Now, in terms of whether we should test it, there are a couple of things to look at. One is that there are several different methods of measuring particle size. So far, scientists haven't agreed on which one is the best one. This is still a matter of debate.
For example, there's NMR. There's VAP. There are a few different types of electrophoresis. The ones that are most available to the average patient are going to be the VAP test and the NMR test. There was one study where they took - I think it was 40 people. They had their blood analyzed in all these different ways. They're analyzing the same exact blood, but you're giving it all four or five different tests to measure particle size.
[-----50:00-----]
This showed that in the VAP test, only eight percent of people were classified as Pattern A, which means they have the large LDL, which is the good LDL. In the same people, when they were subjected to a certain type of electrophoresis, 80 percent of people were classified as Pattern A. The question is, "Which is the right way to measure it?" NMR was kind of in the middle between the two. There's that question.
Then there's a question on.We know from what numerous studies have shown that people with smaller LDL particles are more likely to have a greater risk of heart disease in the future. The question is, "Does that provide additional information above and beyond what the total to HDL cholesterol ratio is providing or other traditional risk factors? Or is it communicating the same information?"
To date, I would say there are too few studies to answer these for sure. There's a handful of them. Some of them have reported the results without making statistical adjustments for more traditional risk factors. The ones that have made the adjustments have used different ones. So far, it looks to me like when you tend to look at particle size and the ratio, they're both communicating information. But it's very unclear whether you're actually getting more information about future heart disease risk when you have the two together.
I think with particle size, if it's affordable (especially if your insurance is going to pay for it), then it would be really interesting - especially for someone like you who gets a chance to see even in your own practice how a large amount of data might correlate with different outcomes -to have these measurements done and to see what you can come up with in terms of what correlates with what.
In terms of the average person who's going to their doctor, who will get the total to HDL cholesterol ratio, and they won't have to pay for it except for the co-pay (versus going online and paying 175 dollars for it on [HealthCheckUSA.com] or something like that), I'm not ready to tell that person that the particle size is so important that they should pay the extra 175 dollars.
I think it's really an individual thing, where depending on the cause and benefit scenario, we should use the information that we can generate affordably to try to maximize how we can understand this person's metabolism and what are the most likely things to help them optimize their health.
DM : Well, interestingly, I do believe that the cholesterol ratios and the particle size are really most likely indirect measurements of the more important foundational physiological process, which is the turnover of the LDL, as really being the primary culprit. And obviously, that's not something you can measure directly. These are just indirect measurements. I'm wondering if you could comment on the variables that contribute to this LDL turnover, and what would optimize that to be at a level that is consistent with good health.
CJ : Sure. Well, I think that one of the things that can definitely affect that we don't have much control over and is probably not the main reason for most people is genetics. People who have genetic defects in the LDL receptor - familial hypercholesterolemia -they have a primary problem with turnover. That's much more difficult to deal with.
In the general population, I think it's a matter of miscommunication. Basically, the communication molecules, the hormones, are not functioning correctly.
One thing we know is that insulin resistance is extraordinarily common. I think there are number of reasons for this. Probably the primary one is that overweight and obesity is very common, but of course, there are number of other factors that play into that. In any case, insulin actually helps govern thyroid hormone and also may even have a direct impact on promoting LDL receptor activity. Insulin helps us make more thyroid hormone, and it helps activate T4 into T3. This helps increase LDL receptor activity and turn over these LDL particles.
The problem is that a huge portion of our population is insulin-resistant. The insulin is there. Maybe even more insulin than usual is there, but it's not carrying out its function properly. I think correcting insulin resistance is probably a major factor in normalizing thyroid function, which in turn could normalize cholesterol metabolism. Now of course, how to do that is extraordinarily controversial. I have some opinions, but probably no one's going to agree on exactly the right way to attack the insulin resistance issue.
DM : Well, before you answer that question on expanding on your reasons as to why you believe some of the variables. Before you answer the question on some of the strategies that you can use to improve insulin resistance, I'm wondering if you can comment on the contribution to leptin, because some experts believe that leptin also plays a major role in this area.
CJ : Sure. Leptin is a hormone produced by our fat tissue. It appears that a lot of us have a lot of fat tissue. We make a lot of leptin, but the leptin is not doing its job. Leptin does play important roles in governing insulin and, in turn, governing thyroid hormone. Basically, these hormones are all very connected.
The question is, "What is the primary thing that we need to optimize? If leptin governs insulin, do we fix leptin, or do we fix insulin?" I think that probably, yes. Probably leptin plays that role in governing insulin and the downstream thyroid function. But I don't know that it necessarily would make a huge difference in how I would approach the issue.
DM : Sure.
CJ : Especially since the non-functioning of these hormones is so intimately tied to obesity that really, probably anything that successfully fixes obesity is going to fix the hormone function. That's probably going to vary a lot from person to person.
DM : Well, let's hear your controversial approaches to this. I'm very interested.
CJ : Sure. Well, I think the main controversy is that, especially in the alternative health realm, there are a lot of people who feel that insulin is the main cause of insulin resistance. This idea is basically, the more insulin you have, the more resistant you're going to be. The solution to insulin resistance is to minimize insulin. If that's the case, then what you want to do is to not eat carbohydrates, for example. And maybe you don't want to eat so much protein either.
I think that there may be some value in that approach for some people. But I do not believe that the primary cause of insulin resistance is insulin itself. My view is that insulin resistance - I kind of view it the same way that I view the formation of the plaque. The formation of the plaque is not the ideal scenario, but it's not the thing we want to stop.
For example, like when we talked about atherosclerotic plaque before, you have these toxic things floating around in the blood, the oxidatively damaged molecules. The immune system wants to clean it up and form the plaque. You don't want to intervene right at the point where you stop the immune system from cleaning it up. That's not bad, right? I look at insulin resistance in kind of the same way. In my view, insulin resistance is a natural reaction of the cell to energy overload.
Before I go on, I want to clarify that I don't simply mean people are eating too much. What I mean by energy overload is a little bit more complicated, and I'll explain that in a minute. But basically, if the cell is receiving energy - for example, in the form of glucose, we know that insulin brings glucose in the cells. It does other things, too, but one of the things that it does is bring glucose into the cell. Or in fat cells, for example, insulin also brings fat into the cell to store it.
If the cell cannot handle that energy, one reason could be that there's too much energy coming in. But another reason could simply be that the ability of the cell to handle that energy is diminished. Then the cell is going to shut off that energy input and say, "Look, I don't want to bring more energy into the cells." The fat cell is going to say, "Insulin, I see you there, but I'm not taking that fat into the cell." The muscle is going to say, "Insulin, I see you there, but I'm not taking any more glucose into the cell." So, the cells stop listening to the insulin.
[----- 1:00:00-----]
There are a lot of people who find that if they eat a low-carbohydrate diet, it helps them maintain their weight better . I think someone who fits into that category - eating a low-carbohydrate diet - is going to help normalize the insulin signaling, because it's taking care of one aspect, that energy overload. For another person, there could be someone who is deficient in a certain nutrient. Maybe they're deficient in B vitamins, and they're not able to burn energy or something like that.
There are a lot of different things that could be going on that could cause energy input to be overloading the ability to burn, use, or store the energy. Depending on why a person is suffering from that energy overload, fixing their particular problem - whatever it is, whether they're deficient in certain nutrients, whether they're eating a diet that is giving them a foggy head, and they don't want to exercise or think about anything, they're lying in bed all day, whether they're eating a diet that is just making them overeat, or whatever it is - I think that's going to vary from person to person.
The thing about carbohydrate restriction is... Let's say, someone loses a lot of weight by eating a low-carbohydrate diet, and then they come to a point where they maintain a healthy weight. You need - in my view - some carbohydrate in the diet to have some insulin for the insulin to do its job. I don't think it helps you to have maximal insulin sensitivity, if you don't have any insulin. I think that could be controversial, at least, in some circles, especially in the alternative health world, where a lot of people feel that carbohydrates are the enemy.
I don't feel like that. I feel like carbohydrate restriction may have value for some people. But overall, fixing insulin sensitivity and fixing insulin signaling is going to require, for most people, some carbohydrate in the diet, at least enough to actually get that insulin out there, so it can do its job.
DM : Yeah. Well, thank you for expanding on that. I'm actually.. In the near future - I think in a week or two - going to be having a three-hour debate with Dr. Ron Rosedale and Dr. Paul Jaminet to address that very specific issue with the insulin and leptin signaling and is there really such a thing as a safe amount of carbohydrates. It is controversial. I think there's a lot of good science on both sides and really good arguments. I appreciate you sharing your perspective on it. So, it sounds like you're really not a huge fan of these more advanced newer technologies like NMR and VAP.
CJ : Right.
DM : Certainly, they have their indications, but maybe we can use these traditional views. I wonder if you can comment on even a simpler test that people can do at home. Because I think ultimately, one of the artifacts or another biological parameter that we can assess that is an indicator that either the LDL turnover is not right or maybe more fundamentally the signaling process is disturbed is that you have increased levels of body fat, which could be independent of your weight.
Because you can have, theoretically, a very muscular person, an NFL football player who could be overweight, but not have large amounts of body fat. It would seem a simple method to assess that body fat might be another powerful predictor of heart disease. And of course, the deposition of that fat - the waist being more important than the hips, or the waist-hips ratio. I'm wondering if you can comment on your perspective or view on using indirect measurements of body fat. My particular favorite is the waist circumference.
I mean, obviously you can do an underwater body measuring, dexa scans, skin calipers, or bioimpedance. But the waist measurement is a simple measurement that requires a one-dollar tape measure that basically you can have the rest of your life to measure this and to monitor that throughout. I'm wondering how you would place that measurement in the total context of these tests that we would use to predict our risk for heart disease.
CJ : Sure. Well, I mean basically, heart disease is very strongly related to all of these metabolic dysfunctioning. And that's very much tied to obesity, but more specifically certain types of obesity. Visceral fat is more important. Abdominal fat is more important. The waist-hip ratio is a valuable marker . It certainly doesn't cost very much money.
Where that would fit in, I would think, is if someone's trying to optimize their. People shouldn't try to optimize their weight. They should try to optimize their body fatness and body fat distribution . I think something like that would be a lot better than jumping on the scale every morning.
DM : Or even measuring your cholesterol ratios every week or every month. CJ : Sure.
DM : I mean, how would you compare between the...They're actually blood measurements.
CJ : Every week or every month is a little bit extreme. But I think that those measurements can have a lot of usefulness sometimes in finding things that people wouldn't be able to predict otherwise. I'll give you one example. I knew a guy a talked to who started having his LDL cholesterol start floating up unexpectedly over the course of several months. He ignored it at first, because he was on forums. People said, "LDL cholesterol is not a cause of heart disease. Don't worry about it. Don't look at that." And it kept going up higher.
Eventually, he developed a number of other problems. Among them, he got really high iron levels and anemia at the same time. He went to a bunch of different specialists and probably paid a lot of money trying to figure it out. They couldn't figure it out. He went from one person to another, and they couldn't figure it out. He talked to me and I said, "Look, I think what's happening is this." He had some other symptoms. I don't remember them all, but they all sort of fit into this picture.
I said I think what's happening is, you made some dietary changes that impacted your thyroid function. Your thyroid activity started going down . First thing that started happening was your LDL cholesterol started going up . And then as problems became more advanced - in some cases with low thyroid activity (you don't always have this) -you have erythropoietin and you don't make blood cells. Then what happens is your iron goes up into the hemochromatosis range and your blood cells go down into the anemia range.
He eventually - at least as far as I understand - went to another practitioner who had his free T3 measured and lo and behold, it was extremely low. And he was then on the path to recovery.
In my personal opinion, if LDL cholesterol starts going up... I wouldn't have the same normal range as what they give you for the clinical recommendations in most places. But LDL cholesterol going up, even if LDL cholesterol is not a cause of heart disease, it can often be used as a metabolic marker for a number of things including thyroid function.
In my personal opinion, if the LDL cholesterol starts jumping up unexpectedly, absent predictable causes... For example, if someone loses a lot of weight, I would ignore their blood lipids until their weight stabilizes. But if it starts going up for no apparent reason, then it's time to look at some other metabolic clues to see if it can be an early sign that something else is going on. I think he could have saved a lot of money and a lot of hassle if as soon as his LDL cholesterol started going up, he had his Free T3 measured. You see.
Another example: someone came to me. Their father had, I think, a total cholesterol around 250, which in itself is a little high, but it's not that high. You find people... Especially women, but in general, you find that in Pacific islanders who eat a lot of coconut oil, they're free of heart disease. So, 250 is not the, Oh-my-god-you're-going-to-die-of-a-heart-attack range, despite what the reference range in the lab might say. However, the total to HDL cholesterol ratio was over seven (which is really high), triglycerides were really high, and testosterone was really low.
What does this say to me? Well, I look at it this way. Triglycerides being really high are a sign of insulin resistance in most cases - not always, but most of the time. If you don't have insulin sensitivity, you don't have as good thyroid function as you should. When your thyroid function is poor, your cholesterol starts going up. But mainly, your total to HDL cholesterol ratio starts going up, because you're not turning over those LDL particles and you're not using them to produce things like testosterone.
The way that I see this is: the high triglycerides indicated insulin resistance, insulin resistance caused poor thyroid function, poor thyroid function caused high total to HDL cholesterol ratio, and low testosterone because the LDL cholesterol wasn't being brought into those cells, where testosterone is synthesized.
[-----1:10:00-----]
While I wouldn't say that 250 total cholesterol is a warning sign in and of itself, when [inaudible 1:10:09], I would say, "Okay, what's your ratio?" If your ratio is really high like seven is really high, I would say "Okay, can we measure other indicators of thyroid function? Do you have low testosterone? How do you feel?" If someone like that has elevated blood lipids and they're feeling fatigued, or they're libido is poor or something, that can be a really. Together, the whole picture can act as a warning sign that thyroid function is off.
Now, there are some doctors where everyone who comes to them, they measure Free T3 or something like that. Maybe measuring cholesterol isn't as important in cases like those, but we have to realize that the vast majority of people on the Internet, you know, that we're reaching probably, they have a regular doctor. They go to their doctor, and all their doctor measures on a regular basis are those few blood lipid panels. They're not going to go into the doctor, and the doctor's not going to ask them all signs and symptoms of thyroid function and measure the full thyroid panel, but the antibodies and the free thyroid hormones and all that stuff.
It just doesn't happen. So, for someone who has access to a regular doctor and these are the main things that are measured, rather than ignoring them... I mean, you're going to go to the doctor, and they're going to measure that stuff anyway. Rather than ignoring that and say, "Oh, that's not the cause of heart disease," I would say, we're going to measure it anyway; let's harvest as much information as we possibly can from this really cheap routine measurement that everyone gets done.
To me, it's not about being scared of high cholesterol. It's about how can we harness information about that and use it as clues to help us in our search for the other things you want to measure or the other signs and symptoms we want to look at to see: is there's something metabolically wrong with this person that needs to be optimized?
DM : Well, thank you for pointing that out - the important relationship between thyroid hormone and cholesterol. Because it's one that's not frequently mentioned, yet is a big issue. And frequently, before the introduction of statin drugs, one of the common treatments for high-cholesterol was routinely the use of thyroid hormone. I mean, it was, clinically. That was even before my time, way before the '80s.
CJ : The most effective trial I've ever seen in something that reduced the risk of heart disease pharmacologically was a trial that William Kountz published in the 1940s, where he took people who had low metabolic rates and gave them thyroid extract . He almost obliterated their risk of heart diseases, especially in the younger people, way more effectively than statins or any of the other drugs that are given now.
DM : Yeah. And it's particularly important now in the 21st century, because of the pervasive use of fluoride and soy protein, which are both potent inhibitors of the thyroid function. For some reason - and may be you know why - this seems to be particularly pernicious for women. They seem to be far more susceptible to this problem than men. Of course, it affects both sexes. But just like autism and ADHD that seems to affect males more, this thyroid dysfunction or impairment seems to affect females more.
CJ : I don't know why that is, but that's pretty interesting.
DM : Yeah. But it is an important point. I would certainly add that to the list of thyroid screens and something that I personally need to emphasize more and remember, because it is such a massively important component not only for normalization of that, but the normalization of the fat [inaudible 1:13:42]. Many people try all these well-known strategies to lose weight by optimizing their diet and exercising. They're not effective because they have dysfunctional thyroid hormones.
CJ : Yup.
DM : You add that back into the mix, and the whole world changes. That's not true for everyone, but for the person who is affected by it, it's a difference between life and death frequently.
CJ : Yeah.
DM : Thank you for bringing out that point. It really is great to have access to your research, knowledge, and your perspective, because you're so impartial and unbiased and you're a voracious reader of the literature. You really understand these studies at a very deep level and can identify these things.
I'm wondering. First of all, thank you for sharing this information with us. But are there any new items on the horizon that you see up and coming or that you feel is important to emphasize at this point or at least to comment on?
CJ : You mean, with respect to tests?
DM : No, with respect to anything. Because I think we've hit the cholesterol issue and the tests, and I think you've really given us a good perspective. This is anything on your research horizon or like maybe even comment on some of the things that you're studying now on your research down at the University of Illinois.
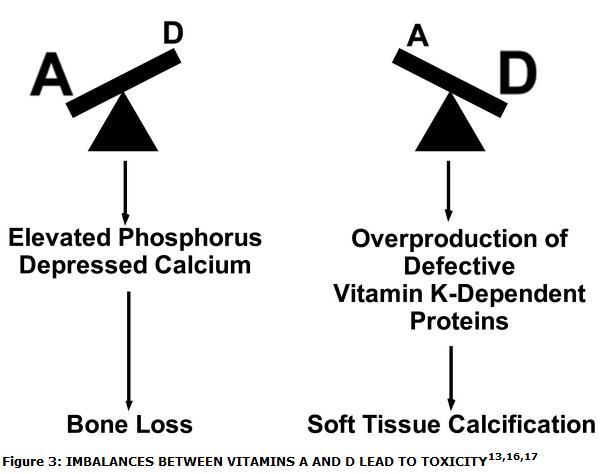
CJ : Yes. Right now, on my horizon, I'm getting ready to resurrect some research into a hypothesis I published back in 2007 on the interactions between vitamins A, D, and K . The basic crux of my hypothesis is that vitamin D raises the need for vitamin K , because it stimulates the production of vitamin K-dependent proteins.
DM : This would be vitamin K2, right?
CJ : Yeah.
DM : Or both?
CJ : Both can help, but vitamin K2 is much more effective when it comes to protecting against soft tissue calcification. Basically, my hypothesis is that these vitamins are all needed together. I'm going to be doing some mechanistic research into that. And hopefully, as things progress, I'd like to move this into the realm of some human studies where we can look at, you know, what are the optimal ratios of these vitamins, and how does this actually work in humans at doses of the vitamins that people are getting.
I think it will be a while before we have information like that, but that's what I'm currently working on. That's the main thing that's on my horizon right now. Yeah.
DM : So, is this a postdoctoral position that you have? Then how long do you plan on being on this and what are your plans for the future?
CJ : Oh, well, our contract is a year at a time. My hope is that. At least during this postdoctoral research position, my plan isn't based so much on time. You know, a position like this might be one to three years. But my real hope is that I can move the focus on these interactions into the realm of convincing other researchers that these interactions are relevant and need to always be looked at when we look at studies of any of these three vitamins.
I think what that will be is in animal experiment that I'm working on now, which will really answer some mechanistic questions that need to be answered and round out some of the holes in the literature, and then moving into a human study to show that the dose of these vitamins that people are currently taking in are relevant to these interactions. I think once something like that gets published, that will really sort of open other researchers' eyes. If other people start considering these important issues, I'll be satisfied with my postdoctoral project.
Other than that, I haven't planned too far ahead, but I will eventually be coming out with a book on heart disease. I'm not ready to give a date for that yet. And of course, I will carry on with writing, speaking, and researching on topics like these.
DM : Well, great. We're glad to have you as a resource. I really appreciate your contributions to helping us all understand more about these really important issues. Thank you for all that you do and good luck to you in the future.
CJ : To you, too. Thank you so much.
[END]
