Evidence-Based Vitamin D Conference
Vitamin D: Moving Toward Evidence-based Decision Making in Primary Care
website includes video of the 1.5 day session
December 2-3, 2014
Sponsored by
Office of Dietary Supplements, National Institutes of Health, Bethesda, Maryland
10 Federal Co-sponsors
Summary of Conference Presentations and Discussions - Published Oct 2015
📄 Download a 6 page summary PDF from VitaminDWiki
📄 Download the NIH detailed PDF from VitaminDWiki
Text and some graphics from the NIH PDF follow
PREFACE
When questions center on vitamin D screening, status and supplementation, what are the key issues in providing guidance about these matters to primary care practitioners? The media and healthcare system's increased focus on vitamin D and its potential health outcomes—coupled with mixed messages and conflicting recommendations about the benefits and safety of this nutrient— warrants a conversation about evaluating the available data for the purposes of making recommendations about vitamin D and for identifying the information gaps that need to be filled in the context of primary care practice.
The Office of Dietary Supplements (ODS) at the National Institutes of Health can serve as a forum for such conversations. With support from 10 federal co-sponsors, ODS organized a conference entitled "Vitamin D: Moving Toward Evidence-based Decision Making in Primary Care." It was held in December 2014, and more than 25 speakers and panelists took part, offering a wide range of scientific and clinical expertise. The conference was open to the public, and those in attendance contributed to the conversation. Given the professional experiences of many participants, the dialogue was rich and frank, and was characterized by a clear willingness to engage in constructive debates.
As highlighted by Conference Chairperson Dr. Clifford Rosen, the agenda was designed to begin with general discussions about evaluating data in the context of developing clinical guidelines and recommendations in the face of uncertainty. The focus then shifted specifically to vitamin D. Presenters were not tasked with resolving the controversies surrounding the benefits and risks of this nutrient, but rather to consider how to deal with existing uncertainties. A special panel described the clinical and media experience that currently surrounds vitamin D. This was followed by sessions on exploring the challenges in determining who is at risk of vitamin D inadequacy, the use of cut-points versus probabilities, the nature of the data on current intakes of vitamin D, factors that influence serum concentrations of vitamin D, and the risks from excessive supplementation. The final session reviewed the methodological stumbling blocks that cause inconsistencies in the measures of serum 25(OH)D concentrations—and hence, in laboratory reports from patient screenings—and which, in turn, suggest the need for analytical standardization. The conference concluded with a final discussion of the key points that were brought out and the gaps in information and data.
This document is a summary of the presentations and discussions that took place during the conference. Speakers were invited to give informal presentations; written text was not requested. Therefore, this document was compiled from the spoken words of the participants. However, it is not a transcript. References are included in many cases when cited by the presenters, but no effort was made to provide a comprehensive citation listing. The speakers and panelists listed at the front of this document are referred to in the text by their last name. The full name and affiliation of audience members who spoke are included when possible. The conference in its entirety can be viewed in video format by using the link: https://ods.od.nih.gov/Research/VitaminD.aspx
The conference was a success due to the hard work of many people. Scientific experts provided advice to ODS in identifying topics and relevant speakers. The support of Dr. Paul Coates as Director of ODS, Ms. Claudia Faigen, federal co-sponsors, and the staff at ICF International made the conference a reality. Special thanks go to Dr. Paul Thomas of ODS who, as co-rapporteur, helped to develop this document.
This conference was not designed to reach consensus, and consensus did not occur. Likewise, providing advice on vitamin D in primary care practice was not within the scope of the conference. However, several important themes were sounded. Participants acknowledged that while specific practice recommendations begin with solid science, their development likely requires the incorporation of values and preferences that must be clearly identified when the recommendations are issued. Participants went on to note the many uncertainties that surround the benefits and harms of vitamin D as well as the uncertainties about measurement of vitamin D status and desirable clinical targets. Concern was expressed about the disconnect between the current research focus for vitamin D and the current focus of clinical practitioners. Specifically, it appears that vitamin D supplementation is frequently prescribed to treat depression and general malaise despite virtually no evidence concerning its effectiveness. It was suggested that either research be conducted relative to vitamin D and depression or that work be done to better inform clinicians about the more likely benefits of vitamin D. When placed within the context of the notable increase in both vitamin D screening and dietary supplementation, and coupled with evidence of rising healthcare costs, this concern took on greater meaning. A related theme related to rising healthcare costs followed from the discussions about the U.S. Preventive Services Task Force conclusion that there is insufficient evidence to indicate that screening for vitamin D status improves health outcomes.
The suggestion that clinical decisions about vitamin D be based on a statistical probability measure such as a z-score, rather than on a cut-point, was embraced by some but not by all. Many participants acknowledged the important shared-decision component of primary care practice between provider and patient. But they pointed out that there is very little time for such discussions in the typical medical appointment, and then queried whether the many uncertainties surrounding vitamin D would preclude it being elevated for inclusion in such dialogues if the patient does not ask about it. One participant suggested that the only honest answer for many questions about vitamin D is "I don't know." Some participants suggested that the conference make specific recommendations about targets for vitamin D serum concentrations and provide other advice on vitamin D relevant to clinical practice. While this conference could not be the venue for such advice, the stated interest highlights the urgency underpinning the need for guidance.
Perhaps the most important question that came from the conference is "Where do we go from here?" The conference served to underscore that much work needs to be done to better understand the appropriate process and approach for developing clinical care guidance when the topic is fraught with considerable uncertainty. There was a clear call for future workshops to begin to resolve the issues surrounding vitamin D, which range from interpreting patient laboratory reports of vitamin D concentrations to incorporation of values and preferences in the development of guidelines for vitamin D.
Christine Lewis Taylor, Ph.D. Office of Dietary Supplements
WELCOME AND OPENING REMARKS – Clifford J. Rosen, M.D.
Conference Chairperson, Maine Medical Center Research Institute
This conference is taking place at an opportune time. There is intense focus on vitamin D in the research community and the public media. Furthermore, several groups have recently developed recommendations and guidelines, manufacturers are apparently adding vitamin D to more foods, and the dollars spent on vitamin D supplements have increased (Figure Intro-1). Screening for vitamin D status in primary care practices has also become more common (Figure Intro-2), and it can be costly. Further, the U.S. Preventive Services Task Force (USPSTF), an independent panel of experts who make evidence-based clinical practice recommendations, recently reviewed the relationship between vitamin D screening and health outcomes. In short, there has been and continues to be a plethora of information about vitamin D. The information is varied and has caused confusion, including in primary care practice.
FIGURE INTRO-1. Dollars Spent on Vitamin D Supplements, 2003-2014.
Sources: Nutrition Business Journal. NBJ's Supplement Business Report 2010. Page 3-49. New York, NY: Penton Media, Inc. Copyright 2009. Nutrition Business Journal. Supplement Business Report 2015. Page 25. New York, NY: Penton. Copyright 2015.
FIGURE INTRO-2. Vitamin D Laboratory Tests at Endocrine Laboratory, Rochester, MN, 2004-2010. Source: Personal communication to Clifford Rosen.
The starting point for this conference is an acknowledgement of the uncertainty surrounding vitamin D. The discussions here will not resolve the uncertainties, and the goal is not to clarify the benefits of vitamin D or to directly review in any depth the data on the relationships between vitamin D and health outcomes. Rather, the organizers hope that presenters and participants discuss the challenges associated with, and the best approaches for, distilling the data and related uncertainties into vitamin D guidance for clinical practice. Uncertainty will remain for quite some time. We must be honest and systematic about the knowledge gaps. And we must also be as transparent as possible about the ways that healthcare practitioners make clinical judgments and the nature of the data that inform expert opinion and clinical judgments.
The ultimate goal of this conference is to discuss strategies and to address uncertainties. We are also asked to highlight research gaps as well as data and methodological needs regarding the uncertainties surrounding clinical guidance about vitamin D. The Office of Dietary Supplements (ODS) at the National Institutes of Health serves as a forum for these kinds of discussions. The importance of the topic is demonstrated by the fact that 10 other federal agencies are joining ODS in co-sponsoring this conference (see Listing at the beginning of this publication).
_We have grouped the presentations and discussions into six sessions. The first session addresses the use of data. Subsequent sessions focus on common vitamin D-related uncertainties facing primary care practitioners, including risk of inadequacy, intake from foods and supplement use, and laboratory measurements. The final sessions consist of discussions about how to ensure that the guidance for primary care practitioners is developed appropriately, deals with uncertainties, and clearly describes the data used to form conclusions. Our conference speakers and panelists reflect diverse perspectives, and agreement will be elusive on most topics. However, the organizers have asked participants to reach as much agreement as possible regarding next steps, which are likely to be directed to a range of stakeholders.
My final task is to thank not only ODS and the federal co-sponsors, but also the speakers and panelists who are generously contributing their time and expertise. Dr. Christine Taylor from ODS worked diligently to conceptualize and organize this conference, and she deserves much credit for assembling the impressive array of conference participants. She and Dr. Paul Thomas from ODS will create an executive summary of this conference and ensure its publication and dissemination.!!!Session 1: The Challenges — How Do We Evaluate and Apply Evidence for Primary Care Decision Making?
PRINCIPLES FOR EVALUATING EVIDENCE
Presenter: Barry S. Kramer, M.D., M.P.H. National Cancer Institute, National Institutes of Health
This presentation focuses on how, and in what ways, scientists weigh evidence and how they and policy makers use the evidence to make recommendations that might affect many millions of people. A core tenet for prevention and screening is that it is difficult to make healthy people healthier, but it is sometimes easy to make healthy people less healthy. Therefore, the best starting point is the understanding that strong evidence of benefit is important when large numbers of healthy people are placed in harm's way.
Decision-making about prevention and screening can have different purposes, and negative reactions to the resulting recommendations can sometimes be due to a misunderstanding about the purpose of, or target for, these recommendations. Leon Gordis of Johns Hopkins University suggests that there are several levels of decision-making that can become conflated. The first is the individual- level decision, which is: "Would you have this done for yourself or someone in your family?" The decision at the second or health-professional level is: "What would I recommend to my patients/clients?" The decision for the third level is public-health oriented and affects hundreds of thousands or even millions of people: "Would I recommend this to the nation or the world?" This presentation pertains to the third level. Third-level decisions about public health recommendations should be based on rigorous assessments of high-quality evidence.
Underpinnings of a Data Evaluation
Two considerations should drive a data evaluation: the questions to be asked about the evidence, and the specification of an analytic framework for the evaluation. For the first consideration, the initial questions about the evidence that medical research needs to answer are:
What is the exposure and what is the outcome?
How certain is it that the exposure causes the outcome?
How important is the outcome?
How big is the effect?
To whom does the effect apply?
The next task is to develop an explicit analytic framework. Figure 1-1 illustrates a generic framework applicable to vitamin D. It is quite similar to the one that the U.S. Preventive Services Task Force (USPSTF) uses. Based on the framework, the first step is to identify the target population (on the left in Figure 1-1), and the last step is to assess the link between the intervention and the health outcome (on the right in Figure 1-1).
FIGURE 1-1. Generic analytic framework for vitamin D.
Although the framework has intermediate endpoints, they are not health outcomes. The literature includes many intermediate endpoints, but research has not validated most of them. These endpoints therefore cannot replace actual health outcomes in research. On the other hand, a validated intermediate endpoint (or a surrogate endpoint) could be used to make an inference related to the actual health outcome of interest. A mere association, however tight, between an intermediate endpoint and a health outcome is not a validated intermediate endpoint. Establishing the relationship between an intermediate measure and a health outcome requires a high level of evidence. The person establishing this relationship must be very confident of the link. However, typically only associations are available, rather than rigorous validations showing that the intermediate endpoint nearly always produces the same inference as the true health outcome. In most fields, validated intermediate endpoints are rare, and scientists therefore should emphasize health outcomes.
When the framework is completed for vitamin D (Figure 1-2), the complexity is clear. A dozen or more health outcomes are of interest. This large number of health outcomes is positive because it suggests that vitamin D could have health benefits. However, these many outcomes could also lead to multiplicity. That is, the more times a scientist examines and manipulates the data to detect a benefit, the more likely he or she is to make a false-positive discovery. In other words, rejection of the null hypothesis for at least one outcome becomes more likely, which leads to false-positive conclusions. These false-positive conclusions, in turn, lead to additional investments in mechanistic studies, which lead to more tests of the null hypothesis. This cycle is potentially never ending and rather vicious, and it underscores the importance of the hierarchy of evidence.
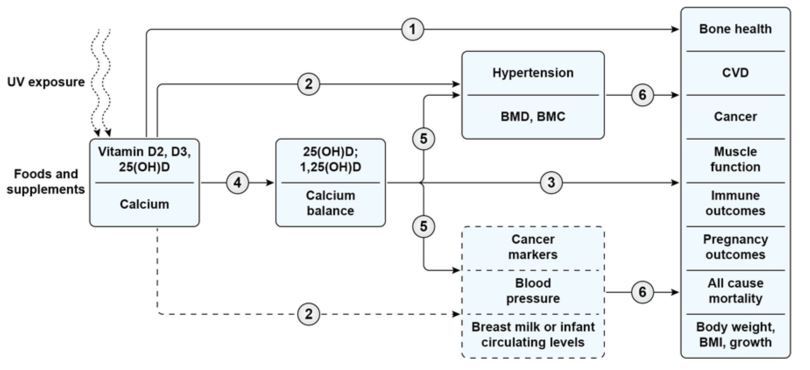
FIGURE 1-2. Detailed analytic framework for vitamin D with calcium.
Arrow 1: Association of exposure with clinical outcomes of interest.
Arrow 2: Association of exposure with surrogate or intermediate outcomes (that have good or possible evidence for linkage with clinical outcomes, respectively). (Surrogate outcomes are depicted in boxes with a solid outline, and intermediate outcomes are depicted in boxes with dashed outline.)
Arrow 3: Association of indicators of exposure to clinical outcomes.
Arrow 4: Association between exposure and indicators of exposure.
Arrow 5: Association of indicators of exposure to surrogate or intermediate outcomes.
Arrow 6: Association between surrogate or intermediate outcomes and clinical outcomes.
Note: UV= ultraviolet light; 25(OH)D = 25-hydroxyvitamin D; 1,25(OH)D = 1-25-dihydroxyvitamin D; BMD = bone mineral density; BMC = bone mineral content; BMI = body mass index ; CVD = cardiovascular disease.
Source: Chung M, Balk EM, Brendel M, et al. Vitamin D and Calcium: A Systematic Review of Health Outcomes. Evidence Report/Technology Assessment Number 183. Rockville, MD: Agency for Healthcare Research and Quality; 2009.
Hierarchy of Evidence and Causality
The hierarchy for ranking evidence is arranged in a pyramid, as shown in Figure 1-3, with higher- quality evidence at the top and less-reliable evidence at the bottom. Lately, the approach to ranking evidence this way has come under fire and experts have referred to it as outdated. However, abandoning this approach is risky, especially for third-level decision making about global recommendations. The closer the levels of evidence are to the base the pyramid, the more the studies are at risk of influence from confounders and a wide range of interpretations.
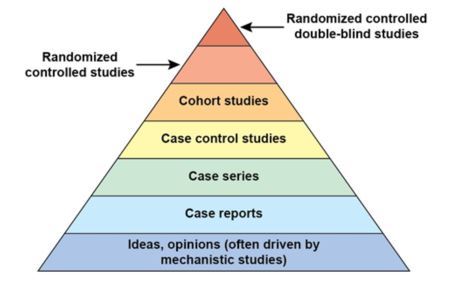
FIGURE 1-3 . Hierarchy of evidence. Higher-quality evidence is at top of pyramid.
A randomized controlled trial (RCT)-at the top of the pyramid—is the only study design that provides a direct test of causality. This design eliminates many confounders inherent in other study designs closer to the bottom of the pyramid. Observational data are useful for generating hypotheses.
At the bottom of the pyramid are ideas and opinions, which are only as strong as the evidence on which they are based. Too frequently, opinions are driven by mechanistic studies. Scientists generally do not fabricate opinions in a vacuum; rather, they observe mechanistic studies that "show" the likelihood that the intervention will lead to health outcomes. Such opinions are not proofs. Hypotheses are useful but must be tested.
Sir Austin Bradford Hill , a British epidemiologist, identified a series of considerations [1] that can help assess evidence of causation:
Strength of association: This consideration is often missing in chronic disease epidemiology. In the field's early years, epidemiologists primarily identified causes of acute diseases, such as infectious diseases, in which links between exposure and health outcomes had very high relative-risk values. As epidemiology began to address cancer, outcomes related to tobacco were associated with high relative-risk values. But for most exposures and chronic diseases, relative risks are less than 2.0. However, scientists often embrace these low relative risks with the same enthusiasm as high relative risks.
Consistency: If the available evidence—regardless of population, study design, or study implementation—gives the same result several times, the scientist is justified in believing that an association, if not necessarily causality, exists.
Specificity: The evidence should point to a specific site and disease without other likely explanations. Determining specificity is tricky for nutrients that have many sources of intake and claims of health outcomes.
Temporality: Evidence must demonstrate that the health outcome of interest does not cause changes in the nutrient intake or measure of interest. That is, scientists should not be fooled when a disease, such as cancer, causes changes in nutrient status rather than the other way around. This "cause-before-effect," or reverse-causation, phenomenon can be very challenging.
Biological gradient (dose-response association): The higher the exposure, the greater the effect. If the exposure stops, the effect recedes.
Plausibility: This is a weak c riterion because developing a plausible explanation for almost any phenomenon is easy.
Coherence: Epidemiological and laboratory findings should be coherent with the "known ...natural history and biology of the disease," but Hill noted that evidence from human studies is more relevant than that from animal studies.
Experiment: When possible, investigators should use RCTs for their studies.
Analogy: Scientists may consider the effect of factors similar to those under direct consideration, but this criterion, like plausibility, is weak.
These criteria are limited when myriad confounding variables exist that can be overlooked by those hoping that if an association exists, it is causal. Confounding variables can easily make a study's findings meaningless. Faulty conclusions due to confounders exist throughout modern society. These conclusions range from simple observations (e.g., factors that "cause" a car to be safe or vaccinations that "cause" autism) to conclusions from well-recognized scientists. Importantly, research on the impact of nutrient intakes on health outcomes involves the difficulties presented by confounders. The relative risks of relationships between nutrients and chronic diseases (such as cancer) can be very low, in the range of 1-2. Thus, if a confounding variable is the least-bit powerful, it can overwhelm the signals from the relative-risk measures. In the nutrition field, confounders can be powerful. People living in the United States have easy access to health care and often seek interventions to maximize their health. However, health outcomes improve in patients with access to high-quality healthcare regardless of whether these people use a dietary supplement, for example. Not unexpectedly, one of the primary weaknesses of observational data is confounding. If exposure is not determined by the equivalent of a coin toss, allocation to exposed and unexposed test groups likely risks confounding due to prejudices, fears, experiences, and many factors linked to personal choice. David Ransohoff at the University of North Carolina, Chapel Hill has put it best: observational studies are "guilty until proven innocent."
The further investigators move from using a disease as an outcome of interest and the more they rely instead on surrogates or intermediate markers, the less confident the research community can be of the intervention's benefits. When investigators find fewer deaths in one arm of a study than in another, experts in the field can be confident that the outcome is important. The demonstration of fewer deaths from a disease is strong evidence but requires the challenging and complicated task of interpreting and attributing the death to a disease, often using a death certificate.
In short, investigators sometimes only assess changes in risk factors rather than actual health outcomes. The literature offers examples where the discordance between an intermediate or surrogate measure and the outcome it was purported to substitute for led to false inferences, and these inferences resulted not only in the failure to realize a benefit but also the harms. Examples include studies of the cancer drug paclitaxel (Taxol®), the arrhythmia drug flecainide (Tambocor®), and the outcomes related to estrogen/progestin treatment revealed by the Women's Health Initiative.
The National Cancer Institute uses its Physician Data Query (PDQ) database to assess study design when staff determines whether an intervention can prevent cancer. But doing so is not enough. Focusing only on the hierarchy of study design is only one step in the process. It is possible to conduct poor RCTs and excellent observational studies. Questions to consider in assessing quality of evidence are:
Internal validity: Was the study well done?
Consistency: What is the volume of evidence and direction of effect?
Magnitude of effect: How great is the effect (preferably expressed as the absolute rather than relative effect)?
External validity: Can the effect be generalized to the general public or other settings?
When the PDQ panel integrated and reviewed the available data on vitamins/minerals in cancer, it concluded that the evidence of benefits is insufficient to support the use of multivitamin/mineral supplements or single vitamins or minerals to prevent cancer. Specifically for vitamin D, the overall body of evidence in humans indicates that at the doses studied (400-1,100 IU per day), vitamin D supplements do not reduce the overall risk of cancer.
Finally, I will close with a caution. We should be very rigorous in decision-making and data evaluation when making recommendations because, once a recommendation is made, the thinking of a population that has accepted the recommendation is difficult to shift. Furthermore, making recommendations not based on solid evidence impedes acquisition of new evidence and closes off pathways of discovery.
References
[1] Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58:295-300.
TRANSLATING EVIDENCE INTO GUIDELINES
Presenter: Victor M. Montori, M.D. Mayo Clinic
One goal of this presentation is to highlight the importance of making recommendations using a body of evidence that has been systematically synthesized, taking into account the trustworthiness of the evidence. A second goal is to emphasize that evidence alone never provides complete information on what to do. It is helpful to think of making recommendations as a series of three overlapping circles (Figure 1-4) that represent the research evidence, patient values and preferences, and the context in which people make decisions.
Figure 1-4. Overlapping components of recommendations development.
Basing recommendations solely on research data and ignoring either preferences and values or the context is not appropriate and results in a "tyranny" of evidence. However, people tend to frame disagreements in terms of data issues and research findings. Data are simply data, and disagreements are often due to differences in values, preferences, and goals as well as the context in which people make decisions. It is important to provide language for describing these types of disagreements.
General Principles for Building a Recommendation
An underlying principle of evidence-based medicine is that the body of evidence is the focus. Clinicians do not make decisions on the basis of a single published report or a subset of available data. Use of the body of evidence requires a systematic synthesis of the data. Those making evidence-based recommendations seek trustworthy evidence because they can be more confident in the accuracy of the outcome measures and, thereby, in their ability to use the data to guide care.
Developers of clinical recommendations establish evidence trustworthiness by considering several factors:
Study design: Randomized controlled trials (RCTs) provide the highest quality of evidence and are at the top of the evidence pyramid (see Figure 1-3). Observational studies are lower down in the evidence hierarchy. Despite the high quality of data that can be generated by RCTs, some factors may decrease the confidence that experts can place in these data. The first factor is imprecision. If investigators observe few events and they have wide confidence intervals, the precision is insufficient to determine how real these events may be. The next factor is the risk of bias. Measurement error is a component of risk of bias and may be due to lack of blinding, failure to conceal allocation, or inappropriate allocation of participants. Loss to follow-up can also lead to risk of bias, and publication bias is an additional concern.
Consistency of results: Differences in effect size that cannot be explained by differences in components of the study decrease confidence in the data. Statistical confidence intervals can also overlap, and statistical tests may identify inconsistencies not due to chance.
Directness: Directness pertains to the applicability of the outcomes to the question of interest. Directness is limited, for example, when a study's outcomes are valid and of high quality but are not generalizable to the population of interest. The existing studies might, for example, focus on older persons with several diseases and therefore not be directly relevant for a panel developing a recommendation for a young, healthy population. Likewise, the nature of the interventions may limit directness. For example, the same substances might not be administered in practice in the same amounts and in the same way as in the studies. Furthermore, the use of surrogate or intermediate markers can affect directness if the intermediate marker or outcome has not been established as a valid substitute for the actual outcome of the intervention. The intermediate marker or outcome must not be extrapolated from another intervention because this can result in indirectness. For example, a panel might want to compare the effects of vitamin D2 and vitamin D3 on a particular outcome, but the only studies available compare vitamin D2 or vitamin D3 to a placebo, resulting in only indirect comparisons of vitamin D2 to D3.
Dose-response relationship: Confidence in a causal effect is higher if a dose-response measure is used.
Recommendations developers must evaluate the outcome of interest by determining how it behaves within the entire body of evidence. They must not only consider how confident they are in the estimates of the effect, but also take into account values and preferences, benefits and harms, and resource implications. For values and preferences, for example, if every participant in this meeting received information about the relative effectiveness of statins (e.g., the proportions of 100 people that might or might not benefit), their preferences regarding statin therapy might vary, even though they have similar educations and work in healthcare.
Several contextual concerns must also be considered. Recommendations developers must balance benefits and harms by considering, for example, whether an effect closely matches important benefits and harms or whether the relationship between the effect, benefits, and harms is unknown or unclear because the evidence is of low quality. Context also includes resource implications. The figures for vitamin D laboratory testing and supplement use are staggering. The uncertainty or certainty surrounding the available research outcomes on vitamin D cannot be ignored. Conclusions about the strength of the evidence can temper or inform these types of judgments. Stronger evidence may provide better justification for ignoring resource limitations, for example.
It is possible to characterize the milieu that surrounds a strong recommendation versus a weak one. A strong recommendation is associated with situations in which almost everyone with the disease or condition would like to receive the intervention, most of these people should receive the intervention, and the recommendation can serve as a policy. A weaker recommendation is associated with situations in which many people with the disease would like to receive the intervention, but many would not. There is an opportunity for shared decision-making between clinicians and patients about which option is consistent with patients' informed preferences. Weaker recommendations are not well suited for policy, and policy activities stemming from such recommendations require extensive and broad consultation.
Application of GRADE Approach
The approach known as GRADE (Grades of Recommendation, Assessment, Development, and Evaluation) specifies four levels of quality: high, moderate, low, and very low. It is conducted using seven steps:
Identify the clinical question
Rank the importance of each outcome
Collect and analyze the evidence
Rate the quality of evidence for each outcome
Assess the overall quality of the evidence
Craft a recommendation
Grade the strength of the recommendation
GRADE defines the quality of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the quantity of interest. The GRADE process includes the identification of the outcome that is most important, such as mortality. Outcomes that patients report are important and outcomes based on laboratory tests are less important. After the recommendations developers assess the quality of the evidence in relation to the outcome, they craft a recommendation. In the absence of very high-quality evidence, the weakest link in the causal pathway must drive the recommendation. The group grades the recommendation based on the strength of the evidence but also on the basis of values, preferences, risk/benefit ratios, and resource implications.
An example of the GRADE approach is the review of the effect of vitamin D on falls by Murad and colleagues for the Endocrine Society [1]. This systematic review initially found 26 trials related to the outcome. However, as the risk-bias assessment suggested, about half of the studies did not meet quality criteria for confidence, and some had significant loss to follow-up. A meta-analytical plot (Figure 1-5) shows an inconsistency between the outcomes. Some studies showed that the intervention was beneficial (right side of dark vertical bar) and others did not (left side of dark vertical bar). The pooled- estimate odds ratio was 0.86 (indicating no difference) and had a confidence interval of 0.77 to 0.96.
The i2 statistic, which measures the degree of uncertainty, was 66% when it should have been 0%. The initial vitamin D status of study participants and co-administration of calcium partially explained the inconsistency.
Figure 1-5. Plot of odds ratios derived from meta-analysis of relationship between vitamin D and falls. Source: [1].
Most people would say that confidence in the science supporting the relationship between vitamin D and falls is, at best, moderate. There are randomized trials with moderate risk of bias and a moderate treatment effect but with wide confidence intervals. In addition, many of these studies appear to suffer from publication bias. The evidence overall is most relevant to individuals who have high rates of falls.
However, in making a vitamin D recommendation, other factors came into play for the Endocrine Society [2]. The recommendations developers decided to place a low value on avoiding vitamin D cost and resource implications and on the likelihood of toxicity at the recommended levels. However, they placed a high value on achieving benefits. In the end, they made a strong recommendation for supplementation of 800 IU per day for women aged 65 years and older. That is, they were willing to hold healthcare providers accountable for implementing this recommendation, but they also specified that it was based on low-quality/low-confidence evidence.
This outcome illustrates the likelihood that disagreements here and elsewhere in recommendations making are less likely to be about the nature of evidence than about other factors. Benefits of the approach described in this presentation are that the considerations taken into account can be separated and disagreements can be discussed appropriately and constructively.
References
Murad MH, Elamin KB, Abu Elnor KO, et al. Clinical review: the effect of vitamin D on falls: a systematic review and meta-analysis. J Clin endocrinol Metab. 2011;96(10):2997-3006.
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30.
REVISED CRITERIA FOR THE NATIONAL GUIDELINE CLEARINGHOUSE
Presenter: Mary P. Nix, M.S., P.M.P. Agency for Healthcare Research and Quality
The National Guideline Clearinghouse (NGC) is a database of evidence-based clinical practice guidelines and related documents maintained as a public resource by the Agency for Healthcare Research and Quality (AHRQ). NGC provides an accessible mechanism for obtaining objective, detailed information on clinical practice guidelines and furthers their dissemination, implementation, and use.
Like electronic libraries, NGC serves as a repository. An editorial board of experts helps lead NGC, and these experts are important links to the communities that NGC serves. NGC represents more than 200 organizations that develop guidelines. Currently, NGC houses more than 2,700 guidelines and receives more than 400,000 visits per month. More than 90,000 people subscribe to NGC's weekly emails. To help users determine which guidelines might be relevant to their interests, NGC creates structured summaries of the guidelines.
Unfortunately, many people assume that NGC vets the guidelines that it stores. That is, there has been a prevailing belief that a guideline is "good" if it is available in NGC. This conflicts with NGC's purpose, which is to make existing guidelines widely available and allow users to determine the quality and appropriateness of the guidelines. NGC does not endorse, approve, develop, or implement guidelines. In short, it does not appraise guideline quality. However, stakeholder input has suggested that NGC should be more selective in choosing which guidelines to add to its collection.
Until recently, NGC's criteria for inclusion had been based on criteria established in 1997. As a result of the issues mentioned above, the age of NGC's inclusion criteria, and the Institute of Medicine's (lOM's) 2011 definition of evidence-based clinical practice guidelines [1], AHRQ recently developed new criteria for adding guidelines to NGC. These revised criteria establish the foundation for a related effort to indicate the extent to which each guideline adheres to the 2011 IOM "trustworthy guideline standards."
AHRQ's starting point in developing its new NGC guidelines was the IOM definition of a clinical practice guideline: "statements that include recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options." The main differences between the 1997 and 2013 criteria are the addition of a new criterion and added specificity to two criteria (Table 1-1). According to the new criterion, clinical practice guidelines must contain an assessment of benefits and harms of recommended care and alternative care options. Importantly, the new criterion stipulates not just that care options be recommended, but also that other options be considered and their benefits and harms conveyed.
TABLE 1-1. Comparison of Original and Revised National Guideline Clearinghouse Criteria
While a systematic review must now underpin each guideline included in the NGC, the NGC does not exclude a guideline if a systematic review identified gaps in the evidence base for some of the recommendations. The key components of a systematic review as recognized by NGC are:
An explicit statement that the clinical practice guideline was based on a systematic review
A description of the search strategy that includes a listing of database(s) searched, a summary of search terms used, the specific time period covered by the literature search including the beginning date (month/year) and end date (month/year), and the date(s) when the literature search was done
A description of study selection that includes the number of studies identified, the number of studies included, and a summary of inclusion and exclusion criteria
A synthesis of evidence from the selected studies, e.g., a detailed description or evidence tables
A summary of the evidence synthesis included in the guideline that relates the evidence to the recommendations, e.g., a descriptive summary or summary tables.
AHRQ announced the revised criteria in 2013 and began implementing them in June 2014. Between June and December 2014, NGC had added 62 guidelines meeting the 2013 criteria. Users can now apply a search filter to identify only the guidelines that meet the new criteria. Because of funding limitations, AHRQ was unable to re-review the entire database. As a result, AHRQ retained or "grandfathered" all guidelines in NGC prior to June 2014, regardless of whether they met the 2013 criteria. The new search filter for guidelines meeting the criteria, therefore, does not pull out the "grandfathered" guidelines that could meet the 2013 criteria.
AHRQ is eager to help developers produce clinical practice guidelines that are supported by systematic reviews and can be added to NGC. By establishing its new criteria and working actively with its stakeholders, AHRQ hopes to support the realization of significant advances in clinical care quality and public health.
References
[1] Institute of Medicine. Clinical Practice Guidelines We Can Trust. Washington, DC: The National Academies Press; 2011.
DEVELOPMENT OF ENDOCRINE SOCIETY GUIDELINES – Holick
Presenter: Michael F. Holick, Ph.D., M.D. Boston University
The purpose of this presentation is to describe the process that the Endocrine Society used to develop its recent recommendations regarding the evaluation, treatment, and prevention of vitamin D deficiency [1] with an emphasis on the care of patients at risk of deficiency.
Overall, a systematic review of evidence coupled with discussion guided the process. A task force prepared a draft set of recommendations for review by the Endocrine Society Clinical Practice Guidelines Subcommittee, the Clinical Affairs Core Committee, and co-sponsoring associations. The task force examined the conclusions of the Institute of Medicine (IOM) about vitamin D, particularly the lOM's 2011 report on dietary reference intakes for vitamin D [2]. As that report points out, its purpose was not to direct physicians or provide clinical guidelines, a responsibility of professional associations. Instead, the IOM focused on a population model, rather than a medical model, and it accordingly is not surprising that the conclusions of the Endocrine Society experts and those of the IOM may differ.
Diet and Sunlight
The 2011 IOM report said that people can obtain vitamin D from their diet. However, vitamin D is rare in foods, so people must consume very large amounts of fortified dairy products, fortified orange juice, or fish to obtain the daily values that the IOM recommended. A 2004 study showed that no one in the United States obtains enough vitamin D from foods or supplements to satisfy requirements [3].
The IOM said that sunlight has only a small effect on vitamin D status. However, the Endocrine Society concluded that sunlight plays a significant role in producing vitamin D. Studies in the United States and in Denmark show that blood levels of 25(OH)D peak at the end of the summer, and the nadir is at the end of winter [4,5]. A recent study found that people living in southern areas have fewer differences in vitamin D concentrations between summer and winter than people living in northern regions, and parathyroid hormone (PTH) levels mirror these seasonal changes (Figure 1-6). This leads to the important question of whether it is healthy for PTH levels to fluctuate seasonally.
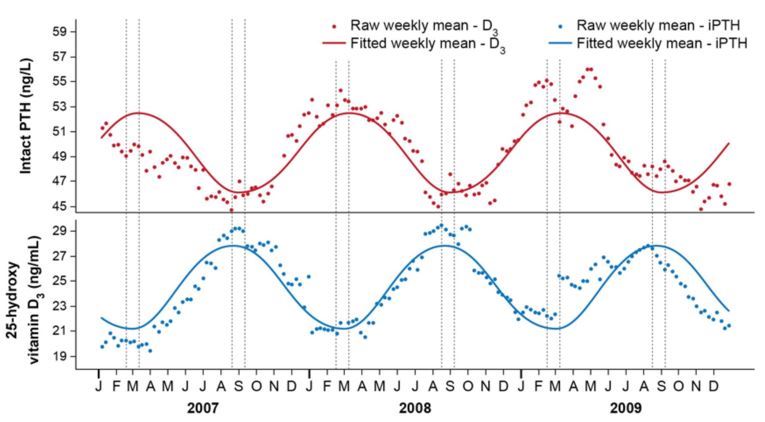
FIGURE 1-6. Changes in serum 25-hydroxyvitamin D concentrations and intact parathyroid hormone (iPTH) concentrations across seasons in northern regions.
Source: [5]
Measures of Status and Metabolic Bone Disease
Researchers generally agree that serum 25(OH)D concentration is a better measure of vitamin D status than concentrations of the other active metabolites of vitamin D. In 1998, after the IOM established the vitamin D deficiency cutoff as a 25(OH)D concentration less than 11 ng/mL [6], a study clarified that vitamin D deficiency occurs when serum values are less than 20 ng/mL based on declining PTH levels and secondary hyperparathyroidism [7]. In addition, Priemel and colleagues showed that vitamin D supplementation needs to restore circulating levels of 25(OH)D to 30 ng/mL to maintain skeletal health [8]. The study also found that 24% of otherwise healthy German adults who had blood concentrations of 25(OH)D of 21-29 ng/mL had evidence of osteomalacia. The Endocrine Society task force disagreed with the IOM's interpretation of these data—that a serum level of 20 ng/mL was associated with no evidence (<1% prevalence) of osteomalacia or metabolic bone disease due to vitamin D deficiency. The task force concluded that 25(OH)D serum concentrations of 30 ng/mL or above is necessary to avoid deficiency and support bone health, based in part on the Priemel study findings.
Upper Limits of Intake
The 2011 IOM report established a tolerable upper intake level (UL) of 4,000 IU of vitamin D per day for persons older than 8 years and lower levels for younger children. Doctors have been extremely concerned about the risk of vitamin D intoxication. However, Robert Heaney of Creighton University showed that healthy males taking 10,000 IU per day for 5 months experienced no adverse effects [9]. Reinhold Vieth of the University of Toronto confirmed the safety of 10,000 IU per day [10]. A recent study suggests that even 15,000-20,000 IU per day does not increase serum 25(OH)D levels to 100 ng/mL, the concentration that reflects an upper limit of intake [11]. For infants, 2,000 IU per day or
IU once a week for 6 weeks is not associated with adverse effects [12]. In pregnant women, up to
IU per day increases serum 25(OH)D levels to approximately 50 ng/mL without changing serum or urinary calcium levels [13].
Non-skeletal Benefits of Vitamin D
Essentially every cell in the human body has a vitamin D receptor, and researchers want to know why they are present. This interest led the Endocrine Society task force to consider non-skeletal benefits of vitamin D in people with deficiency. The benefits that the task force identified ranged from reduced cancer risk to improved immune function (e.g., production of proteins to kill infectious agents and a reduced risk of influenza) and links between serum 25(OH)D concentration and risk of upper respiratory tract infections. Other possible benefits included reduced risk of type 1 and type 2 diabetes, multiple sclerosis, neurocognitive dysfunction, cardiovascular disease, and hypertension. However, although a great deal of data suggests that vitamin D deficiency is linked to all of these chronic illnesses, most of the studies were not randomized controlled trials (RCTs). For this reason, the task force noted the findings but did not make recommendations based on them.
Two systematic reviews were conducted to assist the task force in developing the vitamin D guidelines. These reviews focused on falls, pain, quality of life, and cardiovascular outcomes. Based on the results, the task force concluded that the relationship between vitamin D supplements and cardiovascular disease benefits could not be supported, and it made no recommendation to screen people for vitamin D deficiency because of cardiovascular concerns.
However, there was sufficient evidence for the Endocrine Society to recommend giving vitamin D supplements to prevent falls because vitamin D deficiency causes proximal muscle weakness and is important for muscle strength. A small RCT showed that among nursing home residents, taking 800 IU of vitamin D for 5 months reduced the number of falls by 72% [14]. A European study showed that vitamin D status predicts physical performance and decline in older persons at serum 25(OH)D concentrations of 30 ng/mL [15], which seems to be the appropriate level for many associated health benefits of vitamin D.
Mortality risk is also of interest. Early studies suggested a 7% reduced risk of mortality based on better vitamin D status, and a more recent study indicated a reduced risk of up to 25% for all-cause mortality if vitamin D status improves [16]. Furthermore, a range of studies have shown significantly decreased mortality rates at serum 25(OH)D concentrations of 40-50 ng/mL. The IOM concluded, however, that while very low vitamin D status increases the risk of all-cause mortality, levels of 30 ng/mL or higher also increase the risk (i.e., the "J curve"). A study by Melamed and colleagues, which the IOM cited, showed that serum 25(OH)D concentrations of 30-49 ng/mL, on average, were associated with decreased mortality rates, and increased mortality the risk might have been only for women.
The IOM might have misinterpreted the J curve. To determine whether the slight increase in mortality rates associated with 25(OH)D blood levels higher than 50 ng/mL was due to appropriate treatment of chronic vitamin D deficiency with pharmacologic doses or lifetime excessive intakes, a study used data on 3.8 million laboratory test results to detect the presence of 25(OH)D2, a marker of vitamin D2 levels [5]. Patients with 25(OH)D2 were being treated for deficiency because foods and most over-the-counter supplements do not contain vitamin D2. Of study participants with serum concentrations of 25(OH)D higher than 50 ng/mL, 59% had detectable levels of 25(OH)D2 and thus were likely being treated for vitamin D deficiency. Conclusions from the J curves that achieving blood levels of 25(OH)D higher than 30-50 ng/mL increases risk of cardiovascular disease, prostate cancer, pancreatic cancer, other chronic illnesses, and mortality should be re-evaluated.
Recommended Intake Levels
The 2011 IOM report recommended fixed amounts of vitamin D intakes for various age groups ranging from 400 to 800 IU per day. The approach that the IOM used to develop these recommendations has been challenged. Some scientists have suggested that curvilinear analyses that incorporate study averages, fitted dose-response relationships, 95% prediction limits, and study averages minus two standard deviations may be more relevant than the IOM's approach to setting an intake recommendation. With the approach of these scientists, if 2,000 IU vitamin D per day results in 25(OH)D serum levels of about 30 ng/mL and the goal is to cover 97.5% of the population, the intake probably needs to be approximately 5,000-7,000 IU per day. There are suggestions that the IOM made a statistical error in estimating the recommended intake for vitamin D.
From the Endocrine Society's perspective, ranges for recommended intakes are better than absolute amounts. The literature has sufficient evidence to support the society's intake recommendations (Table 1-2).
TABLE 1-2 . Endocrine Society Vitamin D Intake Recommendations and Upper Limits [Source: [1]
Summary
The Endocrine Society recommends screening persons at risk of vitamin D deficiency and the use of serum 25(OH)D concentrations as a measure of status. The society does not recommend population screening.
The society concluded that vitamin D deficiency is very common in all age groups. Because few foods contain vitamin D, it recommended supplementation at suggested daily intake levels and within ULs depending on age and clinical circumstances. The goal should be to achieve a 25(OH)Dconcentration of at least 30 ng/mL; the preferred range is 40-60 ng/mL, and up to 100 ng/mL is the upper limit of normal (Figure 1-7). However, patients with hypersensitivity to vitamin D, including those with granulomatous disorders, require a physician's guidance about taking vitamin D supplements to prevent hypercalcemia.
Deficiencies should be treated with vitamin D3 or D2. Maintenance of vitamin D status should include a three-part strategy consisting of increased intakes of foods containing vitamin D, sensible sun exposure, and vitamin D supplementation.
The Endocrine Society recognized that the evidence was insufficient to suggest that improvement in vitamin D status reduces risk of many chronic illnesses. However, the society did not ignore the multitude of epidemiologic and association studies showing reduced risk of acute and chronic illnesses with supplementation. The society concluded that increasing vitamin D intakes in both children and adults to its recommended levels has no downside.
References
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30.
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Moore C, Murphy MM, Keast DR, Holick MF. Vitamin D intake in the United States. J Am Diet Assoc. 2004,104(6) :980-3.
Brot C, Vestergaard P, Kolthoff N, et al. Vitamin D status and its adequacy in healthy Danish perimenopausal women: relationships to dietary intake, sun exposure and serum parathyroid hormone. Br J Nutr. 2001,-86 Suppl 1:S97-103.
Kroll MH, Bi C, Garber CC, et al. Temporal relationship between vitamin D status and parathyroid hormone in the United States. PLoS One. 2015;10(3):e0118108.
Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academy Press; 1997.
Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351(9105):805-6.
Priemel M, von Domarus C, Klatte TO, et al. Bone mineralization defects and vitamin D deficiency: histomorphometric analysis of iliac crest bone biopsies and circulating 25-hydroxyvitamin D in 675 patients. J Bone Miner Res. 2010;25(2):305-12.
Heaney RP, Davies KM, Chen TC, et al. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77(1):204-10.
Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69(5):842-56.
Ekwaru JP, Zwicker JD, Holick MF, et al. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One. 2014;9(11):e111265.
Gordon CM, Williams AL, Feldman HA, et al. Treatment of hypovitaminosis D in infants and toddlers. J Clin Endocrinol Metab. 2008;93(7):2716-21.
Hollis BW, Johnson D, Hulsey TC, et al. Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res. 2011;26(10):2341-57.
Broe KE, Chen TC, Weinberg J, et al. A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. J Am Geriatr Soc. 2007;55(2):234-9.
Wicherts IS, van Schoor NM, Boeke AJ, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007;92(6):2058-65.
Thomas GN, ó Hartaigh B, Bosch JA, et al. Vitamin D levels predict all-cause and cardiovascular disease mortality in subjects with the metabolic syndrome: the Ludwigshafen Risk and Cardiovascular Health (LURIC) Study. Diabetes Care. 2012;35(5):1158-64.
APPLYING SYSTEMATIC REVIEWS TO DIETARY REFERENCE INTAKES: VITAMIN D AS A CASE STUDY
Presenter: Patsy M. Brannon, Ph.D., R.D. Cornell University
This presentation examines the use of systematic evidence-based reviews to develop recommendations for nutrient intakes for the 2011 dietary reference intakes (DRIs) for vitamin D [1].
The challenges include considering the totality of the evidence, addressing uncertainties, and integrating the reviews into the larger process for developing recommendations.
Background: Dietary Reference Intakes
The DRIs are nutrient reference values issued by the Institute of Medicine (IOM) of the National Academies. Unlike a model in which a cut-point value is set and clinicians work to ensure that their patients have a nutrient level above that cut-point, the DRIs take into account that human requirements have a distribution of values around a mean rather than a single value. In this sense, the DRIs reflect a population model.
Establishing DRIs requires identifying the distribution of requirements for the population, determining the average or median requirement, and specifying the level along the distribution of requirements at which the needs of most of the population—the 97.5th percentile of the distribution- are surpassed. The distribution is based on a health outcome for the nutrient along with its relevant dose-response relationship. The point at which intakes (or a biomarker of exposure) are associated with an increased risk of adverse effects is also determined.
Systematic evidence-based reviews assist in establishing the cause-and-effect relationship between the nutrient and health outcomes (both beneficial and adverse). They are also useful in determining dose-response relationships.
Overall, DRIs reflect the U-shaped risk curve commonly associated with nutrient effects, as shown in Figure 1-8. Health-related risks are associated with intakes of the nutrient that are too low or too high. Generally, above even the highest nutrient requirement there is a range of safe and adequate intakes before the risk of adverse effects from excessive intakes begins to arise.
FIGURE 1-8. Dietary Reference Intakes as a reflection of distribution of risk.
Source: Modified from Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: The National Academies Press; 2006.
In the case of the 2011 DRIs for vitamin D, an important aspect of the deliberations of the IOM review committee was the use of a risk assessment model. In effect, the determination of human requirements and adverse effects from excessive exposure involves an analysis of the risk of intakes that are both too low and too high. The risk assessment model stipulates consideration of the totality of the evidence and transparency in decision-making. For this reason, the development of objective and independent data reviews reflecting the totality of the evidence were essential in informing the IOM committee and serving as a starting point.
Incorporation of Systematic Reviews of Evidence
The IOM committee used two systematic reviews from evidence-based practice centers sponsored by the Agency for Healthcare Research and Quality (AHRQ)—one that the Ottawa Evidence- based Practice Center published in 2007 on vitamin D and bone health, and one from the Tufts Evidence-based Practice Center in 2009 on health outcomes of vitamin D and calcium [2,3]. Data methodologists in these two centers, as in all AHRQ-sponsored evidence-based practice centers, objectively evaluate the evidence to inform committee deliberations by answering questions from relevant experts prior to the review.
Systematic evidence-based reviews are extremely useful in reducing bias, but they cannot automate the decision-making process, relegate decision-making to computer models, or replace expert judgment. The AHRQ reviews served as an important foundation and were coupled with additional literature searches and evaluations, expert opinion, and scientific judgment.
Both centers used well-recognized grading systems. The Ottawa group assessed the quality of individual studies using the Jadad criteria for RCTs and a combination of the Harris and U.S. Preventive Services Task Force (USPSTF) grading systems for observational studies. The Tufts group used a three- grade quality scale for all studies. The Ottawa review examined subpopulations of interest to DRI development and total exposure levels that accounted for vitamin D intakes from the diet, sun exposure, and food. The review incorporated intermediate biomarkers and surrogate health outcomes and took into account measures of serum 25(OH)D in relation to bone health. The Tufts review focused on a range of health outcomes in addition to bone health. It was based on two analytic frameworks— one that addressed deficiency and adequacy relative to the nutrient and the health outcomes, and another that focused on adverse outcomes relative to vitamin D excess or toxicity.
Totality of Evidence
To determine the health outcome that would serve as the basis for the DRI for vitamin D, the IOM committee first considered the data on the relationship between vitamin D and all of the health outcomes in the literature regardless of the nature of that evidence. Ultimately, the committee considered over 25 health outcomes. The conclusions in the literature reviews for many of these outcomes appeared to be derived from a subset of selected studies rather than the totality of the evidence. The committee determined that RCTs provided the greatest level of confidence, but it also considered outcomes from observational studies. This comprehensive examination of the entire dataset required an evaluation of data quality and strength, identification of consistency of effect, and searches for confounding factors.
The committee considered a wide array of possible health outcomes for vitamin D, including:
Cancer/neoplasms: all cancers, breast cancer, colorectal/colon polyps, pancreatic cancer, and prostate cancer
Cardiovascular diseases and hypertension
Weight, diabetes (type 2), and metabolic syndrome
Immune functioning: asthma, autoimmune diseases (eczema, type 1 diabetes, inflammatory bowel and Crohn's disease, multiple sclerosis, rheumatoid arthritis, systemic lupus erythematosus), and mortality due to infectious diseases (tuberculosis and influenza/upper respiratory infections)
Neuropsychological function: autism, cognitive function, and depression
Pregnancy: preeclampsia, hypertension, preterm birth, low birth weight, and infant mortality
The AHRQ systematic reviews were an important basis for the IOM committee's conclusions overall. However, the committee recognized that some useful studies had been published after the completion of these reviews and that several relevant studies did not meet the inclusion criteria for the AHRQ analyses. The committee considered these data in its deliberations.
The committee determined that the evidence was insufficient to establish a link between vitamin D and health outcomes other than bone health. The reasons for this determination were that the evidence failed to demonstrate causality, research outcomes were contradictory, and there was no consistency of effect. For example, the data for all cancers was inconclusive, and data on specific types of cancers showed trends in opposite directions. The risk of some cancers in response to vitamin D supplementation trended toward an increased risk, whereas the risk of others trended toward a decrease.
Given the IOM committee's conclusion that only bone health outcomes could be demonstrated to have a causal link to vitamin D exposures, the committee focused on specifying a dose-response relationship between serum 25(OH)D concentrations and bone health. Serum 25(OH)D is known to reflect intake, and newer studies have enabled linkages between vitamin D intakes and changes in serum 25(OH)D concentrations under minimal sun exposure. The measures that the committee integrated to reflect bone health were calcium absorption, bone accretion (including bone mineral content/density and rickets), bone maintenance (including bone mineral density and osteomalacia), and bone loss (including fracture risk).
The types of summaries from systematic evidence-based reviews that were important to the committee's conclusions for fractures are highlighted in Table 1-3. Although the committee judged the evidence to be "good" in relation to the connection between serum 25(OH)D and fractures, it was not strong. Other evidence gleaned from the AHRQ reviews indicated that calcium absorption was enhanced only when serum 25(OH)D levels were quite low (<12.5 nmol/L); a linear relationship between serum 25(OH)D and calcium absorption could not be demonstrated. Data supported the conclusion that bone mineral content increases with vitamin D exposure in children but were only fair for adults.
TABLE 1-3. Evidence for Relationship Between Vitamin D Exposure and Fractures: Example of Good But Not Strong Evidence [Source: [3]
Compiling and integrating data such as these led the IOM committee to conclude that the strongest evidence linked a concentration of 16 ng/mL (40 nmol/L) serum 25(OH)D to an average requirement for bone health. The committee had no reason not to assume that the average requirement was normally distributed. Therefore, based on a two-standard-deviation calculation, the level that surpassed the need for 97.5% of the population was 20 ng/mL (50 nmol/L). Although some studies may have suggested a higher average requirement and some studies a lower one, the weight of the totality of the evidence rested on a 16 ng/mL (40 nmol/L) concentration.
Determining a serum concentration at which the risk of adverse events increases was more challenging because few, if any, data could be derived from clinical trials for obvious ethical reasons. Therefore, the body of evidence was largely based on observational studies. Beyond the classic hypercalcemia and hypercalciuria measures, which reflect extreme vitamin D toxicity, the IOM committee took into account the emerging evidence on all-cause mortality along with evidence on cardiovascular disease, falls, and fractures associated with high vitamin D exposures. Such observational studies are subject to confounding effects. However, they often provide the only available data on adverse effects.
Because of its desire to err on the side of caution and safety, the IOM committee used these observational data while acknowledging that frank toxicity causing kidney and liver damage or even death might occur at much higher levels. Adverse events (e.g., all-cause mortality and cardiovascular disease) became more common at vitamin D levels of 30-48 ng/mL (75-125 nmol/L). Therefore, the committee established upper levels of intake that would keep serum concentrations from surpassing 48 ng/mL (125 nmol/L).
Finally, the IOM committee's experience with systematic evidence-based reviews for establishing a DRI underscored the often-made point that careful specification of the a priori questions for the evidence review is important for the successful contribution of these reviews to recommendations development. Persons knowledgeable about the needs and application of the review should be involved in these important stage-setting activities. Furthermore, an evidence review can use meta-analyses to combine data and expand overall understanding. However, in the end, evidence reviews of any kind are only as relevant as the available studies. In the case of nutrition in general and vitamin D in particular, studies that focus on dose-response relationships are often lacking.
References
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Cranney A, Horsly T, O'Donnell HA, et al. Effectiveness and Safety of Vitamin D in Relation to Bone Health. Evidence Report/Technology Assessment Number 158. Rockville, MD: AHRQ; 2007. http://archive.ahrq.gov/downloads/pub/evidence/pdf/vitamind/vitad.pdf.
Chung ME, Balk M, Brendel M, et al. Vitamin D and Calcium: A Systematic Review of Health Outcomes. Evidence Report/Technology Assessment Number 183. Rockville, MD: AHRQ; 2009. http://www.ahrq.gov/downloads/pub/evidence/pdf/vitadcal/vitadcal.pdf.
U. S. PREVENTIVE SERVICES TASK FORCE: SCREENING FOR VITAMIN D DEFICIENCY IN ADULTS
Presenter: Michael L. LeFevre, M.D., M.S.P.H. University of Missouri
This presentation describes the U.S. Preventive Services Task Force (USPSTF) and its recent report, Screening for Vitamin D Deficiency in Adults [1]. Understanding the process helps clarify the conclusions and recommendations generated by USPSTF reviews.
U.S. Preventive Services Task Force Approach
The goal of preventive services, and thus of the USPSTF evidence-based recommendations, is to improve population health by reducing the risk of future suffering or adverse conditions and to prolong life. Preventive services do not focus on relieving current suffering or adverse conditions. Therefore, the USPSTF recommendations address screening tests, counseling, and preventive medications in, or as a result of referrals from, primary care settings.
The panel of experts that develop USPSTF recommendations are volunteers. Congress has authorized the Agency for Healthcare Research and Quality (AHRQ) to provide administrative, scientific, technical, and dissemination support to the USPSTF. However the USPSTF remains an independent body. ARHQ maintains evidence-based practice centers that assess the existing research for the USPSTF. The panels represent disciplines in primary care and do not include clinical specialists. Therefore, the USPSTF panels are ideally suited to make unbiased assessments of the science.
Figure 1-9, a generic USPSTF analytic framework for screening services, highlights several important aspects of the USPSTF process. The process begins (left side of figure) with asymptomatic, not diseased, persons at risk of the disease in question. A panel assesses the link between the evidence and the outcome of morbidity and/or mortality (right side of figure). USPSTF panels rarely use intermediate outcomes as a basis for their recommendations. The analytic framework reflects a tenet (or perhaps a bias) of the USPSTF that it is impossible for someone who is asymptomatic to improve, or to make a healthy person better. Therefore, the evidence bar for subjecting healthy people to interventions with possible harms must be high.
FIGURE 1-9. USPSTF's generic analytic framework for disease screening
Even with rigorous data reviews, judgment is involved in making USPSTF recommendations. The panels must assess the certainty and magnitude of the estimated benefits and harms, the balance between them, and the magnitude of the net benefit. At the end of the process, as shown in Table 1-4, either the panel finds the evidence sufficient and assigns a letter grade to the recommendation for practice based on both the certainty and magnitude of the net benefit, or it finds the evidence insufficient and assigns the topic a grade of "I."
TABLE 1-4. USPSTF Grades of Evidence
USPSTF Recommendations on Screening Adults for Vitamin D Deficiency
The USPSTF report on the benefits of screening asymptomatic adults for vitamin D deficiency used the process described above. The USPSTF vitamin D panel compared the certainty of a net benefit from screening to the outcomes of decreased morbidity, reduced mortality or disability, and improved psychosocial outcomes (Figure 1-10). The panel concluded that the evidence was insufficient and assigned it a grade of "I." In short, whether the benefits of screening asymptomatic adults for vitamin D deficiency outweigh the harms is not known.
FIGURE 1-10. USPSTF analytic framework for vitamin D deficiency screening. Source: [1].
The USPSTF process for evaluating vitamin D screening began with the specification of the study inclusion criteria (Table 1-5). The panel included studies with varying definitions of vitamin D deficiency but required that 90% of the study populations have a serum 25(OH)D concentration lower than 30 ng/mL. The interventions that the panel included were supplementation with vitamin D alone or with both vitamin D and calcium, and the outcome had to be reported at 8 weeks or longer after the intervention ended. The panel identified the relevant health outcomes based on those addressed in published studies, and included those shown in Table 1-5.
TABLE 1-5. USPSTF Inclusion Criteria for Vitamin D Supplementation Studies
Study
Characteristic
Inclusion Criteria
Population3
Adults (18 years or older) with vitamin D deficiency but no symptoms of vitamin D deficiency
No medical condition for which vitamin D might be used as treatment (e.g., osteoporosis or chronic kidney disease)
90% of study population had 25(OH)D concentrations of 30 ng/mL or lower
Intervention
Vitamin D alone
o Vitamin D versus placebo or no treatment
Vitamin D and calcium
o Vitamin D and calcium versus placebo or no treatment o Vitamin D and calcium versus calcium
Design
For benefits: Systematic evidence reviews, RCTs, and case-control studies embedded in RCTs
For harms: Systematic evidence reviews, RCTs, cohort studies, and case- control studies
Setting
• Relevant to primary care, generalizable to U.S. population
Benefitsb
Decreased morbidity from osteoporosis/fractures, falls, diabetes mellitus, cardiovascular disease, cancer, and immune diseases
Reduced depression and improved psychosocial functioning
Improved physical fitness capacity or performance and physical functioning
Reduced disability
Reduced mortality
Harms
• Adverse events (e.g., gastrointestinal or renal outcomes, hypercalcemia, or kidney stones)
a Studies defined vitamin D deficiency in different ways. b Studies reported outcomes at least 8 weeks after start of intervention. Note: RCTs = randomized controlled trials.
For this review, USPSTF asked whether it is possible to screen people for vitamin D deficiency, identify those who have deficiency, give them vitamin D supplements, and improve their health. An important consideration was the accuracy of screening tests. Although this was not an a priori key question, the review process identified unresolved questions about what to measure when screening adults for vitamin D deficiency and how best to measure it. Almost all studies to date measured 25(OH)D bound by vitamin D-binding protein, so this measure was the only available basis for the USPSTF recommendations.
Researchers measure serum 25(OH)D analytically using various methodologies, and these different methodologies do not provide quantitatively similar results. For this reason, the field of study clearly needs a vitamin D reference material. For the USPSTF report, these potential quantitative differences would have been important if the data review had revealed studies with a mix of positive and negative outcomes. However, the consistent conclusions among the studies made this potential concern somewhat moot.
The field has no established or generally accepted definition of "normal" for measures of serum 25(OH)D concentrations, and investigators have used different definitions. Therefore, the studies that the USPSTF panel reviewed treated study participants and determined study goals based on different serum 25(OH)D concentrations. The panel responded to this challenge by accepting the definitions that the authors of each study used.
As the USPSTF report shows, none of the reviewed studies had evaluated the effects of screening on health outcomes or harms to answer the questions for tasks 1 and 2 in Figure 1-9. Therefore, the panel proceeded through the middle of the analytic framework using the question of whether treatment with vitamin D supplements leads to improved health outcomes or adverse effects.
The panel concluded that the evidence was adequate to show no benefit of vitamin D supplementation for preventing cancer, type 2 diabetes, mortality in community-dwelling adults, or fractures in persons without a high risk of fracture. The evidence was insufficient for psychosocial functioning and disability as well as physical functioning. The panel concluded that the evidence was insufficient to recommend for or against vitamin D screening in asymptomatic adults. The panel was not moderately certain that the benefits outweigh the harms or that the harms do not outweigh the benefits.
References
[1] LeFevre ML; U.S. Preventive Services Task Force. Screening for vitamin D deficiency in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;162(2):133-40.
Follow-up Questions and Comments
Padma Maruvada from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, asked whether the USPSTF vitamin D panel had recommendations about fortification practices related to vitamin D. Dr. LeFevre indicated that the USPSTF does not develop such recommendations because fortification is a community preventive service, not a clinical preventive service.
Taylor Wallace from the National Osteoporosis Foundation indicated a concern that the studies used as the basis for recommendations might not take into account baseline status for the nutrient. Clinical services might need to be personalized rather than be based on evidence-based medicine approaches. Dr. LeFevre responded that the commenter's concern relates to the literature, not the USPSTF process for recommendations. Baseline status can be taken into account if the studies available carry out and conduct the assessment; such studies are needed. The questioner commented that metaanalyses are carried out often without regard to subgroups, and that a conclusion of "insufficient" means to most that they should not use the intervention. Dr. LeFevre responded that meta-analyses can and do examine data on subgroups, but studies often lack sufficient statistical power to allow analysis of subgroups. He added that an "I" rating means that the USPSTF cannot formulate a recommendation for clinical practice on the basis of the evidence. Clinicians still must make a decision about what to do, but the USPSTF cannot tell them what to do based on evidence. He suggested that it would be best to hope that the absence of, or at least the relative inadequacy of, the science is incorporated into any discussion with patients that may take place. The "I" statement does not mean "don't do it," it means instead "we don't know."
PANEL DISCUSSION: PERSPECTIVES ON EVALUATING EVIDENCE IN THE PRIMARY CARE CONTEXT
Following the Session 1 presentations, a panel provided additional comments on evaluating evidence. A discussion with the audience followed. Paul Coates, Ph.D., of the Office of Dietary Supplements at the National Institutes of Health, served as moderator. He introduced the four panelists and invited them to provide opening remarks.
Panelist: Robert P. Heaney, M.D.
Creighton University
Two frameworks can be used to determine vitamin D requirements: the risk-avoidance (or risk- assessment) approach, which focuses on the prevention of a disease outcome, and the physiology approach. Physiology here means a determining endpoint, not an intermediate endpoint, and is related to the support of cell function. In the risk-avoidance approach, the focus could be on statistical power and the asymptotic approach to a chosen endpoint. Although these are important, this presentation focuses on adherence to the rules for nutrient studies.
The components of an informative nutrient study are:
Basal status determined and used as an inclusion criterion
Treatment (change in intake) sufficient to alter nutrient status meaningfully
Change in nutrient status confirmed and used as the independent variable in the hypothesis
Known dose-response curve
Optimized co-nutrient status
These components have been used regularly in animal studies, but are novel to clinical nutrition.
Let us first consider the dose-response that is of interest. A pharmacologic dose-response curve for the average drug response has a sigmoidal shape and typically extends over three orders of magnitude, as shown in Figure 1-11.
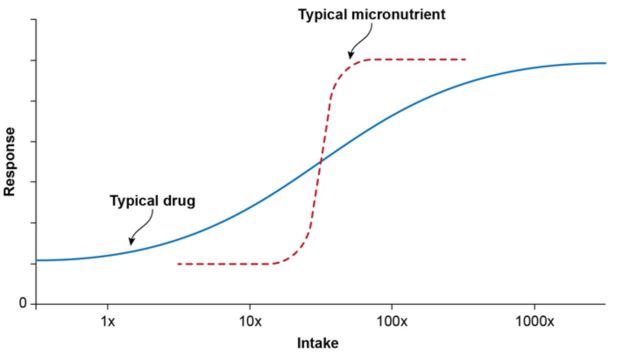
FIGURE 1-11. Dose-Response Curves: Drug versus Micronutrient.
Increasing the dose for a drug anywhere across this relatively large range—which appears to be linear in its central third—results in a measurable effect. Often, linearity is assumed for nutrient effects, but this is not consistent with how nutrients function. Rather, micronutrients tend to have a dose- response relationship in the middle of the 10x and 100x orders of effect observed for drugs. Furthermore, for nutrients, the curve is steep and there are null-response regions at the low or high ends of the range (i.e., flattened ends of dashed curve in Figure 1-11). The existence of null response regions underscores the importance of baseline status. In short, if a patient already has enough of the nutrient, administering more will not produce a benefit.
For vitamin D, the low end of this prevailing range of serum 25(OH)D concentrations is at 10 ng/mL, and the high end is at approximately 100 ng/mL. This range is typical in free-living people with varying sun-exposure levels and diets who do not take supplements. The shape of the curve shows that the response range encompasses less than one-third of the full range, with two null-response regions.
To mix individuals in a single study with baseline status across these three regions will almost guarantee a null outcome. Similarly, to include studies with individuals in all three regions in a meta-analysis or systematic review is inappropriate. Moreover, if the range of intake to maintain 10 ng/mL of serum 25(OH)D is 1,000 IU vitamin D per day and 10,000 IU/day is needed to maintain 100 ng/mL, then studies that typically administer 200, 400, and 600 IU/day span only a tiny fraction of the total available dosing range.
These quantitative issues need to be taken into account in the design of original studies and also of meta-analyses and systematic reviews. Systematic reviews typically have explicit methodology- inclusion criteria, but their authors often overlook the biological criteria mentioned above. This is the case for the principal reviews on which the Institute of Medicine (IOM) and the U.S. Preventive Services Task Force based their recommendations.
The physiology approach relies on readily measureable endpoints. In contrast to measuring, for example, risk of cardiovascular disease, a physiology approach would measure a critical physiologic function, such as the support of lactation. Thus, if the goal is ensuring that breast milk is capable of providing all of the cholecalciferol (vitamin D3) that the infant needs, serum 25(OH)D concentration must be high enough to allow transfer of cholecalciferol into milk. Although serum cholecalciferol is a research measure, not a clinical measure, it is nevertheless quite suitable for the needed physiologic studies.
The physiology approach inevitably produces a higher estimate of requirement than the risk- avoidance approach. Most of the available trials and reviews are flawed because of their failure to use relevant biological criteria associated with an informative nutrition study and are therefore biased toward a null effect. The field of clinical nutrition needs to choose between the risk-avoidance approach and the support-of-physiology approach. Although the risk-avoidance approach might be easier to use, its use might not be compatible with the realities of nutrients.
Panelist: Gordon Guyatt, M.D., M.Sc. McMaster University
My remarks will focus first on the objectives of this conference and then specifically highlight the important role of values and preferences in clinical decision-making. I would like to clarify that value and preference decision-making can be done efficiently in clinical practice.
This conference was organized to be relevant to the developers of clinical guidelines who provide unambiguous recommendations for clinicians. It was not designed to produce an outcome that is directly useable by practicing clinicians. Clinicians cannot be expected to process sophisticated evidence summaries, which was the focus of this first session. Clinicians need unambiguous recommendations.
Unambiguous recommendations can take the form of strong recommendations, along the lines of a directive to "just do this." However, guidelines developers can also make weak recommendations that are value and preference sensitive. Weak recommendations are implemented through shared decision-making, which requires simple, digestible evidence summaries that clinicians and patients can understand. Dr. Heaney asked whether these summaries are to be based on courses of action for patient-important outcomes with estimates of certainty (for example, derived from the GRADE [Grades of Recommendation, Assessment, Development, and Evaluation] system), or whether they are to be based on physiological reasoning. A choice must be made, and my choice is different from that of Dr. Heaney.
Given this meeting's focus on clinical-guidance developers, the emphasis must be on the need to specify values and preferences—that is, judgments that justify various courses of action. Although guidelines are improving, a major deficiency is their failure to articulate the relevant values and preferences. The presentation by Dr. Montori described guidelines that place high value on preventing falls and low value on costs, and which clearly indicated the values and preferences associated with the recommendations. Patients who place low value on a small and uncertain reduction in falls and a high value on avoiding daily medications and on the uncertain risk of excess intake are unlikely to choose to take vitamin D supplements to prevent falls. If vitamin D deficiency is specific to older age and low sunlight exposure, older persons with low sun exposure may choose to take vitamin D supplements more often than younger individuals with greater sun exposure. From a public-health perspective, guidelines producers who place a low value on very uncertain benefits of vitamin D supplements and a high value on the need to conserve scarce health resources for interventions are likely to recommend against the use of vitamin D supplements. In other words, when the situation is uncertain, a person who places a high value on using resources for what is known to work is very unlikely to recommend the uncertain intervention.
It would be useful if this conference could underscore the need for guidelines developers to specify the values and preferences that underlie their recommendations. Once values and preferences are stated in guidelines, the question becomes how such information is used for shared decisionmaking. Dr. Montori gave us an example of decision aids used for this purpose—cards given to patients to help them make decisions about anti-diabetic medications. Clear evidence summaries of key information can be shared with patients through electronic devices. Researchers are studying ways to present these summaries so that patients and clinicians can understand outcomes and risks of undergoing or not undergoing a given intervention. These kinds of aids and electronic databases could be developed for vitamin D supplements.
In summary, clinicians need well-structured guidelines with graded evidence that indicate the guidelines developers' confidence or lack of confidence in the outcomes of implementing the guidelines. The outcomes should be informed by physiology, but patient-important outcomes should be the focus.
It is important to specify the constellation of values and preferences that could lead to different decisions or courses of action relative to the outcomes. If shared decision-making is to occur, clinicians will need simple, understandable evidence summaries. Overall, the importance of values and preferences must be highlighted in the face of uncertainty, and, as this session's presentations revealed, vitamin D is associated with uncertainties.
Panelist: Edward L. Giovannucci, M.D., Sc.D. Harvard University
My comments address the impediments to the ability of randomized controlled trials (RCTs) to demonstrate a true association between an intervention and a health outcome. The question of whether RCTs are really the gold standard is not unique to vitamin D, but it is germane to the evaluation of evidence, as discussed in this session. Six factors that influence evidence quality are:
Dose that is too low or too high
Wrong part of dose-response curve
Low compliance rate
Contamination (placebo group)
Wrong part of natural history
Insufficient duration
It is important to keep in mind the natural history of diseases and its influence on the appropriate duration for RCTs to demonstrate an effect. If the exposure to the intervention occurs at a later stage in the development of the condition of interest, an RCT is likely appropriate and relevant. The trial of such an intervention that is conducted, for example, over 3-5 years late in the disease's natural history can, in theory, produce the "correct" answer. However, if the relevant exposure occurs over the long term, perhaps even a lifetime, a trial can focus only on a fraction of the exposure period. It is still possible to obtain the "correct" answer, but the association is greatly attenuated. If the exposure occurs prior to the trial, it is not possible to obtain the "correct" answer. For trials using vitamin D and many other substances, investigators might not consider sufficiently the timing of the exposure and the trial.
For example, evidence suggests that hormones exert their actions late in the development of breast cancer. Obesity probably also has an effect on breast-cancer development at a late stage.
Tobacco can have effects early in cancer development, possibly because patients have direct exposure to it. Overall, most risk factors for cancer have a long time lag. Very few RCTs on cancer endpoints have lasted long enough, such as 15-20 years, to establish "correct" answers. One exception is aspirin for colorectal-cancer prevention. Most of the existing trials lasted 5 years, but several included a follow-up period. These studies initially found no effect of aspirin on colorectal-cancer development. However, by 10-19 years after aspirin administration, the intervention had a beneficial effect. A person whose understanding of aspirin and cancer was based on trials of less than 10 years would have come to the wrong conclusion about the benefits of aspirin use for colorectal-cancer prevention.
Almost all RCTs have examined late effects only. The number of associations missed in trials due to mis-specified latency periods or insufficient duration is unknown. These mitigating factors should be an important aspect of interpreting and using results from trials.
Panelist: Roger Bouillon, M.D., Ph.D. Katholieke Universiteit, Leuven, Belgium
My focus pertains to vitamin D considerations in countries other than the United States and Canada. All of the European guidelines related to vitamin D specify daily intakes of vitamin D, and most are country specific. However, the Standing Committee of European Doctors, an umbrella organization of the national medical associations of 27 countries, also published a recommendation on vitamin D intakes. Several of the European recommendations are summarized in Table 1-6.
Table 1-6. European Recommended Vitamin D Intakes
Nutritional Society of Germany, Austria, and Switzerland; 2Health Council of the Netherlands; 3Health Council of Belgium; 4Nordic Council of Ministers; department of Health; 6Committee on Nutrition, French Society of Pediatrics; National Medical Association.
aRecommended if sun exposure is limited; bRecommended if >75y; cBreastfed infants; dChildren <18 months receiving fortified milk; ePlus calcium if >75 y.
Despite recommended intakes for vitamin D in the amounts shown in Table 1-6, Europeans typically have a median reported vitamin D intake below 200 IU/day. The exception tends to be the Nordic countries, especially Norway, where the routine consumption of cod liver oil is common. Infants appear to have an approximately 80% compliance rate with the intake recommendations, whereas the elderly frequently fail to meet the recommendations.
Recommended vitamin D intakes from Japan are lower than those in Europe. In 2005, an adequate intake in Japan was <200 IU/day. The exception was pregnant women, who needed an extra 100 IU/day. The average intake for the Japanese population, 200-400 IU/day, is higher than in Europe, likely due to the high intake of fish in Japan.
The European Food Safety Authority defines the amount of a nutrient that may be present or added to a food for it to be labeled as having health effects in European Union countries. The authority requires that the food provide 15% of a standard reference value (400 IU/day for vitamin D) for this purpose. The authority has also set an upper safe limit of intake, which is similar for vitamin D to that recommended by the IOM.
Many European recommendations have not been reviewed or updated for several years, and some countries are revising their recommendations. The extent to which these recommendations will change is uncertain.
Panel and Audience Discussion
Dr. Coates opened the discussion by noting that Dr. Kramer had joined the panel and invited him to offer a remark. Dr. Kramer acknowledged the tension between observational data and data from RCTs. He pointed out that observational data often have the same biases as RCTs, only more so, and thereby introduce more "noise" into the determination of relevant relationships.
Dr. Kramer further commented that issues related to duration and timing of exposure are well known to trial designers, which is why they prospectively design and adequately power their studies. He added that the National Cancer Institute understands the issues surrounding study duration and often considers funding studies for 10 years and beyond. Investigators should design observational studies that are good enough to derive the same answer as an RCT.
Dr. Giovannucci agreed with Dr. Kramer's comments and expressed concern that the outcomes of inappropriately short clinical trials sometimes lead researchers to conclude that the observational data are inaccurate, which may not be the case. Observational data can provide an integrated picture and may have a high probability of producing false-positive results, but RCTs have a high probability of producing false-negative results. Dr. Heaney noted that the discussion between Dr. Kramer and Dr. Giovannucci related to the avoid-disease mode of data evaluation, not to the physiology mode, which has different issues.
Dr. Mayne noted that the possibility of false-negative outcomes is important when adverse effects occur. She asked the panel to comment on the need to start trials earlier in the life course in light of the points that Dr. Giovannucci had made. She also asked whether to discount the statistically significant increase in breast-cancer risk seen in the largest trial conducted to date, the Women's Health Initiative, based on subgroup analyses of participants taking vitamin D supplements.
Dr. Giovannucci responded by describing a recent Mendelian randomization study on vitamin D that focused only on single nucleotide polymorphisms that were "upstream" of 25(OH)D production.
The authors concluded that vitamin D concentration has a strong inverse association with cancer mortality. Dr. Giovannucci said he did not consider the outcomes conclusive or airtight in large, well- conducted studies, and believes that the evidence tends to be more positive for vitamin D supplementation's ability to reduce cancer risk.
Dr. Bouillon noted that international trials or observational studies have the advantage of elucidating how different backgrounds and environments might be relevant to the benefits or adverse effects of vitamin D supplements. Dr. Kramer pointed out that larger samples provide more precision, but not necessarily the correct result. A hallmark of evaluating the literature is noting the level of consistency in the findings of studies with different designs and in different populations.
Dr. Young asked whether data on the benefits and risks of vitamin D supplements could be presented in the same way as for statins and whether presentations of such information to patients could be standardized. Dr. Guyatt responded that presentations on risks and benefits of interventions to patients must be standardized and messages must be clearly stated. Approaches to delivering information on the risks of taking or not taking an action are being studied. These decision aids help both patients and clinicians. Dr. Heaney remarked that statins are expensive and have side effects, whereas vitamin D is less expensive and its side effects are speculative. Dr. Kramer noted the appeal of shared decision-making between clinicians and patients, but this approach has downsides and gaps. For example, educating different subpopulations might require different approaches to framing the literature. Furthermore, many clinical issues that clinicians are supposed to discuss with patients have insufficient information. Discussing every such area of uncertainty in the doctor-patient encounter is not feasible and might crowd out other issues of more importance to the patient. Clinicians and patients run out of time very quickly, and eliminating some discussions on interventions that lack sufficient evidence to yield informed decisions might be valuable.
Dr. Dawson-Hughes from Tufts University commented on the timeline issues for identifying adverse effects in studies. In the Women's Health Initiative, for example, women developed kidney stones after 5 to 7 years of intervention. Dr. Giovannucci noted the many examples of adverse effects that "show up later." Dr. Kramer said that this issue is critical for clinical trial design, and investigators often underestimate the amount of time needed to reveal the outcome of interest. The possibility of unexpected outcomes underscores the value of data safety and monitoring committees.
Dr. Victor Montori commented that the decision aid he had described earlier has been independently studied in multicenter settings, and it appears to add about 3 minutes to the patient visit. Shared decision-making therefore has an "opportunity cost," in that discussing one topic means not addressing other topics, which could have a downside. Dr. Montori also underscored his concern that clinicians not revert to selective citation (sharing details only on studies that show benefits) during shared decision-making about vitamin D supplements. Selective citation is misleading and reduces trust in the medical profession. The resulting question for the panel is how clinicians should have conversations with patients that do not reduce their trust in clinicians further. Dr. Coates said that this question is a theme of this conference.!!!Session 2: What Is the View from the Front Lines of
Clinical Practice?
This session introduced practical challenges faced by clinical practitioners and those who communicate health information to the public. The session began with an overview of the vitamin D "information landscape" that confronts caregivers and patients. A panel discussion followed.
THE VITAMIN D LANDSCAPE
Presenter: Clifford J. Rosen, M.D. Conference Chairperson, Maine Medical Center Research Institute
Session 1 focused on the use of evidence to develop recommendations and guidelines in the face of uncertainty and, particularly, on the use of data to inform expert opinion and clinical judgment. The remaining sessions will consider several key uncertainties that surround vitamin D:
How should nutrition scientists approach the concept of nutritional risk?
What is the context for the use of dietary supplements and food sources of vitamin D?
What are the challenges surrounding laboratory measures of serum 25(OH)D concentrations?
The conference goal is not to delve into the controversies regarding the relationship between vitamin D supplements and health outcomes. There seems to be wide agreement that vitamin D supplements play a role in skeletal health, some agreement that they might help prevent falls in older persons, and considerable—but not total-agreement that other relationships between vitamin D supplements and health outcomes lack conclusive evidence. Of course, the benefits of vitamin D supplements reflect an uncertainty of a type important to guidelines developers. However, the focus of this session is the process for distilling available data and dealing with uncertainties, including those surrounding the benefits of vitamin D supplementation.
A number of factors present challenges to practicing clinicians. First, guidance and recommendations on vitamin D supplements vary (Table 2-1). Guidelines developers agree on the benefits of vitamin D supplements for skeletal health and that routine screening for vitamin D status is not necessary. But other conclusions of guideline panels are less harmonious. For example, panels have different recommendations on dietary vitamin D intake as well as optimal concentrations of serum 25(OH)D.
Table 2-1. Selected Vitamin D Recommendations and Conclusions
Moreover, as Table 2-2 shows, suggested intakes of vitamin D range by twofold or more.
Table 2-2. Recommended Vitamin D Intakes from Different Guidelines
Second, there are notable differences between what intake measures of status tell us compared to serum measures of status. Measures of vitamin D intake cannot take into account contributions from sun exposure and therefore typically underestimate status. In addition, given the changes in the food supply in recent decades, available food composition tables are probably out of date and might not capture important current sources of vitamin D. Therefore, when compared to the more commonly used status measure, i.e., serum 25(OH)D concentrations, it is not surprising that vitamin D intakes predict a higher prevalence of deficiency than do serum measures. Figure 2-1 uses a reference value from the Institute of Medicine to assess vitamin D status. The results show considerable discrepancies between status based on intake versus serum concentrations of 25(OH)D for each age/gender group.
Figure 2-1. Serum 25(OH)D concentrations versus intake as measures of vitamin D status. Red line reflects reference value for use with population groups. Figure is for illustration purposes only; accurate estimates of prevalence of inadequacy require use of probability calculations. Source: [3].
Third, terminology and definitions can cause confusion. Some guidelines developers use "deficient" or "insufficient" either synonymously or without defining these terms based on an established clinical outcome. Guidelines developers have also suggested different serum 25(OH)D concentrations as reflective of the same status condition, for example "deficient."
Busy clinicians do not have time to sort through and evaluate the available information, so they often turn to readily accessible and succinct online resources. This makes it even more important that the uncertainty associated with guidelines be communicated. The process of formulating recommendations for vitamin D must involve various types of data that have many uncertainties. Some scientific judgement is usually involved in developing these guidelines. Questions to answer when developing guidelines include: How have the inevitable uncertainties been factored into the guidelines? Is the process for factoring these uncertainties into the guidelines transparent? Are users made aware of the limitations of these guidelines?
The morning's discussions generically addressed evaluation of data in the face of uncertainty. The remainder of this conference will focus on vitamin D relative to several key uncertainties. First, the limited accuracy of analytical methods for measuring serum 25(OH)D concentration might affect a clinician's conclusions about recommendations for patients in daily practice. But it also can affect the foundations for making conclusions about the dose-response relationship between vitamin D supplements and health outcomes that are built on old measures of serum 25(OH)D concentration. Moreover, laboratory 25(OH)D-concentration test reports include a reference range. No government regulations or central body is responsible for establishing these ranges, which can vary by laboratory. At times, the reference ranges change for reasons that are not entirely clear. Furthermore, the cut-point for determining adequacy or inadequacy affects the percentage of the population deemed to be at risk of deficiency and which patients need interventions. These are topics for Session 5 of this conference.
In response to laboratory reports of serum 25(OH)D concentrations, many clinicians prescribe a dietary supplement, but the dosages they recommend vary widely. As will be discussed in Session 4 of this conference, some clinicians wonder whether supplements are overprescribed, what the correct dosages are, and what each patient's background exposure is given the newest food sources containing vitamin D that food manufacturers are introducing. Furthermore, many clinicians believe that high doses of vitamin D supplements are benign and, under certain circumstances, might serve as a legitimate placebo for anxious patients. Certainly, extreme intakes are required to reach serum levels that cause classic vitamin D toxicity. However, some nutrition scientists suggest that serum 25(OH)D concentrations lower than those associated with classic toxicity have adverse consequences, although other experts dispute this claim.
Session 3 will focus on the uncertainties about which groups are most likely to be at risk of lower vitamin D status. Topics to be addressed include differences in the relationships between serum values and functional outcomes for different subgroups and the role of genetic variants in these relationships. Dr. Carriquiry from Iowa State University will begin Session 3 with an overview of thoughts on how to reconcile the reliance in clinical practice on cut-points, given that measures such as nutrient effects and desirable serum values reflect distributions of points around a mean for the population. A distribution of such points does not identify a dividing line above which is one effect and below which is another effect. In reality, many people might have adequate status even though their 25(OH)D concentrations are below a specified cut-point. For instance, many researchers establish a cut-point for adequacy that is akin to the highest requirement for the entire population. When this occurs, as shown in Figure 2-2, many people below that cut-point are declared inadequate but, when illustrated as a distribution, it is clear that at least some of those people are not in fact experiencing inadequacy.
Figure 2-2. Distribution of nutrient requirement illustrating that many persons with intakes below the 2 standard deviation mark (also referred to as the Recommended Dietary Allowance which is often used as a cut-point for adequacy) are not experiencing inadequacy.
These considerations are important food for thought in the arena of vitamin D status, intake, supplement use, and risk from excess. Before Sessions 3, 4 and 5 begin, a panel of conference participants will reflect on both the nature of the front lines of patient care in primary care practice and communicating information about vitamin D to the general public.
References
American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons and recommendations. J Am Geriatr Soc. 2011;59(1):148-57.
Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30.
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Moyer VA; U.S. Preventive Services Task Force. Prevention of falls in communitydwelling older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(3):197-204.
LeFevre ML; U.S. Preventive Services Task Force. Screening for vitamin D deficiency in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;162(2):133-40.
Nowson CA, McGrath JJ, Ebeling PR, et al; Working Group of Australian and New Zealand Bone and Mineral Society, Endocrine Society of Australia and Osteoporosis Australia. Vitamin D and health
in adults in Australia and New Zealand: a position statement. Med J Aust. 2012;196(11):686-7.
German Nutrition Society. New reference values for vitamin D. Ann Nutr Metab. 2012;60(4):241-6.
Health Council of the Netherlands. Evaluation of dietary reference values for vitamin D. 2012. The Hague: Health Council of the Netherlands, 2012; publication no.2012/15E.
http://www.gezondheidsraad.nl/sites/default/files/201215EEvaluationDietaryReferenceVitaminD.pdf.
Francis RM, Aspray TJ, Bowring CE, et al. National Osteoporosis Society practical clinical guideline on vitamin D and bone health. Maturitas. 2015;80(2):119-21.
Standing Committee of European Doctors. Vitamin D nutritional policy in Europe. Brussels: CPME 2009/179 Final EN. http://doc.cpme.eu:591/adopted/2009/CPME AD Brd 241009 179 final EN.pdf.
PANEL DISCUSSION: WHAT DO CLINICIANS EXPERIENCE?
As a prelude to turning to vitamin D specifically, Dr. Rosen introduced a panel intended to highlight what clinicians and the public experience in dealing with vitamin D. Dr. Rosen moderated the panel discussion. He invited each panelist to provide their perspectives and then opened the discussion to the audience.
Panelist: Ravi I. Thadhani, M.D., M.P.H. Harvard Medical School and Massachusetts General Hospital
My remarks highlight a few of my experiences with vitamin D based on my nephrology practice. Nephrologists are primary care physicians for many patients with kidney disease, especially as their disease progresses and they need dialysis. Patients with kidney disease often develop extreme vitamin D deficiency, and studies of the consequences of this deficiency and the potential benefits and/or toxicities of vitamin D replacement in this population are appropriate and informative. In short, administering activated forms of vitamin D in patients with kidney disease has a strong and long history of significant benefit.
However, young nephrologists sometimes wonder why they should prescribe vitamin D supplements. They are familiar with controversies about vitamin D supplementation outside of
nephrology, and they know that clinical trials have not produced the expected positive results. They therefore ask for data to support the use of vitamin D in their practices. They do not remember a time when fractures, significant bone disease, and brown tumors were common. These alterations and abnormalities due to vitamin D deficiency have been largely relegated to textbooks.
As kidney function declines, patients' concentrations of 25(OH)D and 1,25(OH)2D drop and their parathyroid hormone (PTH) levels rise concomitantly, resulting in nutritional abnormalities. Studies published years ago suggested that, in dialysis, skin alterations are profound and the conversion of precursors of vitamin D by ultraviolet light is challenged. Other reasons for the lower levels of vitamin D metabolites in patients with kidney disease are vitamin D catabolism and reduced vitamin D synthesis. Several studies link kidney dysfunction with heart disease (such as left ventricular hypertrophy), partly due to lower levels of activated forms of vitamin D. One dialysis company has reported that 10,00015,000 tests of vitamin D levels are conducted every month in dialysis patients. Almost every patient on dialysis has vitamin D deficiency, raising the question of why clinicians measure it. Nephrologists treat elevated levels of PTH very effectively with calcitriol (1,25(OH)2D) and related analogs. Vitamin D treatment has good effects on bone, but identifying other benefits has been a challenge even though supplement use is common in patients with kidney disease. Almost every nephrology meeting has debates about whether patients on dialysis or with chronic kidney disease need nutritional vitamin D supplementation, active vitamin D administration, or both.
Panelist: Peter S. Millard, M.D., Ph.D. Seaport Community Health Center
Family doctors like myself live with uncertainty and are comfortable with it. However, I experienced a new uncertainty when I returned to my community after working in Africa for 5 years. A colleague told me that he was taking vitamin D supplements for depression. In fact, many people seemed to be undergoing vitamin D testing and were being told that their 25(OH)D levels were low.
When I checked UpToDate®, an online resource for primary care doctors, I learned that measuring 25(OH)D concentrations was appropriate in people taking medications that accelerate vitamin D metabolism (such as phenytoin); hospitalized patients; and those with obesity, limited sun exposure due to wearing protective clothing, osteoporosis, malnutrition, and dark skin. I had not been ordering vitamin D tests for my patients, many of whom as resident of Maine wear protective clothing, and I considered that I was probably outside the mainstream and should begin doing so.
Given my new interest in vitamin D, I and colleagues examined national data on vitamin D testing using electronic medical records from Athena Health, Inc., for the approximately 750,000 patients seen monthly by 8,000 primary care providers. From January 2013 through September 2014, approximately 4-5% of all patient encounters included vitamin D testing. The sunbelt states of Arizona and Nevada had higher rates of vitamin D testing (8-10%) than others states. Although these differences could be due to the high concentration of retirees in these states, Florida had a lower rate of vitamin D testing even though it probably has a similar population. Moreover, Illinois, Maryland, Delaware, and Rhode Island had high testing rates (approximately 10%). The largest age group tested, as expected, was those over age 65 years, which accounted for 39% of all tests. About 70% of the tests were done in females, and this rate was fairly constant among age groups. Based on International Classification of Diseases, 9th revision (ICD-9) diagnoses, fewer than 0.1% of the vitamin D test orders were for an osteoporosis diagnosis and monitoring. The primary diagnoses associated with a vitamin D test were falls in the elderly (12.3% in those aged 65 years or older) and depression in younger groups (5.7% in those aged 18-29 years, 7.0% in those aged 30-49 years, and 7.2% in those aged 50-64 years).
I suggest that these data do not answer many questions, but testing vitamin D status clearly has opportunity costs. The cost of the test itself is significant. The amount of time my colleagues spend doing the tests, interpreting the results, and deciding what to do based on the results is considerable. Clinicians need some clarity on when to order vitamin D tests. In the long run, the research to resolve issues surrounding vitamin D testing might not be nearly as expensive as continuing to do what clinicians are doing now.
Panelist: Sylvia B. Rowe, M.A. SR Strategy, LLC
Vitamin D is an incredibly hot issue in the media. An examination of media reports over 2 weeks in November 2014 indicated that the mainstream ("prestige") media reported that people should take vitamin D supplements to prevent neuromuscular disease, pre-hypertension, cardiovascular and respiratory disease, type 2 diabetes, and cancer and to maintain brain function. Even the New York Times reported that low vitamin D status is tied to high death risk. Popular physician websites state that vitamin D supplements can combat asthma, dementia, pain, inflammatory bowel disease, arterial calcification, nitric oxide reduction, flu, antibiotic resistance, and melanoma. Not only is this information distributed to the public, but it also has an impact on the wide range of health professionals who must answer patients' questions and provide a grounding in what is and is not fact in this arena.
What makes coverage of vitamin D so sexy compared to other issues? First, it is important to understand that a communication chain exists that starts with emerging research, scientists, and expert reports. Press offices amplify this information. The chain also includes journals and professional societies, which further amplify the message. At the same time, health advocacy groups and the food and dietary-supplement industries address the issue from a marketing perspective. At the far end of the chain are journalists. So, when there is genuine disagreement about vitamin D supplementation among well-respected scientists, it is quickly recognized and relayed. Although there may be some consensus on general recommended intakes among most experts, many are calling for far higher intake levels. The media love these types of conflict, especially when they stem from bona-fide experts. Although experts probably agree more than they disagree, the disagreement is what receives the coverage. It is challenging for members of the public to decide what to do under these circumstances.
Second, advocacy groups are calling for significantly higher recommended vitamin D intakes than those discussed at this meeting at a time when the media are paying no attention to the potential harms of high vitamin D intakes. Some experts might suggest that the risks of high vitamin D intakes are minimal. However, recommended intakes must be considered in the context of the population's characteristics, how often they take vitamin D supplements, their background diets, their food sources, the extent of vitamin D fortification in their food sources, their sun exposure, their adiposity, and similar factors.
Today's media reports give the sense that vitamin D supplements on their own are major contributors to health in the absence of this context. However, higher levels in certain populations might have downsides. Vitamin D supplements could divert behavior. For example, people might pay more attention to vitamin D supplementation than adopting other health behaviors that may be more important. How does the clinician discuss with patients how to prioritize health behaviors, especially given the short duration of office visits? Moreover, the cost of vitamin D supplementation to the consumer and to public-health programs in general must be considered.
By far, however, the major concern is the potential harm of the media approach to consumers' trust. When something is labeled as the "magic bullet" and these claims are followed by evidence to the contrary and questions from medical groups about the value of interventions, consumers lose trust in the entire scientific and medical establishment. How to communicate such downsides to consumers must be understood. Furthermore, advice is muddled on the amounts and serum concentrations of
vitamin D that can be considered deficient or optimal for health. Questions arise about whether there is a difference among these recommendations and how to describe the difference.
When I was covering news stories, I heard the following: "Extraordinary claims require extraordinary proof." If the promise of vitamin D supplementation stays front and center in communications, those responsible for these messages must understand the science and the unanswered questions. They must also place the information into the appropriate context for consumers so that consumers can make truly informed decisions about vitamin D supplements.
Panel and Audience Discussion
Dr. Rosen opened the discussion by describing a study that reviewed recent publications on vitamin D by 10 journalists and rated the journalists' views on vitamin D as either favorable or unfavorable. The researchers then examined each journalist's entire publication history on vitamin D. The results showed that journalists' publication histories aligned perfectly with their current views; those who had had negative attitudes toward vitamin D supplements earlier in their careers had the same attitudes later on. Dr. Rosen did not know whether the study had been published. He asked Ms. Rowe whether journalists are as polarized as physicians. Ms. Rowe responded that, like everyone else, journalists may have biases and some are better informed than others. Journalists' own perspectives often influence the stories they write. Journalists depend heavily on their sources, and the champions of vitamin D supplements have been vocal and perhaps more successful at reaching out to members of the media.
Dr. Rosen asked Dr. Millard to comment further on his impressions when he returned from Africa about whether patients were asking about vitamin D, how vitamin D was perceived in his rural community, and how it was brought up in office conversations. Dr. Millard responded that many of the patients he saw early on already had vitamin D on their radar screens and some were interested in being tested. However, he believed his patients request vitamin D testing less often now than in the past, and the enthusiasm now comes from professionals instead. Dr. Millard wondered about attitudes toward testing in urban communities. In his rural community, new patients often do not have their vitamin D levels measured and do not seem to view their concentrations as a concern.
Dr. Montori suggested that vitamin D supplements "went viral" before evidence was available to support their value. Most notably, the focus on vitamin D supplements resulted from the belief that it is an effective intervention for psychosocial complaints, fatigue, discomfort, aches, depression, and other conditions that everyone experiences in some way. This treatment has seemed innocuous, almost like a placebo. Dr. Montori contended that there is an apparent disconnect that this conference should address between what is occurring on the front lines with respect to the use of vitamin D for depression and general malaise versus the research focus on vitamin D relative to reduced risk of diseases such as cardiovascular disease, cancer, diabetes, and organ dysfunction. He invited comment from the panelists.
Dr. Millard agreed with Dr. Montori, commenting that clinicians are struggling to find a way to help patients who report a myriad of psychosocial or pain conditions. Vitamin D supplements seem to offer a way to address these conditions, and clinicians have embraced it widely as a result. Dr. Montori added that physicians may not be sure of the cause of their patient's symptoms. Therefore, when patients have low vitamin D concentrations, many clinicians recommend a supplement. These physicians might admit that they do not know whether the treatment will correct the condition, but patients feel better because they are doing something about their symptoms. Dr. Rosen added that patients report feeling better after taking supplements and clinicians feel better because their patients experience measurable benefits. In effect, the surrogates (increased serum levels) become the outcomes.
Ms. Rowe queried whether this approach amounted to using a placebo. Dr. Rosen did not think that clinicians would take this position. He often asks groups of physicians whether they take vitamin D supplements, pointing out that there is not much evidence for its benefits beyond bone health. Physicians often respond that evidence will ultimately become available, and there is no harm in starting supplementation now if future evidence will show that it is beneficial.
Dr. Young recalled attending a conference 15 years ago in which virtually all physicians in attendance were taking antioxidant supplements. The antioxidant interest at the time was similar to that of vitamin D now: large bodies of evidence, plausible mechanisms, widespread reports of deficiency, and availability of antioxidant supplements coupled with a sense that a supplement could not be harmful. However, the completion of clinical trials disproved these views. Dr. Young asked whether panelists agreed that the earlier antioxidants-supplement situation is analogous to that of vitamin D today. Dr. Millard responded that the situation of homocysteine is also similar to that of antioxidants and vitamin D.
Neil Binkley from University of Wisconsin, Madison strongly supported Ms. Rowe's perspective on trust, adding that this conference had the potential to restore some trust. No one at this conference could know the right amount of vitamin D supplements to take, the correct way to measure vitamin D concentrations, or even how to measure them. He suggested that the conference organizers develop conclusions to clearly state these uncertainties. Dr. Binkley then referred to the earlier statement made by Dr. Bouillon during the Session 1 panel that a great deal of evidence supports the utility of consuming 800 IU/day vitamin D among older adults. Dr. Binkley suggested that this intake amount is the best that this conference has to offer at the moment, and that it should be communicated with the caveat that the field will continue to evolve.
Dr. Rosen noted that Dr. Binkley had raised important points to consider, but this conference was not designed to develop guidelines or consensus recommendations. Although many nutrition scientists would agree with an 800 IU/day recommendation, tremendous uncertainties surround this level and other aspects of vitamin D benefits. In short, reasonable data indicate varying outcomes surrounding the intake of 800 IU/day vitamin D, and this conference was designed to highlight these uncertainties.
Dr. Rosen then raised the topic of uncertainty about vitamin D supplementation in patients with renal disease. He asked Dr. Thadhani whether any guidelines or standard approaches are available. Dr. Thadhani responded that guidelines and recommendations are available, but the number of clinical trials on this topic is so small that uncertainty remains very high.
Dr. Rosen shared a question from an online attendee, who asked why vitamin D is prescribed so often for depression when so few data support this use. The questioner also asked about the types of information that convinces psychiatrists to prescribe vitamin D supplements for depression. Dr. Rosen noted that psychiatrists probably prescribe vitamin D supplements much less often than primary care physicians. Dr. Millard agreed that primary care physicians treat the vast majority of routine depression cases, so they are the chief prescribers of vitamin D supplements. He noted that everyone wants a magic bullet, including primary care providers. Ms. Rowe added that some patients ask for vitamin D supplements, and that physicians responded given that the fallout from media attention to vitamin D affects professionals as well as patients.
Dr. Montori emphasized that research to answer the questions raised during this discussion may be less costly than the continuation of the current health-care-provider practice of prescribing vitamin D supplements. With the growing availability of electronic medical records and other data-management advances, it might be possible to conduct a meaningful trial in patients who ask for vitamin D supplements for depression to answer some of these questions. He suggested this is a missed opportunity at the moment.
Session 3: The Uncertainties—How Do We Think About Risk of Nutritional Inadequacy?
This session explored the use of cut-points versus other determinations of vitamin D inadequacy and then considered questions about groups at risk of vitamin D deficiency. African American case studies were included in the context of both bone health and genetic variants.
DISTRIBUTION VERSUS CUT-POINTS IN CLINCIAL PRACTICE
Presenter: Alicia Carriquiry, Ph.D., M.Sc. Iowa State University
The goal of this presentation is to discuss serum 25(OH)D concentrations and explore how clinicians can more appropriately characterize patients' vitamin D status. There are limitations to the use of cut-points, whereas there are advantages to approaching vitamin D status from the perspective of likelihood and probability. I will be referring to the Institute of Medicine (IOM) recommendations for vitamin D requirements and desirable concentrations of serum 25(OH)D [1] to illustrate the points made, but other recommended standards could be used to illustrate the same points.
Regardless of the population examined, requirements vary from person to person—even among a homogeneous group with similar ages, genders, and races/ethnicities. There is, in fact, a distribution of requirements. The IOM [1] concluded that the normal, bell-shaped distribution of adequate serum 25(OH)D concentrations for healthy adults has a mean of about 40 nmol/L and a standard deviation (i.e., the "spread" around the mean) of about 5 nmol/L (Figure 3-1).
Figure 3-1. Distribution of "requirements" for serum 25(OH)D assuming requirements are normally distributed. Mean serum 25(OH)D concentration requirement is 40 nmol/L; standard deviation is 5 nmol/L. Adequate concentrations for approximately 70% of the population are between 35 and 45 nmol/L.
Therefore, adequate concentrations for the majority of individuals (about 70%) cluster within one standard deviation on either side of the mean and reflect concentrations between 35 and 45 nmol/L. That is, out of 100 patients a clinician sees in a week, the 25(OH)D needs of 70 will be within one standard deviation of the mean. The lOM's Recommended Dietary Allowance (RDA)-like reference value for serum 25(OH)D is derived by adding two standard deviations to the mean reference value. Based on this calculation, 97.5% of all healthy adults have adequate concentrations when they are below 50 nmol/L 25(OH)D. Virtually no one requires more than 55 nmol/L, an amount that exceeds the needs of 999 of 1,000 people. Based on our understanding of distributions, and unless there are any indications to the contrary, it is most reasonable to assume that a patient 's serum 25(OH)D concentration is adequate when it is about 40 nmol/L or 16 ng/mL.
Of course, these measures of serum 25(OH)D—which are used to determine the vitamin D status of an individual—vary among individuals within a group. The measures could, however, also vary among the repeated measurements for a single individual due to within-person variability. However, there is currently only one sample for most individuals in the National Health and Nutrition Examination Survey, and two samples are needed to calculate within-person variability. The limited data suggest that the within-person variability of serum 25(OH)D concentrations is not very large, perhaps 20% of total variability. Therefore, within-person variability does not distort measurements of serum 25(OH)D concentrations to a major extent.
The question for a clinician who wants to determine a patient's vitamin D status is whether the patient's serum 25(OH)D concentration is adequate or inadequate. A key point is that the concentration is adequate if it meets his or her need for 25(OH)D, not if it meets a cut point. A very low serum concentration will be adequate for a person who needs very little 25(OH)D. However, someone with a higher concentration of 25(OH)D may be at risk of inadequacy if his or her need is much higher. Therefore, determining the serum level of 25(OH)D does not provide sufficient information to determine status. The clinician needs to compare this information to that person's true "requirement" for a serum concentration of 25(OH)D. The problem is, of course, that the true need is unobservable.
Because true needs cannot be determined, standard practice is to declare that everyone whose measure is below a given cut-point (such as the RDA or the 97.5th percentile) has inadequate status and everyone else has adequate status. However, this is the wrong way to approach nutrient adequacy because it is based on the assumption that everyone in the population has extraordinarily high requirements. The RDA and biochemical reference values akin to the RDA exceed the needs of the 97.5% of the population and miss only those with the most extreme requirements (2.5% of population). Therefore, use of this type of cut-point greatly overestimates the probability of inadequacy for the vast majority of patients. Moreover, reports on patients' serum 25(OH)D concentrations sent to physicians from different laboratories tend to provide very high ranges for adequacy. For example, some laboratories report that an acceptable range is 75 to 250 nmol/L, and others use 50 to 125 nmol/L.
Based on the lOM's conclusions, 55 nmol/L exceeds the needs of 999 of 1,000 individuals [1]. Even the lower end of these "optimal" ranges of 25(OH)D exceeds the needs of most.
Reliance on a specific concentration would be straightforward and easy if the person's true need for serum 25(OH)D was observable, but this is not the case. An alternative approach that better reflects the biological realities is to calculate the likelihood that a patient's measured 25(OH)D is adequate instead of assuming incorrectly that all individuals have a need for a specific concentration of 25(OH)D. We can develop this approach using two pieces of information. First, we use a measure of the person's serum concentration, which is a stand-in for the true measure of the individual. Second, use an educated guess of the person's need, which is the established mean for the population. But these measures are not perfect and introduce uncertainty which needs to be taken into account as part of our alternative approach.
This alternative "likelihood approach" is based on a measure similar to a z-score, which indicates the probability that a patient has adequate or inadequate 25(OH)D status. The calculations can be used in the clinical setting (see examples in Table 3-1). The first step is to compute the difference between the person's reported 25(OH)D concentration and the established mean need of the overall population. The second step is to compute the standard error of that difference, which takes into account the uncertainties about the accuracy of the person's measurement and the person's true need. In a patient who has a serum 25(OH)D concentration of 17 ng/mL, the difference between the patient's concentration and his or her presumed need is only 1 ng/mL when 16 ng/mL is stipulated as the mean need for adults. Based on information in the IOM report, the standard error is about 3.6 ng/mL. Therefore, for this patient, the approximate z-score is about 0.27.
Table 3-1. Examples of Approximating a Z-score to Assess Adequacy
Patient A
Patient has a measured concentration of 17 ng/mL (42.5 nmol/L).
D is 17-16, or 1ng/mL, where 16 ng/mL is the proposed mean requirement for adults from IOM [1].
Sr is 2 ng/mL (per the IOM).
Sw tentative value is 3 to 4 ng/mL (this example uses 3 ng/mL).
SD is calculated as follows: SD = square root of 3+22 = 3.6 ng/mL.
Approximate z-score for the patient is calculated as follows: z-score = D/SD = 1/3.6 = 0.27.
If the conclusion is that the patient has an adequate 25(OH)D concentration, the chance of being in error is about 39%.
If the conclusion is that the patient has an inadequate 25(OH)D level, the chance of being in error is about 61%.
Patient B
Patient has a measured concentration of 20 ng/mL (50 nmol/L).
D is 20-16, or 4 ng/mL, where 16 ng/mL is the mean requirement for adults from IOM [1].
Sr is 2 ng/mL and Sw is 3 ng/mL.
SD is 3.6 ng/mL.
Approximate z-score for the patient is calculated as follows: z-score = D/SD = 4/3.6 = 1.11.
If the conclusion is that the patient has an adequate 25(OH)D concentration, the chance of being in error is about 13%.
If the conclusion is that the patient has an inadequate 25(OH)D level, the chance of being in error is about 87%.
The calculations needed to carry out this approach are simple. The only information that the clinician requires is the patient's reported serum 25(OH)D concentration. Everything else can be programmed into an app for use on an electronic device. The user enters only the serum concentration, and the app indicates the certainty with which the user can conclude that the patient has adequate or inadequate status.
To summarize, in the real world, serum 25(OH)D concentrations and needs for serum 25(OH)D concentrations vary. Therefore, a low serum level can be perfectly adequate if the patient's need is low. It is not possible to determine an individual's actual need for serum 25(OH)D, but it is possible to make a very good guess using the population's mean need because that is the most common value. A z-score approach takes into account the uncertainties about both the patient's true serum 25(OH)D concentration and his or her true need. The z-score allows the user to compute the chance of making a right or wrong conclusion about the patient's 25(OH)D adequacy based on the data. The user can then tailor treatment decisions based on the z-score and, of course, other clinical considerations.
References
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Follow-up Questions and Comments
Christopher Sempos from the Office of Dietary Supplements commented that within-person variance has two major components: biological variation and laboratory-method variation. One way to increase certainty about the probability of a correct conclusion about a patient's 25(OH)D adequacy is to develop more accurate laboratory procedures. Dr. Carriquiry agreed.
Dr. Heaney concurred that 5 ng/mL is probably an acceptable standard deviation for the distribution of serum 25(OH)D concentrations at the very low requirement concentrations that the IOM stipulated. However, he contended that the coefficient of variation of vitamin D intakes around the mean is 38.4%, regardless of intakes extending from 0 to 20,000 IU per day, as shown in very large datasets. This coefficient of variation would change the calculations presented because the standard deviation is not constant. Dr. Carriquiry responded that her presentation had focused on serum 25(OH)D concentrations, not vitamin D intakes for which the coefficient of variation is typically high. In this case, she assumed that the person-to-person coefficient of variation is about 20% for serum 25(OH)D concentrations.
Dr. Hoofnagle from University of Washington questioned the basis for the IOM's selection of 40 nmol/L as the mean serum 25(OH)D concentration and suggested that different experts might come up with a different number. Dr. Carriquiry responded that whatever the actual mean is, the principles of a distribution are relevant and it would be wrong to use an upper-end RDA-like value as a cut-point. Rather, the clinician must take into account the fact that the requirement is a distribution across the population.
GROUPS AT RISK: IS LOWER SERUM 25(OH)D ALWAYS A CONCERN?
Presenter: Bonny Specker, Ph.D. South Dakota State University
(Delivered by Patsy M. Brannon, Cornell University)
This presentation provides an overview of differences in endogenous synthesis of vitamin D followed by a description of a few populations with low concentrations of circulating 25(OH)D.
Sun exposure is a source of vitamin D for the human body. Based on the in vitro human-skin model, both season and latitude influence the formation of pre-vitamin D. Concentrations of 25(OH)D are typically higher at the end of the summer months and in locations near the equator. Not unexpectedly, longer sun exposure achieves greater 25(OH)D concentrations than shorter exposures. In turn, factors that interfere with or affect the synthesis of 25(OH)D via ultraviolet B (UVB) photoconversion are relevant to vitamin D status. Other relevant factors include skin pigmentation, age, and lifestyle behaviors, including time spent outdoors, clothing, and use of sunscreen.
In vivo UVB radiation studies have examined outcomes for whites versus blacks as well as single exposures versus repeated exposures with additional high doses of UVB radiation [1]. After single UVB radiation exposures, whites achieved higher 25(OH)D concentrations than blacks. However, when blacks were exposed to larger doses of UVB radiation, they demonstrated the same capacity to produce vitamin D as whites. Likewise, related research has shown that repeated exposure to UVB radiation increased serum 25(OH)D at the same rate in whites and blacks [2]. However the magnitude of the increase was lower in black individuals because their initial concentrations were lower. Asians had a similar 25(OH)D trajectory to Caucasians in response to single exposures of UVB radiation, but Asians needed longer dosing periods to achieve the same concentrations as Caucasians [3]. Overall, these findings raise the question of whether race/ethnicity differences in 25(OH)D concentrations following UVB radiation exposure are due to skin pigment or other genetic influences.
Aging affects skin in many ways, including its ability to support vitamin D synthesis. There is evidence that the ability of both the epidermis and the basal stratum to synthesize pre-vitamin D is lower in older individuals [4]. At the same time, research has shown that skinfold thickness declines with age. So a question arises: Is there a role for thin skin in the reduction of serum 25(OH)D concentrations among the elderly?
At the other end of the age spectrum, breastfed infants have large seasonal differences in serum 25(OH)D concentrations, apparently in response to sun exposure [5]. The nadir is in winter for infants born in the summer, whereas the peak for infants born in the winter is in the summer.
Sunscreen use is a lifestyle behavior that could influence endogenous production of 25(OH)D. However, sunscreen might not cover all exposed areas, and it likely becomes less effective during the day if it is not repeatedly reapplied. A randomized controlled trial in Australia found that 25(OH)D concentrations after application of a sunscreen with sun-protection-factor (SPF) 17 were not significantly different between persons younger than 70 and those who were older [6]. Although these findings are interesting, they may be confounded by the fact that an SPF of 17 is low, and higher SPF values are often recommended. Much research is needed to clarify the impact of sunscreen on 25(OH)D levels.
As with lifestyle factors, obesity raises some interesting but unresolved questions about effects on serum 25(OH)D concentrations. Early research showed that obese individuals have lower serum 25(OH)D concentrations than lean individuals when subjected to the same number of hours of sunlight in the same location [7]. In addition, those who are obese show less seasonal variation. Although one might wonder whether spending little time outdoors affects 25(OH)D concentrations in obese individuals, the limited data do not support this possibility [8]. Likewise, research suggests that endogenous synthesis is the same in obese and lean persons. Explanations of these differences have focused on differences in absorption or clearance rates of vitamin D. For example, Wortsman and colleagues revealed that, following both UVB exposure and oral vitamin D supplementation, serum 25(OH)D concentration was lower in obese individuals than lean individuals, leading the authors to conclude that the lower levels may be due to increased clearance or, perhaps, sequestration into fat [9].
Bone mineral density and all-cause mortality, as outcomes, have an interesting relationship to serum 25(OH)D concentrations. Data from the National Health and Nutrition Examination Survey suggest that bone mineral density among whites and Mexican-Americans correlates with concentrations of serum 25(OH)D [10]. However, in African Americans, bone mineral density does not correlate with serum levels and, in fact, is high regardless of serum 25(OH)D concentrations. Data from NHANES also reveal that all-cause mortality rates have a U- or J-shaped risk relationship with serum 25(OH)D concentrations, and higher concentrations are associated with increased mortality rates [11]. Importantly, African Americans have a higher risk of mortality at lower 25(OH)D concentrations than whites, suggesting that African Americans may be more sensitive to some adverse effects of low 25(OH)D concentrations.
Much research remains to be done to clarify the true meaning of serum 25(OH)D concentrations as both an indicator of status and a marker of health outcomes. Despite all of the caveats, the current data suggest rather strongly that serum 25(OH)D concentrations do not mean the same thing in all populations, and this measure needs considerably more sorting out before nutrition scientists can make definitive conclusions.
References
Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesize vitamin D3. Lancet. 1982;1(8263):74-6.
Brazerol WF, McPhee AJ, Mimouni F, et al. Serial ultraviolet B exposure and serum 25 hydroxyvitamin D response in young adult American blacks and whites: no racial differences. J Am Coll Nutr. 1988;7(2):111-8.
Lo CW, Paris PW, Holick MF. Indian and Pakistani immigrants have the same capacity as Caucasians to produce vitamin D in response to ultraviolet irradiation. Am J Clin Nutr. 1986;44(5):683-5.
MacLaughlin J, Holick MF. Aging decreases the capacity of human skin to produce vitamin D3. J Clin Invest. 1985;76(4):1536-8.
Specker BL, Tsang RC. Cyclical serum 25-hydroxyvitamin D concentrations paralleling sunshine exposure in exclusively breast-fed infants. J Pediatr. 1987;110(5):744-7.
Marks R, Foley PA, Jolley D, et al. The effect of regularsunscreenuse on vitamin D levels in an Australian population. Results of a randomized controlled trial. Arch Dermatol. 1995;131(4):415-21.
Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin D. Am J Clin Nutr. 1993;58(6):882-5.
Harris SS, Dawson-Hughes B. Reduced sun exposure does not explain the inverse association of 25- hydroxyvitamin D with percent body fat in older adults. J Clin Endocrinol Metab. 2007;92(8):3155-7.
Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690-3.
Gutierrez OM, Farwell WR, Kermah D, Taylor EN. Racial differences in the relationship between vitamin D, bone mineral density, and parathyroid hormone in the National Health
and Nutrition Examination Survey. Osteoporos Int. 2011;22(6):1745-53.
Sempos CT, Durazo-Arvizu RA, Dawson-Hughes B, et al. Is there a reverse J-shaped association between 25-hydroxyvitamin D and all-cause mortality? Results from the U.S. nationally representative NHANES. J Clin Endocrinol Metab. 2013;98(7):3001-9.
Follow-up Questions and Comments
Dr. Holick noted that the role of sunlight is complicated by photophysics in that the sun's angle and its ability to penetrate ozone is important. Even at the equator, vitamin D production is very limited in the morning due to the sun's angle. In addition, ozone layer and nitric oxide levels affect people's ability to synthesize vitamin D. For these reasons, the common recommendation for people to spend 15 minutes outside every day is meaningless without specifying the time of day, season, latitude, and adjustments for skin pigmentation. Dr. Holick added that in a study of Nigerian women who were not heavily wrapped in clothing, serum 25(OH)D concentration averaged 40 ng/mL (100 nmol/L), a concentration that can be characterized as an evolutionary response that reflects the ideal.
Dr. Heaney commented that the lower serum 25(OH)D concentrations in obese individuals are not mysterious because they are a function of the distribution volume. If weight is adjusted for, the difference between obese and non-obese individuals disappears. Dr. Brannon responded that she was not certain that the distribution volume issue has been completely settled yet. Johanna Dwyer of Tufts University and the Office of Dietary Supplements asked if there are adverse events associated with the lower levels of 25(OH)D concentrations in the obese. Dr. Holick responded that he believed obesity increases the risk of vitamin D deficiency, and that he did not believe that 25-hydroxylation was impaired in obese individuals.
AFRICAN AMERICAN CASE STUDY: SERUM 25(OH)D AND BONE HEALTH
Presenter: John F. Aloia, M.D Winthrop University Hospital and Stony Brook University
Some people wonder whether the Dietary Reference Intakes (DRIs) for vitamin D should be race specific. If so, should they be higher or lower? Data from a recent study suggest that when measures of serum 25(OH)D concentrations for Africans and those of African descent are organized by latitude, groups living closer to the equator have serum levels in the range of 30 ng/mL [1]. In contrast, those farther from the equator (notably African Americans in the United States) have lower serum concentrations (slightly below 20 ng/mL). These results are similar to those of studies showing that persons with light skin and high sun exposure have higher concentrations of serum 25(OH)D than those with dark skin and low exposure [2]. Does this indicate that African Americans have a higher risk of deficiency than others? African Americans may have very similar concentrations of free 25(OH)D (unbound to vitamin D-binding protein) to European Americans [3], and this will be the subject of other presentations at this conference. However, consistent with the principles for other hormones such as testosterone and thyroxine, this may explain why African Americans, who have lower total serum 25(OH)D concentrations than whites, do not experience adverse consequences from these lower concentrations.
African Americans have better bone health measures, including bone mineral density and calcium retention, than whites. Furthermore, blacks have half the fracture risk and osteoporosis rates of whites [4]. Serum 25(OH)D concentrations in whites have the expected inverse relationship with parathyroid hormone (PTH), but this is not observed in blacks [5]. Moreover, trials have not shown that serum 25(OH)D prevents bone loss to a different extent in blacks and whites [6]. Notably, blacks have a lower calcium excretion rate than whites throughout life. Calcium retention is higher in black children
than white children, and this difference appears to continue during the growth spurt period [7,8]. PTH and 1,25(OH)D concentrations and bone formation rates are higher in adult blacks than whites, whereas bone resorption rates and urinary calcium concentrations are lower. In essence, adult blacks preserve the gain in bone they experienced earlier in life.
However, blacks may be more sensitive than whites to adverse effects of high serum 25(OH)D concentrations. Some emerging data, notably from the Women's Health Initiative, suggest that raising serum 25(OH)D concentrations in blacks increases fracture risk and all-cause mortality rates. Such findings are not definitive, and the studies do not provide sufficient proof of these adverse effects, but they raise a note of caution.
It is important to recognize and treat the truly deficient state, which is likely to be a serum 25(OH)D concentration of less than 12 ng/mL (30 nmol/L). When levels drop to this point, calcium absorption rates decline notably, suggesting a threshold effect associated with vitamin D and calcium absorption. At the same time, markers of bone turnover increase and, by all appearances, a substrate deficiency develops. Treatment is highly appropriate. However, attempting to increase serum concentrations of vitamin D in African Americans who are not deficient has no value and can be harmful. This is of particular concern because few clinicians seem to understand that the desirable concentrations of serum 25(OH)D reflect a distribution, as described by Dr. Carriquiry in her presentation. For this reason, the goal is not to ensure that every person in the population achieves the serum concentration needed by those who have the highest requirements (i.e., those at the 97.5th percentile of 25(OH)D needs).
This misunderstanding about the most appropriate goals for serum 25(OH)D concentration was incorporated into the work of Ng and colleagues, who examined the vitamin D dose-response relationship in African Americans [9]. The reported requirement was higher in this study than in previous studies. However, the researchers assumed that everyone should achieve the serum concentrations needed by persons with the highest requirement (i.e., the serum concentration conceptually similar to the Recommended Dietary Allowance (RDA) for intake, which reflects the 97.5th percentile of the distribution of needs). As a result of that assumption, the treatment (designed to ensure that everyone achieves the concentration of the 97.5th percentile of need) would actually produce concentrations that are much higher than the goal in many people, as shown in Figure 3-2. Widespread dosing to achieve the 97.5th percentile for the low end of the distribution would shift the entire distribution, with those at the top end of the distribution initially reaching even higher concentrations. The failure to understand this distribution model and, in turn, making efforts to ensure that all people achieve the RDA-like concentration (97.5th percentile) for serum 25(OH)D would raise the population's serum concentrations to levels that are much higher than the RDA-like concentration, which could be too high for some people.
Figure 3-2. Efforts to achieve 20 ng/mL serum 25(OH)D concentrations for all members of the population can cause a shift in the entire distribution of serum 25(OH)D.
Source: Brannon PM, Mayne ST, Murphy SP, Taylor CL. Vitamin D supplementation in African Americans: dose-response. Amer J Clin Nutr. 2014;100(3):982-4.
On this basis, the conclusion that African Americans should have higher serum 25(OH)D concentrations is not justified. And, in turn, there is little rationale for increasing the recommended intakes because this could lead to harms, at least potentially, in the form of increased incidence of fractures. The requirement and goals for serum concentrations should be the same for African Americans as for the rest of the population. In the meantime, researchers should continue to examine the dose-response relationship for vitamin D to clarify the relevant intake levels for benefit. We also need to await the outcomes of newer ongoing research focused on non-bone health benefits linked to vitamin D, especially those using a range of doses.
References
Durazo-Arvizu RA, Camacho P, Bovet P, et al. 25-Hydroxyvitamin D in African-origin populations at varying latitudes challenges the construct of a physiologic norm. Am J Clin Nutr. 2014;100(3):908-14.
Hall LM, Kimlin MG, Aronov PA, et al. Vitamin D intake needed to maintain target serum 25- hydroxyvitamin D concentrations in participants with low sun exposure and dark skin pigmentation is substantially higher than current recommendations. J Nutr. 2010;140(3):542-50.
Powe CE, Evans MK, Wenger J, et al. Vitamin D-binding protein and vitamin D status of black Americans and white Americans. N Engl J Med. 2013;369(21):1991-2000.
Barrett-Connor E, Siris ES, Wehren LE, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2015;20(2):185-94.
Gutierrez, OM. Recent insights into racial differences in bone and mineral metabolism. Curr Opin Endocrinol Diabetes Obes. 2011;18(6):347-51.
Aloia JF, Talwar SA, Pollack S, Yeh J. A randomized controlled trial of vitamin D3 supplementation in African American women. Arch Intern Med. 2005;165(14):1618-23.
Need AG, O'Loughlin PD, Morris HA, et al. Vitamin D metabolites and calcium absorption in severe vitamin D deficiency. J Bone Miner Res. 2008;23(11):1859-63.
Braun M, Palacios C, Wigertz K, et al. Racial differences in skeletal calcium retention in adolescent girls with varied controlled calcium intakes. Am J Clin Nutr. 2007;85(6):1657-63.
Ng K, Scott JB, Drake BF, et al. Dose response to vitamin D supplementation in African Americans: results of a 4-arm, randomized, placebo-controlled trial. Am J Clin Nutr. 2014;99(3):587-98.
AFRICAN AMERICAN CASE STUDY: GENETIC VARIANTS PERSPECTIVE 1
Presenter: Ravi I. Thadhani, M.D., M.P.H Harvard Medical School and Massachusetts General Hospital
It is well established that the major carrier of 25(OH)D in the serum is vitamin D-binding protein (DBP). The 25(OH)D metabolite, as with other hormones (e.g., testosterone), may also be present in the "bioavailable"—bound to albumin or free—form. Approximately 70% of 25(OH)D is bound to DBP, perhaps 10-20% is bound to albumin, and a very small amount is free. The available assays measure an aggregate of these three forms.
It is only recently that researchers have begun to understand that examining the bioavailable fraction of vitamin D more closely may be important. Seminal work in this area was carried out in the 1980s, when nutrition scientists recognized that total vitamin D concentrations in persons with liver disease could be misleading for determining deficiency. Such persons may have low total 25(OH)D but adequate free 25(OH)D. The free 25(OH)D could give them necessary vitamin D even though they have severe liver disease. Since that time, research interest in DBP and the bioavailable form of vitamin D has waxed and waned. However, this area is again experiencing resurgence.
One consideration related to DBP is often overlooked—that DBP is a negative acute phase reactant. Therefore, its concentrations decline during acute illness (e.g., sepsis), potentially explaining why vitamin D levels are low during acute and even sub-acute illness. However, many researchers conclude that when patients experience acute illness, they are vitamin D deficient and thus at risk of adverse outcomes. This conclusion has stimulated a number of studies suggesting that intervention in this setting is appropriate.
Although DBP is the major carrier of 25(OH)D, the 25(OH)D that is bound to albumin or is free is probably the primary source of the nutrient for cells. However, this does not mean that DBP does not have a role. Knockout animal studies have demonstrated that if DBP cannot be absorbed, vitamin D deficiency eventually follows and that DBP may act as a reservoir. The knockout animals become vitamin D deficient much more quickly with a vitamin-D-deficient diet than their wild-type counterparts. In other words, knocking out DBP knocks out the reservoir. However, profound deficiency does not immediately follow because other sources of 25(OH)D are either bound to albumin or free.
Studies in persons of African descent have made it possible to gather considerable evidence to link genotype (single nucleotide polymorphisms such as rs7041 and rs4855) with total 25(OH)D concentrations. The question is whether these differences in concentration are due to DBP levels per se, DBP's affinity, both, or something else. Moreover, parathyroid hormone (PTH) levels are quite similar across different populations, despite observed differences in total levels of 25(OH)D.
Other research conducted by our group indicates that although 24,25-dihydroxyvitamin D concentrations are higher in whites than blacks, the ratio of 24,25-dihydroxyvitamin D to 25(OH)D is almost identical in both populations. If a researcher argues that the 25(OH)D levels observed in African Americans reflect a deficiency, 24,25-dihydroxyvitamin D concentrations (a byproduct in the catabolic pathway of 25(OH)D) should be lower than the concentrations we observed. The findings do not suggest that deficiency does not exist, but rather than it might not occur until a very low level is reached. Furthermore, although the research is somewhat preliminary, it appears that bioavailable 25(OH)D concentrations are more strongly correlated than total 25(OH)D concentrations with PTH concentrations and bone mineral density.
A study we recently completed demonstrated that 25(OH)D levels are different in whites and African Americans, confirming the work of others. It also showed that DBP levels were different when measured with monoclonal assays than with polyclonal assays that produced over-readings. We described the DBP genotypes involved, noting that Gc1F, GC1S, and the "F" category were most common in African Americans. Furthermore, we and others have shown that Gc1F is also strongly linked with lower total levels of 25(OH)D, independent of DBP levels. Finally, we have observed that the bioavailable levels of 25(OH)D were similar in African Americans and whites. Of course, the appropriate assays for bioavailable and free 25(OH)D need further exploration and validation. However, given that African Americans have better bone health than whites, similar if not higher levels of serum calcium, and similar blood levels of PTH, African Americans do not show the same traditional evidence of vitamin D deficiency as whites.
In summary, it seems that free (or "bioavailable") 25(OH)D is important, at least to explore questions about vitamin D status. In turn, given what researchers know about bioavailable 25(OH)D, African Americans—who have lower total 25(OH)D concentrations but better bone health than whites— may not necessarily be deficient. African Americans may have lower reserves, however. Next steps should include developing improved assays for bioavailable 25(OH)D as well as conducting research to clarify why the SNPs result in differences in DBP.
AFRICAN AMERICAN CASE STUDY: GENETIC VARIANTS PERSPECTIVE 2
Presenter: Roger Bouillon, M.D., Ph.D. Katholieke Universiteit, Leuven, Belgium
This presentation focuses on genetic differences in vitamin D metabolism and action, especially those between African Americans and whites. There is extensive literature on the hereditary nature of vitamin D status. Studies in twins have suggested that 25-80% of variations in concentrations of serum 25(OH)D can be defined by genetic factors. Polymorphisms of several genes involved in the vitamin D pathway, such as CYP2R1, DBP/GCgenotypes, and CYP24A1, explain about 5% of the variation in serum 25(OH)D. This presentation also focuses on the role of vitamin D-binding protein (DBP). As noted in Dr. Thadhani's presentation, DBP binds all vitamin D metabolites and has other functions, such as a serving as a scavenger system for actin.
The structure of DBP includes three domains, often labeled A, B, and C. Domain A has a surface cleft that can bind 25(OH)D and other vitamin D metabolites. The polymorphisms that Dr. Thadhani mentioned reside farther away, in domain C. The polymorphism Rs7041 either codes for amino acid 432 as aspartic acid in Gc1f and Gc2 or for glutamic acid as Gc1s alleles. However, Rs4588 codes for amino acid 436 as threonine in Gc1f and Gc1s but as lysine in Gc2 alleles. Threonine in Gc1 is oxygen-linked with two or three carbohydrate moieties, but this glycosylation is not possible with lysine in Gc2.
Blacks have primarily the Gc1fgenotype, regardless of whether they live in Africa or in other countries. Most Europeans and most Asians have primarily the Gc1s genotype and, to a lesser extent, the Gc2 allele as well. The reasons for these genetic differences are not understood. However, germane questions are: Do the concentrations of DBP differ between blacks and non-blacks? Is this difference associated with race or genotype? Are there differences in DBP by genotype? Do such potential differences in DBP concentration or affinity result in differences in concentrations of free vitamin D metabolites?
Much of my information presented at this meeting is in process and has been generated in collaboration with either the investigators from Osteoporotic Fractures in Men, a prospective cohort study in elderly men, or investigators from the Medical Research Council at Cambridge University. Because assay methodologies are important, DBP was measured using a polyclonal assay with two-site ELISA (Genway), a polyclonal assay with single radial immunodiffusion (Leuven), and a monoclonal assay with sandwich ELISA (R&D;). In addition, free serum 25(OH)D concentrations were measured using a direct immunoassay (Future Diagnostics).
When we used the monoclonal R&D; assay, DBP concentrations were consistently about 50% lower in black populations in the United States and The Gambia than in U.S. or U.K. whites (who typically have the Gc1sand Gc2 genotypes). These results confirmed those of other studies that have used this DBP assay. When we used a polyclonal assay, however, there was no difference in DBP concentrations among genotypes, although we found a modest decrease in Gc2-2 carriers.
We previously found that the affinity of DBP for 25(OH)D or 1,25(OH)2D was not different, regardless of whether we tested in DBP/GC from Gc1f, Gc1s, or Gc2 homozygotes. Two other laboratories reached similar conclusions after using highly specific [3H]-labeled 25(OH)D or 1,25(OH)2D. In contrast, one French study found a two- to four-fold lower affinity for 25OHD in Gc1s or Gc2 homozygotes compared with Gc1f homozygotes. However, careful analysis of their methodology revealed that they used [3H]-vitamin D3 (and not the more polar metabolites) of low specific activity as a tracer, thereby raising questions about the validity of the affinity differences. It therefore seems highly likely that there are no differences in the affinity of 25(OH)D among the DBP/GC genotypes, which is in line with the results of in si/ico-modeling of DBP-25(OH)D holoprotein. Therefore, when we used different cohorts of white and black individuals, we found no significant differences in DBP concentration based on race/ethnicity or on DBP/GC genotype (except for a modestly lower DBP concentration in GC2-2 homozygotes, in line with previous studies). It is therefore highly likely that the monoclonal R&D; assay for DBP discriminates by genotype incorrectly.
The next important question is: What is the effect of genotype on free vitamin D concentrations? The first step to answer this question is to apply the law of mass action. If DBP concentration is the same in blacks and whites and the association between 25(OH)D and DBP is constant among the genotypes, the free concentration reflects the total 25(OH)D concentration. Therefore, the difference between the higher concentration of free 25(OH)D in The Gambia and the lower concentration in the United Kingdom is consistent with the difference between the total concentrations of 25(OH)D between these populations. African Americans in the United States have a lower free 25(OH)D concentration than U.S. whites because blacks have lower total 25(OH)D concentrations and similar DBP concentrations to whites. Moreover, free 25(OH)D and total 25(OH)D concentrations correlate well when the polyclonal assay is used. However, again, the monoclonal assay results in poor correlation and suggests differences by genotype. Finally, free 25(OH)D concentrations calculated from 25(OH)D and DBP (measured by polyclonal assays) agree very closely (>0.74) with concentrations of free 25(OH)D measured directly using the Future Diagnostic methodology. The short answer to the question about differences in free 25(OH)D concentrations is that differences do indeed exist, but they reflect differences in total 25(OH)D concentrations and are not due to differences by race/ethnicity or genotype.
In summary, free 25(OH)D, whether measured directly or calculated based on reliable DBP assays, is lower in African Americans than whites because African Americans have consistently low total 25(OH)D concentrations. When a monoclonal DBP assay is used, DBP concentrations in blacks (living in the United States or The Gambia) are underestimated, and, therefore, their free 25(OH)D is overestimated. In clinical practice, 25(OH)D concentrations below the thresholds of sufficiency as recommended by the Institute of Medicine should be addressed and corrected. Whether free 25(OH)D measurements are better than total 25(OH)D concentrations in predicting surrogate and hard clinical endpoints will require better standardization of measurements of free vitamin D metabolites and then appropriate clinical long-term observational or intervention trials.
DISCUSSION: AFRICAN AMERICAN CASE STUDY, GENETIC VARIANTS
Dr. Rosen opened the discussion by asking Dr. Thadhani if he had any comments in response to Dr. Bouillon's presentation. Dr. Thadhani said that he agreed with Dr. Bouillon that researchers need standardized assays for these emerging measures of interest. He indicated he had used the polyclonal antibody approach in his research but concluded that the method was over-recovering. He and his colleagues considered that the vitamin D-binding protein (DPB) might bind other related proteins, especially given that DBP is related to albumin and alpha-1 antitrypsin as well as other proteins. For this reason, they avoided using the polyclonal assay. Instead, they chose the Arnaud affinities, which are consistent with the Bikle affinities. They were concerned at the time that investigators were finding almost a 10-fold difference in affinities, depending on the buffers used. He noted that Dr. Bouillon's explanation in this session was extremely helpful.
Dr. Thadhani also commented that his group consistently finds a relationship between genotype and concentrations, meaning that in their work-independent of DBP concentrations and methods used—there is a strong relationship between genotype and 25(OH)D concentrations. It suggests some aspect of the genotype seems to dictate those concentrations. Others have reported this as well. He reported that a structural-chemist colleague even suggested that this difference in genotype could modify affinities and other relationships. However, researchers are not certain about these effects, and more studies are needed.
Dr. Bouillon agreed that additional studies are needed. He noted that his main message was that it would be unwise to conclude that low 25(OH)D concentrations are due to differences in DBP concentrations or, for this reason, that these low concentrations do not suggest any concerns about vitamin D status in African Americans. Dr. Bouillon fully agreed with Dr. Thadhani's conclusions regarding genetic influences on the link between polymorphisms, DBP, and 25(OH)D. What is confusing is that regardless of whether an investigator treats a patient with vitamin D or causes a vitamin D deficiency, the DBP concentration does not change; it does not depend on vitamin D status. Also, when an investigator manipulates the DBP concentration, 25(OH)D concentrations do not change. Therefore, free 25(OH)D appears to have no feedback regulation, in contrast to the tight feedback regulation of free 1,25(OH)2D. It is important to study this issue carefully before concluding that free 25(OH)D is biologically important.
Dr. Rosen asked whether Dr. Bouillon has examined the relationship between polymorphisms in bound 25(OH)D and free 25(OH)D in Africans. Dr. Bouillon replied that a study on this topic would be worthwhile, but such genetic studies likely require a large number of participants and have not been done.
Dr. Brannon asked about the differences between the response to bound and free 25(OH)D if the relevant tissue expresses megalin/cubilin. In recent research with macrophages that express megalin/cubilin, the immune response seemed to be related to the bound 25(OH)D. Dr. Bouillon replied that free 25(OH)D would be a factor if the uptake is important for extra-renal tissues; the issue is irrelevant for the kidney, which has a large supply of free 25(OH)D regardless of DBP concentration. But if DBP is needed for 25(OH)D uptake in cells (e.g., lymphocytes, monocytes, and osteoblasts), the free levels of 25(OH)D would be important. The data currently indicate that DBP sequesters excess 25(OH)D in keratinocytes, monocytes, and osteoblasts and inhibits 25(OH)D uptake activity. Dr. Brannon asked whether this suggests that the macrophage research of Martin Hewison at the University of California, Los Angeles, indicating the uptake of 25(OH)D was DBP related, is an outlier. Dr. Bouillon responded that Dr. Hewison's latest findings indicate that DBP sequesters the uptake of 25(OH)D and therefore inhibits 25(OH)D uptake in these cells.
Dr. Holick clarified that the 24,25-dihyroxyvitamin D is not biologically inactive. In fact, it is as active as 25(OH)D. Dr. Thadhani agreed, noting that he and his colleagues were simply examining the mechanisms of catabolism. However, evidence from patients with chronic kidney disease suggests that as 25(OH)D concentrations decrease, 24,25-dihydroxyvitamin D concentration also decrease; it serves as a type of barometer and was useful in this regard for his research.
Dr. Thadhani then responded to an earlier comment by Dr. Bouillon. Dr. Thadhani agreed that recommendations for clinical practice should not be based on only a few reports. Rather, research is in the nascent stages of understanding regarding the topic of genetic variants and bioavailable vitamin D.
Dr. Albanes from National Cancer Institute asked how to reconcile vitamin D's high heritability discussed in the presentations with genome-wide studies suggesting a heritability rate of only 5%. Dr. Bouillon responded that the differences in heritability are certainly a mystery. Large studies, with up to 50,000 samples, seem to explain only 5% of the variation in 25(OH)D concentrations, much lower that what might be expected considering the predictions from studies in twins. Moreover, the difference among Caucasian individuals, for example, can range from 10 to 90 ng. Clearly, inter-individual variation is enormous. The overall level in blacks might be somewhat lower, but the inter-individual variation is as large as in Caucasians. An important question, therefore, is why differences are so large among individuals.
Dr. Albanes asked whether details on the amino acid residues for the polyclonal and monoclonal assays have been published. Dr. Bouillon replied that information about some epitopes has been published, but the data are not readily available. A recent study on sex steroid-binding globulin is useful in that the globulin is very polymorphic. Some of the polymorphisms induce differences in binding to testosterone or estradiol to a greater or lesser degree, and commercial assays do not detect some of the polymorphisms. Dr. Thadhani added that polyclonal antibodies bind many different things in many different areas. Monoclonal antibodies are more precise, which is one reason why he has used them. Other fields of protein studies have also experienced a controversy about monoclonal and polyclonal antibodies, and even about similar or related monoclonal antibodies. In preeclampsia research, which involves placental growth factor, there has been considerable controversy as to whether the levels of this protein are high or low. Further examination showed that some antibodies bind the bound form and others bind the free form. It was not until this issue was resolved using a monoclonal antibody that the true levels of the protein could be identified. As a general matter, much work remains to be.
Dr. Hoofnagle reported that his laboratory has attempted, unsuccessfully, to detect free 25(OH)D and free 1,25(OH)2D directly. He asked whether any research team has observed free 25(OH)D in serum or plasma directly using mass spectrometry or whether the approach always involves tracer methods. Dr. Bouillon replied that the problems in detecting the free form are enormous because it is present in such small quantities compared to the total concentration. In addition, 25(OH)D adheres to plastic, glass, and other surfaces. Furthermore, if radioactive 25(OH)D is used, it might have a 1% impurity level, at best, which might be called "very good" even though a 1% impurity rate is 10 times higher than the amount existing as a free concentration. It is necessary to add sufficient 25(OH)D as a tracer in an amount that may be even higher than the endogenous concentration, which disturbs this equilibrium. Dr. Thadhani pointed out that the bioavailable form is largely driven by albumin, which may be easier to measure because of its size and quantity. He asked whether measuring 25(OH)D bound to albumin, as opposed to measuring the free form, would be a solution. Dr. Hoofnagle pointed out that his group has been trying to measure free vitamin D and are detecting very little if any of it. He estimated that less than 1 in 1,000 vitamin D molecules are free, given his limits of detection. Dr. Hoofnagle agreed that vitamin D is sticky, but it is possible to use heptane and other solvents to extract it from plastic and glass, which still does not result in detection of the free form. Overall, the inability to detect much free vitamin D is puzzling.
At the close of the session, Dr. Rosen announced that further discussion on Session 3's topics would take place later as part of a joint discussion with Session 4 presenters.
Session 4: The Uncertainties—What Do We Know About Vitamin D Intake and Supplement Use?
Session 4 addressed current understandings about vitamin D intake and supplement use as well as concerns about excess intakes and effects of increased serum 25(OH) concentrations.
CURRENT EXPOSURE TO VITAMIN D: FOOD, FOOD FORTIFICATION, AND SUPPLEMENTS
Presenter: Valerie Tarasuk, Ph.D. University of Toronto
This presentation focuses on the nature and distribution of vitamin D intakes. Nutrient intakes are often used as measures of status. Measures of vitamin D status based on intakes are somewhat different from measures of status focused on physiological parameters, such as serum 25(OH)D concentrations, as discussed by Dr. Carriquiry in Session 3 of this conference.
Expert committees convened by the Institute of Medicine (IOM) have recommended assessing the adequacy of dietary intake by determining a nutrient's usual intake and comparing that intake to the distribution of requirements for the nutrient [1,2]. In this approach, the prevalence of inadequacy is the proportion of the population with an intake below the estimated average requirement (EAR). Figure 4-1 shows a requirement distribution compared to an observed distribution of usual intakes, and illustrates a situation in which the prevalence of inadequacy is low.
Figure 4-1. Illustration of relationship between estimated average requirement and usual intake: Prevalence of inadequacy is low when the distribution of usual intakes is above the estimated average requirement.
On the other hand, when usual intakes cluster below the EAR, the prevalence of inadequate intakes increases (Figure 4-2). Data from the National Health and Nutrition Examination Survey (NHANES) and other sources suggest that the mean vitamin D intake from food and beverages falls significantly below the 10 g/day EAR from the IOM [3], suggesting—on the basis of intake estimates—a high prevalence of inadequacy.
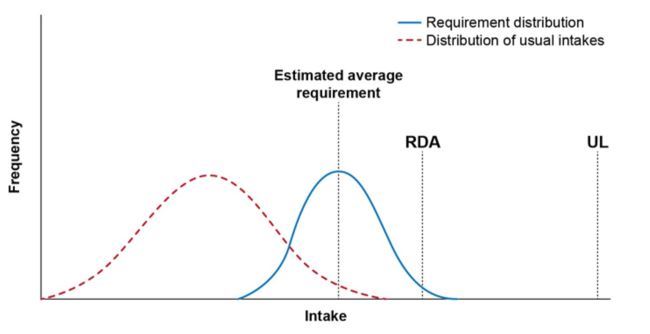
Figure 4-2. Illustration of relationship between estimated average requirement and usual intake: Prevalence of inadequacy is high when the distribution of usual intakes is below the estimated average requirement.
Most vitamin D intake appears to come from fortified foods, but even high levels of fortified- food consumption are associated with a high prevalence of inadequacy [4,5]. Data from NHANES show some variation in the use of vitamin D supplements by age and gender, but use of vitamin D supplements is substantial only among older adults. Overall, whether intakes are primarily from foods or supplements, they differ by age, gender, race, and income. However, the prevalence of inadequacy on the basis of reported intake is very high across all groups, even among supplement users. In short, when the measure of adequacy is intake, evidence indicates a substantial prevalence of vitamin D inadequacy—approximately 70%—across the U.S. population. This observation has led to calls for interventions, such as enhanced fortification programs.
In contrast to intake measures, the use of serum measures to estimate inadequacy results in much lower estimates. These discrepancies greatly complicate considerations about interventions, as of course do the debates about the appropriate threshold for demarcating inadequacy. The key concern is the magnitude of the difference between vitamin D status based on intake versus serum measures. A person might assume that one of these measures must be incorrect. However, there are possible explanations for at least some of these differences. Sun exposure and the resulting cutaneous synthesis, for example, are reflected by serum concentrations but are not captured by intake estimates. Nonetheless, some experts, including Dr. Heaney [6], have suggested that this is unlikely to account for very much of the discrepancy.
An emerging body of literature suggests that vitamin D intake from food sources may be underestimated, perhaps by quite a bit. A recent analysis of the vitamin D content of milk in the United States, for example, suggests that the fortification levels used in practice are much higher than those recommended in guidelines and listed on labels [7]. Milk is a primary contributor of vitamin D to the diet, especially for children, and it might provide much more of the nutrient than experts have realized. Research has also explored the amount of vitamin D in the activated form, 25(OH)D, in foods. The values for vitamin D in current food composition tables do not take into account amounts that may be present in foods (primarily animal-derived foods) as 25(OH)D and are instead based only on the amounts of the parent form of vitamin D. 25(OH)D can provide a great deal of vitamin D to the body. Because these additional sources of vitamin D activity are not included in the composition tables, the values from the tables are very likely to be underestimates of the true contribution of vitamin D from food. If these additional sources of vitamin D activity were to be taken into account in the tables, estimates of intake would increase notably by perhaps 2.9 pg/day for men and 1.7 pg/day for women, according to one analysis [8].
Research in Ireland also offers an interesting explanation for the discrepancy between status based on intake versus serum measures [9]. Most food analyses focus only on the vitamin D3 form. An analysis of the Irish national survey indicated, however, that vitamin D2 (found in supplements and yeast-related products or supplements) may contribute more to vitamin D intakes (1.7-2.3 pg/day) than many researchers have believed.
Finally, a bourgeoning literature has shown that dietary intake overall tends to be underreported. Estimates vary, but 10-40% of the 24-hour recall data in NHANES appear to reflect underestimated food intakes. The extent to which this affects vitamin D status is not known, but underreporting could be partly responsible for the low estimates of vitamin D intake.
One issue that is probably missed in explaining the discrepancy is the discretionary fortification of foods with vitamin D. In response to publicity about scientific findings and reports in the popular literature on the potential health benefits of vitamin D, food manufacturers have fortified more foods with vitamin D and marketed these foods aggressively to consumers. These foods include more conventional products (e.g., yogurts, cereals, and juices) as well as energy drinks, iced coffees, and vitamin waters. These newer fortification practices undoubtedly contribute a great deal of vitamin D to the U.S. food supply. However, the increased vitamin D content of these fortified foods is likely not captured in the current food composition tables because updating has been hampered by lack of resources.
Overall, it would appear that the U.S. population probably consumes more vitamin D than intake estimates suggest, and these intake estimates therefore do not provide a solid foundation for decisions about fortification or other interventions.
At this time it is also worth noting that the U.S. Food and Drug Administration (FDA) does not currently require manufacturers to list vitamin D content on nutrition facts panels, unless the food label makes a claim about vitamin D. However, in 2014, as part of a proposal to update the nutrition facts panel, FDA asked for comments about the appropriateness of requiring manufacturers to list vitamin D content. If this change occurred, it would make the vitamin D content of foods more visible to consumers and could cause manufacturers to add vitamin D to more foods. The FDA is also proposing to increase the Daily Value (DV) for vitamin D from 10 to 20 pg/day. If this change goes into effect, the denominator for the percentage of the DV for vitamin D in the nutrition facts panel will double. In turn, manufacturers that currently fortify their foods to a certain percentage of the DV or to levels that permit them to make the claim that a food is a "good source" or "excellent source" of vitamin D will need to add twice as much vitamin D to continue these practices. What this will mean to the population's overall exposure to vitamin D is unknown. A recent modeling study suggested that the proposed DV change would have only a modest effect [10]. However, this analysis probably underestimated the true effect of the change because it did not capture all of the current fortification practices, and because the assumptions about manufacturers' behavior apparently missed some important considerations.
In conclusion, estimated vitamin D intakes in the United States indicate much lower levels of vitamin D inadequacy than physiological measures based on serum 25(OH)D. This discrepancy should give pause to those who call for population interventions based on intake. Furthermore, the vitamin D intake scene is very dynamic, with the potential for increased intakes because of the ever-expanding discretionary fortification and the potential changes to the U.S. nutrition label on foods.
References
Institute of Medicine. Dietary Reference Intakes: Applications in Dietary Assessment. Washington,
DC: The National Academies Press; 2000.
Institute of Medicine. Dietary Reference Intakes: Applications in Dietary Planning. Washington, DC: The National Academies Press; 2003.
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Fulgoni VL 3rd, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J Nutr. 2011;141:1847-54.
Wallace TC, Reider C, Fulgoni VL 3rd. Calcium and vitamin D disparities are related to gender, age, race, household income level, and weight classification but not vegetarian status in the United States: analysis of the NHANES 2001-2008 data set. J Am Coll Nutr. 2013;32(5):321-30.
Heaney RP, Armas LA, French C. All-source basal vitamin D inputs are greater than previously thought and cutaneous inputs are smaller. J Nutr. 2013;143(5):571-5.
Patterson KY, Phillips KM, Horst RL, et al. Vitamin D content and variability in fluid milks from a US Department of Agriculture nationwide sampling to update values in the National Nutrient Database for Standard Reference. J Dairy Sci. 2010;93:5082-90.
Taylor CL, Patterson KY, Roseland JM, et al. Including food 25-hydroxyvitamin D in intake estimates may reduce the discrepancy between dietary and serum measures of vitamin D status. J Nutr. 2014;144(5):654-9.
Cashman KD, Kinsella M, McNulty BA, et al. Dietary vitamin D2—a potentially underestimated contributor to vitamin D nutritional status of adults? Br J Nutr. 2014;112(2):193-202.
Murphy MM, Spungen JH, Barraj LM, et al. Revising the Daily Values may affect food fortification and in turn nutrient intake adequacy. J Nutr. 2013;143:1999-2006.
Follow-up Questions and Comments
Dr. Holick pointed out that 25(OH)D is generally recognized as safe, and most animal feeds in Europe and the United States contain it. Dietary supplements in the United States do not contain 25(OH)D, but the 25(OH)D in chicken, pig, and cow feed could explain the apparently greater presence of 25(OH)D in foods derived from these animals.
Dr. Heaney commented that the data Dr. Tarasuk presented explain why his study used an equivalence of 1,000 IU/day vitamin D to support a 10 ng/mL increase in the 25(OH)D serum level. The associated equation is suitable for a broad range of intakes and serum concentrations. Dr. Heaney noted, however, that his group did not realize that they had not adequately measured contributions from basal sources. He then commented that Dr. Holick's research suggests that supplements are a source of vitamin D2 in the U.S. diet, while Dr. Tarasuk had cited studies suggesting that there might be some natural vitamin D2 sources beyond certain kinds of mushrooms. Dr. Holick responded that more vitamin D2 is apparently being introduced into the U.S. food supply now than in the past. He and his colleagues have found it in farmed salmon, where it presumably originates from their feed. Yeasts used by major fast-food chains increasingly contain vitamin D2. As a result, breads and other leavened grain products contain vitamin D2, but this contribution has not been reflected in the values used on food labels.
Dr. Heaney asked whether current assays can measure vitamin D2 concentrations as well as vitamin D3 and 25(OH)D. Dr. Holick responded that a subsequent presentation would discuss liquid- chromatography—mass spectrometry, which can distinguish vitamin D2 from vitamin D3. Samples he measured from 2006 to 2009 had very little detectable 25(OH)D2.
Dr. Tarasuk asked whether potentially unrecognized sources of vitamin D could be sufficient to account for the discrepancy between status based on intake assessments versus serum concentrations. Dr. Holick replied that these unrecognized sources are definitely sufficient to account for the discrepancy. Evidence showing that blood levels (mainly in whites) do not drop below 19 ng/mL in the winter imply that most vitamin D comes from other dietary sources. Sunlight contributes approximately 10 ng/mL on average.
Johanna Dwyer from the Office of Dietary Supplements referred to the modeling study on Daily Value (DV) changes and wondered if that publication had actually had as one of its goals the estimation of how much vitamin D manufacturers would add. She then asked Dr. Tarasuk's opinion on how much vitamin D manufacturers are likely to add to their products if the proposed DV change for vitamin D takes place. Dr. Tarasuk replied that manufacturers of cereals and other products that are marketed with health claims will probably add as much vitamin D as they need to in order to support nutrient content claims. She predicted a systematic increase in vitamin D fortification of cereals, and the vitamin D concentrations in energy drinks and other products might increase when the denominator for the DV changes. Dr. Tarasuk also predicted a broad spread of the distribution of intakes based on exposure as a result of the DV change.
FACTORS INFLUENCING SERUM 25(OH)D CONCENTRATIONS
Presenter: Sue A. Shapses, Ph.D., R.D. Rutgers University
This presentation addresses all sources of vitamin D, including dietary, oral supplementation, and sun exposure, as well as dose, initial baseline serum concentrations, and daily/weekly intakes. I will also describe types of vitamin D administered and seasonality of intakes.
**Serum 25(OH)D Response to Intake++
Data from the National Health and Nutrition Interview Survey (NHANES) indicate that the mean serum 25(OH)D concentration in the United States is about 23 ng/mL. The Institute of Medicine (IOM) in its recent report on vitamin D defined 25(OH)D concentrations below 20 ng/mL as low, below 12 ng/mL as deficient, and between 20ng/mL and 50 ng/mL as sufficient [1]. The IOM committee reviewed studies of the response to vitamin D intake, including those conducted in winter at a high latitude and with minimal sun exposure. It found that in children, younger adults, and older adults, increases in serum 25(OH)D concentrations in response to total dietary vitamin D intakes were similar, and concentrations in all age groups leveled off at higher intakes. In the studies reviewed, total vitamin D intakes were as high as 2,400 IU/day. More recent studies have examined even higher vitamin D intakes.
There are a number of notable points from several key studies. Research in the Antarctic among individuals experiencing virtually no sun exposure showed that, without supplementation, 25(OH)D concentrations decreased dramatically in the winter compared to the concentrations in the summer. People with the highest baseline 25(OH)D concentrations had the greatest decreases in the winter months [2]. A dose-response study in postmenopausal women who used supplements containing up to 4,800 IU/day of vitamin D showed that the increase in 25(OH)D concentration began leveling off after intakes exceeded 1,600-2,000 IU/day [3]. Furthermore, the authors of a newly published study concluded that the curve for African Americans appeared to be very similar to that of the white population. Other studies have demonstrated that baseline 25(OH)D concentrations influence responses to vitamin D supplementation. These studies have also shown that the response to supplementation is more dramatic in those with a low 25(OH)D concentration (less than 15 ng/mL) to start with than in those with a higher initial concentration. An update of an Agency for Healthcare Research and Quality (AHRQ) systematic review included 76 placebo-controlled, open-label trials examining 25(OH)D serum responses to vitamin D doses of up to 10,000 IU/day [4]. Responses varied three- to four-fold. Overall, serum 25(OH)D concentrations increased by 2 nmol/L for each 40 IU/day vitamin D from supplements. A study with 17,614 healthy adult volunteers showed that serum 25(OH)D concentrations increased by 12 nmol/L per 1,000 IU vitamin D when the daily dose was 1,000 IU/day or less but increased by only 1 nmol/L per 1,000 IU vitamin D when the daily dose was 15,000-20,000 IU/day [5]. Study participants had a higher mean baseline 25(OH)D concentration (about 90 mmol/L or 36 ng/mL) than starting concentrations in many older studies. Overall, vitamin D concentrations are likely to level off with increased intake and variability among groups.
Interestingly, the frequency of administration of vitamin D appears to affect serum response. In older adults taking oral vitamin D3 doses of 600 IU/day, 4,200 IU/week, or 18,000 IU/month or a placebo for 4 months, 25(OH)D concentration increases were similar in response to daily and weekly dosing [6]. Responses to monthly dosing were slightly but significantly below those for daily and weekly dosing, but responses to all dosing regimens were superior to responses to placebo. In young adults, daily and weekly doses of vitamin D were equally effective at increasing 25(OH)D concentrations. Older women who had undergone hip-fracture repair had similar responses to vitamin D supplementation, regardless of whether it was provided daily, weekly, or monthly [7]. One large study provided an annual dose of 500,000 IU of cholecalciferol versus placebo to women aged 70+ years. In contrast to expectations, the supplemented women had more falls and fractures, especially in the first 3 months
. These studies show that research on timing of dose administration may require special consideration of participant compliance. In any case, daily and weekly dosing with vitamin D increases serum concentrations equally. Monthly dosing has a similar or slightly attenuated effect, and an annual dose seems problematic.
Relative to the form of vitamin D, specifically vitamin D2 versus D3, a classic early study found no difference between the effects of vitamin D2 and D3 supplementation on 25(OH)D concentrations over 12 weeks. More recently, an AHRQ review concluded that the use of ergocalciferol (D2) in place of cholecalciferol (D3) results in a smaller increase in 25(OH)D [4], as did another systematic review conducted by the Biancuzzo group [9]. At this point in time, vitamin D2 and vitamin D3 appear to increase serum 25(OH)D concentrations to a similar extent, and the slight difference is probably not a major concern with respect to which form to choose for treatment.* Serum 25(OH)D Response in Sub-Populations *The relationship between body weight and serum 25(OH)D concentrations has also received attention. The 25(OH)D concentrations in obese individuals tend to be lower than those of non-obese individuals, and concentrations decrease in a graded way as body weight increases. In a study of parathyroid hormone (PTH) and 25(OH)D concentrations in people with obesity, our group found that the 25(OH)D concentration at which PTH is maximally suppressed is lower (11 ng/mL) in people with obesity than in the general population (22 ng/mL) [10]. The high serum PTH concentrations in persons with obesity are not likely due to low serum 25(OH)D concentration. Another research group showed that body weight affected responses to vitamin D supplementation, in that underweight individuals had a greater 25(OH)D response than those who were obese [5]. These investigators recommended administering two to three times as much supplemental vitamin D to those with obesity as in those of normal weight to achieve the same serum 25(OH)D concentration. However, they emphasized that whether such doses improve health outcomes is unclear.
A review of 144 cohorts from 94 studies found that body weight was the strongest predictor of variation in 25(OH)D concentrations and explained 35% of this variation [11]. To achieve a 20 ng/mL 25(OH)D concentration, a 50-kg person requires up to 400 IU vitamin D, but a 100-kg person needs approximately 700-800 IU. Achieving a concentration of 30 ng/mL requires about four times as much vitamin D for an obese person compared to a non-obese person. Furthermore, people who are obese have an attenuated 25(OH)D response to ultraviolet light (sun) exposure.
A related issue is weight loss. Weight loss from gastric bypass surgery does not appear to increase or decrease serum 25(OH)D concentrations. However, gastric malabsorption associated with the procedure confounds the ability to associate weight loss with changes in serum 25(OH)D concentrations. Another study found no standard dose-response relationship for increasing body weight loss, but greater amounts of weight loss led to an increase in 25(OH)D serum concentrations. Weight loss by diet alone, exercise alone, or both diet and exercise all resulted in a rise in 25(OH)D concentrations. In a study published last year, our group examined serum 25(OH)D responses to 2,500 IU/day vitamin D or placebo during weight loss or weight maintenance. Concentrations of 25(OH)D rose by twice the amount (8 ng/mL) in those who lost weight than in those who maintained their weight (4 ng/mL) [12].
Serum-concentration responses to vitamin D supplementation do not appear to vary by race. One research team reported that even though white women in the study had slightly higher 25(OH)D concentrations at baseline, these women's response to supplementation was similar to those of black women [13]. Responses did not vary by age either, and 24-hour urine-calcium responses to vitamin D supplementation did not vary by race. These findings suggest that altering oral supplementation dose by race is unnecessary. Observational data show that 25(OH)D concentration has different relationships to fracture incidence among African Americans and whites. Such studies also show that the confidence intervals for the effects of 25(OH) serum concentrations on glucose, blood pressure, and mortality are more variable in African Americans than whites. However, much more analysis needs to be done, such as studies of vitamin D-binding protein (DBP) polymorphisms and the role of free and bioavailable vitamin D in blacks and whites.
Studies have also assessed the relationship between gender and response to vitamin D supplementation. One study found a steeper slope in the response curves for vitamin D intake or supplementation in women than in men, regardless of correction for body mass index or baseline concentrations of 25(OH)D [14]. Therefore, vitamin D supplementation appears to raise 25(OH)D concentrations to a lesser extent in males than in females.* Impact of Sun Exposure *Another important factor affecting 25(OH)D concentrations is sun exposure. A study in Brazil provides evidence that serum 25(OH)D concentration fluctuate to a greater extent in response to sun exposure in young people than in older individuals, perhaps because older people have less sun exposure [15]. The effects of seasonal variations in exposure are slightly lower in females than males, possibly because men have more sun exposure. The effects are also less evident in nursing home residents than in those living in the community and in those who are sedentary than in those who are physically active. A carefully conducted trial in the United Kingdom found that seasonal variations in 25(OH)D concentrations from sun exposure were significantly lower in South Asians than in whites [16]. Measuring the effects of sun exposure on 25(OH)D concentrations is challenging because exposure differs by such factors as whether the person lives in an urban area or is exposed to ozone pollution, as well as the sun's angle.
In summary, the effect of vitamin D intake on serum 25(OH)D concentration is influenced by diet, supplement use, and sun exposure. Low concentrations of 25(OH)D rise by about 2 nmol for each pg of vitamin D consumed. In people with obesity, concentrations rise by 0.5-2 nmol/pg vitamin D supplementation. The serum increase is attenuated when 25(OH)D concentrations are higher or vitamin D doses are greater. Seasonal variation in 25(OH)D concentrations differs by population. Doses of vitamin D supplements in the obese population probably need to be at least twice the amount required to achieve the same 25(OH)D response in non-obese individuals. Weight loss increases 25(OH)D concentrations. The responses of 25(OH)D concentrations to vitamin D supplementation are similar among people of different races. The effects of sun exposure on 25(OH)D concentration differ by race and obesity status. Elderly and younger persons appear to have similar 25(OH)D responses to oral vitamin D intakes.
There are two final points I would like to add. First, people also need calcium for bone health, and a balanced intake of calcium is as important as a balanced intake of vitamin D. Second, although fortification is one way to provide routine, universal vitamin D supplementation, this approach has associated costs and could have unintended consequences. Adding vitamin D content to the nutrition facts panels on food labels could encourage companies to fortify more foods with vitamin D. If this occurs, micronutrient imbalances may result. Folic acid fortification, for example, increased the number of people, especially those who are elderly, with a low blood concentration of vitamin B12 that is associated with cognitive impairment. Nutrition scientists should be concerned about the effect on other micronutrient concentrations when they recommend raising vitamin D concentrations in the blood.* References *Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Smith SM, Gardner KK, Locke J, Zwart SR. Vitamin D supplementation during Antarctic winter. Am J Clin Nutr. 2009;89(4):1092-8.
Gallagher JC, Sai A, Templin T 2nd, Smith L. Dose response to vitamin D supplementation in postmenopausal women: a randomized trial. Ann Intern Med. 2012;156(6):425-37.
Newberry SJ, Chung M, Shekelle PG, et al. Vitamin D and Calcium: A Systematic Review of Health Outcomes (Update). Evidence Report/Technology Assessment No. 217. (Prepared by the Southern California Evidence-based Practice Center under Contract No. 290-2012-00006-I.) AHRQ Publication No. 14-E004-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
Ekwaru JP, Zwicker JD, Holick MF, et al. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One. 2014;9(11):e111265.
Chel V, Wijnhoven HA, Smit JH, et al. Efficacy of different doses and time intervals of oral vitamin D supplementation with or without calcium in elderly nursing home residents. Osteoporos Int. 2008;19(5):663-71.
Ish-Shalom S, Segal E, Salganik T, et al. Comparison of daily, weekly, and monthly vitamin D3 in ethanol dosing protocols for two months in elderly hip fracture patients. J Clin Endocrinol Metab. 2008;93(9):3430-5.
Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303(18):1815-22.
Biancuzzo RM, Clarke N, Reitz RE, et al. Serum concentrations of 1,25-dihydroxyvitamin D2 and 1,25- dihydroxyvitamin D3 in response to vitamin D2 and vitamin D3 supplementation. J Clin Endocrinol Metab. 2013;98(3):973-9.
Shapses SA, Lee EJ, Sukumar D, et al. The effect of obesity on the relationship between serum parathyroid hormone and 25-hydroxyvitamin D in women. J Clin Endocrinol Metab. 2013;98(5):E886-90.
Zittermann A, Ernst JB, Gummert JF, Borgermann J. Vitamin D supplementation, body weight and human serum 25-hydroxyvitamin D response: a systematic review. Eur J Nutr. 2014;53(2):367-74.
Shapses SA, Sukumar D, Schneider SH, et al. Vitamin D supplementation and calcium absorption during caloric restriction: a randomized double-blind trial. Am J Clin Nutr. 2013;97(3):637-45.
Gallagher JC, Jindal PS, Smith LM. Vitamin D does not increase calcium absorption in young women: a randomized clinical trial. J Bone Miner Res. 2014;29(5):1081-7.
Cashman KD, Wallace JM, Horigan G, et al. Estimation of the dietary requirement for vitamin D in free-living adults >64 y of age. Am J Clin Nutr. 2009;89(5):1366-74.
Maeda SS, Saraiva GL, Hayashi LF, et al. Seasonal variation in the serum 25-hydroxyvitamin D levels of young and elderly active and inactive adults in Sao Paulo, Brazil: the Sao PAulo Vitamin D Evaluation Study (SPADES). Dermatoendocrinol. 2013;5(1):211-7.
Farrar MD, Kift R, Felton SJ, et al. Recommended summer sunlight exposure amounts fail to produce sufficient vitamin D status in UK adults of South Asian origin. Am J Clin Nutr. 2011;94(5):1219- 24.* Follow-up Questions and Comments *Dr. Dawson-Hughes noted that the conditions under which a person takes a supplement (i.e., with a meal or while in a fasting state) can influence the 25(OH)D serum response to vitamin D supplementation. When people take a vitamin D supplement while fasting, they absorb less than if they take the supplement with a meal. Meals containing fat are associated with even greater absorption of the nutrient than those with no fat. Research from her group has demonstrated a 32% increase in absorption of vitamin D when fat was present in the meal. She commented that meal conditions probably contribute to some of the variability found in many studies. Dr. Shapses thanked Dr. Dawson- Hughes for highlighting this issue.
POSSIBLE ADVERSE CONSEQUENCES OF HIGHER VITAMIN D STATUS: EMERGING EVIDENCE FROM OBSERVATIONAL STUDIES
Presenter: Demetrius Albanes, M.D.
National Cancer Institute, National Institutes of Health
The focus of this presentation is the diversity in the associations between vitamin D and cancer, notably the evidence related to prostate, colon, breast, and pancreatic cancers. The findings come primarily from observational serologic studies as well as recent genetic analyses. The provocative question for this presentation is: Are we witnessing the "beta-carotenization" of vitamin D? This question stems from earlier experiences in which a vitamin or nutrient initially believed to be beneficial and widely promulgated as such was later found to have some unanticipated detrimental effects.* Colorectal Cancer *The evidence that vitamin D is linked to a lower risk of colorectal cancer is very convincing. Most of 14 key prospective studies of 25(OH)D concentrations and colorectal cancer risk show an inverse association (Figure 4-3).
—i i 1 1 r—
0.5 1 1.5 2 2.5
Odds ratio and 95% confidence interval
Figure 4-3. Forest plot of association between 25(OH)D concentration and colorectal cancer risk from 22 prospective studies.
Source: D. Albanes.
The largest of these studies is the European Prospective Investigation into Cancer and Nutrition, which followed 520,000 Europeans for an average of about 4 years. An analysis of data from this study showed that cancer risk dropped with increasing quintiles of 25(OH)D concentration (odds ratio 0.58 for highest versus lowest quintiles) [1]. The Prostate, Lung, Colorectal and Ovarian Cancer Screening Study also found a strong ptrend of 0.02 for the inverse 25(OH)D/colorectal cancer-risk association [2]. In general, animal model and cell culture experiments support these observations and suggest mechanisms whereby 1,25(OH)2D bound to the vitamin D receptor (VDR) heterodimerizes with the retinoid X receptor and affect thousands of vitamin D response elements in the colon that are involved in cell growth regulation, including c-FOS and c-MYC. 1-Hydroxylase is expressed in the colon, and the antiinflammation impact of higher vitamin D status or detoxification of secondary biliary acids is relevant.
Yet despite this observational and laboratory evidence, an analysis of data from the Women's Health
Initiative found no effect of 400 IU/day vitamin D combined with calcium for 8 years on colorectal cancer incidence [3].* Prostate Cancer *In 2011, the Alpha-Tocopherol Beta-Carotene (ATBC) Cancer Prevention Study showed that men with higher circulating 25(OH)D had significantly greater prostate cancer risk than men with lower 25(OH)D concentrations, and the dose-response relationship was fairly convincing [4]. A forest plot of 22 studies (Figure 4-4) indicates that in contrast to colorectal cancer, a majority of studies show higher risks of prostate cancer for the highest vitamin D groups, and few studies show inverse associations.
Figure 4-4. Forest plot of association between 25(OH)D concentration and prostate cancer risk from 22 prospective studies.
Two earlier meta-analyses identified very modest associations between 25(OH)D concentrations and prostate cancer risk, with no difference in the effects of high versus low 25(OH)D concentrations. However, a 2014 meta-analysis produced a substantially higher risk estimate (i.e.,17%) for high versus low serum 25(OH)D concentrations.
The data used in these meta-analyses and forest plots are from prospective studies in which blood samples are collected years in advance of cancer diagnoses. An example is the Uppsala Study, which used a nested case-control design and showed a positive association between serum 25(OH)D concentration and prostate cancer risk that just reached statistical significance [5]. In 2014, a research group that combined data from Finnish, Norwegian, and Swedish cohorts found a U-shaped association between 25(OH)D concentrations and prostate cancer [6]. A lag analysis of the prostate cancer association by time to diagnosis in this study showed a striking inverse association (best described as a reverse-J curve) in the first 10 years of follow-up. The notably high incidence of prostate cancer for the very lowest 25(OH)D concentrations appears to be consistent with reverse causality due to the short interval from blood collection to diagnosis.
Our research group identified serum 25(OH)D signals for four genes that appear to play a role in prostate cancer risk: GC (the gene encoding DBPJ, DHCR7 (a cholesterol reductase), CYP2R1 (the key 25- hydroxylation enzyme), and CYP24A1 (a vitamin-D-metabolizing gene) [7]. These four genes explained only about 5% of the variation. Nonetheless, in the large Breast and Prostate Cancer Cohort Consortium, which included over 10,000 cases, we found that having more "low" vitamin D alleles was associated with a lower risk of aggressive prostate cancer but had no apparent association with prostate cancer that was not aggressive. Such unbiased "Mendelian-randomization" evidence adds to the serologic data showing an adverse association between higher vitamin D status and prostate cancer risk.
Several mechanisms could explain such an association. We have found that men with DBP concentrations that are higher than the median coupled with high 25(OH)D concentrations have an increased risk of prostate cancer [4]. This finding might be related to the megalin/cubilin complex, an endocytic plasma membrane protein that is important not only for vitamin D absorption but also for testosterone bound to sex hormone-binding globulin, which serves as a prostate cancer agonist. This possibility is potentially relevant to the interaction between a higher vitamin D-binding protein (DBP) concentration, higher 25(OH)D concentration, and higher prostate cancer risk, and it might be related to a correlation between higher 25(OH)D concentration and higher total testosterone concentration. For example, in a small clinical trial, men who took 3,000 IU/day vitamin D for a year had increased concentrations of total testosterone, bioavailable testosterone, and free testosterone. Moreover, cell- culture studies have shown that exposure to dihydrotestosterone and 1,25(OH)2D3 increases prostate cancer cell proliferation. Taken together, this evidence suggests a vitamin D-androgen interaction that reflects a viable potential mechanism for an adverse association between vitamin D and prostate cancer risk.
Overall, these new findings and remaining unknowns surrounding the relationship between prostate cancer and vitamin D suggest the need for caution regarding high-dose vitamin D supplementation in settings where prostate cancer is prevalent. No large trials on vitamin D and prostate cancer are underway. Until such data become available, we plan to analyze data on 11,000 cases and 18,000 controls as part of the Oxford nutritional/hormone biomarkers pooling project.* Pancreatic Cancer Our studies suggest a higher pancreatic cancer risk among men in the highest category of serum 25(OH)D concentrations who also have low serum DBP concentrations [8]. The Vitamin D Pooling Project corroborated this relationship in multiple cohorts [9]. The free 25(OH)D might not require DBP to enter cells, but once it enters cells, free 25(OH)D acts through the VDR on the nuclear response elements. This mechanism seems to be specific to pancreatic cancer and perhaps to other health outcomes. However, findings from a pooled analysis did not substantiate an elevated risk of pancreatic cancer at the very highest serum 25(OH)D concentrations (though this study did not measure DBP) [10]. If anything, the study found a higher risk only in the lowest category of 25(OH)D concentration. Therefore, the data on the relationship between vitamin and pancreatic cancer are mixed, and more research is needed to sort out the possible associations. Breast Cancer Early retrospective case-control studies pointed to a protective association between vitamin D and breast cancer risk. However, reverse causality was probably at play in that patients whose blood is drawn at diagnosis or soon thereafter may have very low 25(OH)D concentrations because of their cancer or their treatments. Overall, prospective studies have not found an association between breast cancer risk and serum 25(OH)D concentrations. For example, the Women's Health Initiative found a hazard ratio of 0.96 for breast cancer treatment with vitamin D and calcium versus placebo [11]. Summary of Vitamin D and Cancer *The relationship between vitamin D and cancer probably varies by disease site and provides opportunities for additional etiologic and mechanistic insights. Higher vitamin D concentrations are associated with a protective effect for colorectal cancer risk, but no randomized controlled trial data support this possibility. An analysis of data from the Women's Health Initiative found that the relative risk of breast cancer was significantly lower with vitamin D/calcium supplementation except at the highest levels of intake (600+ IU vitamin D) [11]. For colorectal cancer, the lowest risk was in the very highest exposure category. Risk was higher for all lower-exposure categories, in line with the inverse association found in observational studies. Only women with the lowest 25(OH)D status at baseline showed a reduced colorectal cancer risk in response to vitamin D supplementation.
The Vitamin D Pooling Project of Breast and Colorectal Cancer investigators will soon provide solid evidence based on thousands of cases from cohort-based, prospective nested case-control datasets on the relationship between vitamin D and these two cancer sites. Higher vitamin D status might have an adverse association with prostate and pancreatic cancer risk, and data are especially strong for a relationship with prostate cancer. Additional targeted mechanistic research is needed to provide insights into these observations. Research questions that need to be answered include:
How is it that exposure to higher 25(OH)D status lowers the risk of colorectal cancer but raises the risk of prostate cancer?
Is the explanation the androgen pathway, the megalin/cubilin absorption of testosterone and sex hormone-binding globulin, cell proliferation, or something else?
Does vitamin D status influence colonic inflammation or bile acid metabolism?* Other Health Outcomes Studies have not consistently shown a protective association between vitamin D and health outcomes other than certain cancers. Instead, these studies have shown a more complex U-shaped association, with interactions between vitamin D supplementation and baseline vitamin D concentrations. For example, the relationship between serum 25(OH)D concentrations and overall mortality risk is U-shaped, and the lowest risk of overall mortality is associated with 65-85 nmol/L 25(OH)D [12]. Data from the National Health and Nutrition Examination Survey (NHANES) show that cardiovascular mortality is much lower in people with 25(OH)D concentrations in the 25th to 75th percentiles, but the risk is much higher for those in the top (75th to 100th) quartile [13]. Safety of Vitamin Supplements *The idea that vitamin supplements are never associated with harm has been disproved by various clinical trials. The original ATBC Cancer Prevention Study showed that a seemingly innocuous pro-vitamin (beta-carotene) given at 20 mg/day could have harmful effects, in this case on lung cancer and incidence of mortality. This finding presented itself despite abundant evidence from the literature suggesting that intakes had no adverse outcomes. The Carotene and Retinol Efficacy Trial then went on to also demonstrate the increased risk for lung cancer with beta-carotene intake. In short, only large trials have the power to show both benefit and harm, effects that may be relatively small in magnitude.
An unexpected secondary finding of the ATBC trial was that a very modest intake (50 IU) of alpha-tocopherol was associated with a one-third reduction in prostate cancer incidence, particularly in advanced-stage cancer and prostate cancer deaths [14]. In contrast, the Selenium and Vitamin E Cancer Prevention Trial found that dietary supplements did not prevent cancer and, instead, that vitamin E supplements were associated with higher prostate cancer incidence [15,16]. However, dosages in the studies were different, and the baseline prostate cancer screening might have excluded potential participants with small, microscopic tumors that vitamin E could have affected. This type of issue underscores the fact that designing clinical trials can be complicated and requires careful thought and planning. For example, the timeframe of exposure to vitamin D with respect to the endpoint of interest is crucial, as is duration of exposure.
Although large trials are needed to show small adverse—as well as beneficial—effects of a dietary supplement, both human observational and trial data play a role in revealing the relationships between nutrients and health outcomes. Observational studies provide a range of data on circulating vitamin D concentrations at baseline, whereas randomized controlled trials usually administer a specified dosage. Overall, studies need to assess divergent associations across a wide range of health outcomes, consider the totality of the evidence across these outcomes, and detect the real possibility of differing associations for various endpoints. Integrating all of the emerging data and generating solid conclusions or recommendations for new studies will be needed.
References
Jenab M, Bueno-de-Mesquita HB, Ferrari P, et al. Association between pre-diagnostic circulating vitamin D concentration and risk of colorectal cancer in European populations: a nested case-control study. BMJ. 2010;340:b5500.
Weinstein SJ, Purdue MP, Smith-Warner SA, et al. Serum 25-hydroxyvitamin D, vitamin D binding protein and risk of colorectal cancer in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Int J Cancer. 2015;136(6):E654-64.
Wactawski-Wende J, Kotchen JM, Anderson GL, et al. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med. 2006;354(7):684-96. Erratum in: N Engl J Med. 2006;354(10):1102.
Weinstein SJ, Mondul AM, Kopp W, et al. Circulating 25-hydroxyvitamin D, vitamin D-binding protein and risk of prostate cancer. Int J Cancer. 2013;132(12):2940-7.
Brandstedt J, Almquist M, Manjer J, Malm J. Vitamin D, PTH, and calcium and the risk of prostate cancer: a prospective nested case-control study. Cancer Causes Control. 2012;23(8):1377-85.
Tuohimaa P, Tenkanen L, Ahonen M, et al. Both high and low levels of blood vitamin D are associated with a higher prostate cancer risk: a longitudinal, nested case-control study in the Nordic countries. Int J Cancer. 2004;108(1):104-8.
Mondul AM, Shui IM, Yu K, et al. Genetic variation in the vitamin D pathway in relation to risk of prostate cancer-results from the breast and prostate cancer cohort consortium. Cancer Epidemiol Biomarkers Prev. 2013;22(4):688-96.
Weinstein SJ, Stolzenberg-Solomon RZ, et al. Impact of circulating vitamin D binding protein levels on the association between 25-hydroxyvitamin D and pancreatic cancer risk: a nested case-control study. Cancer Res. 2012;72(5):1190-8.
Helzlsouer KJ; VDPP Steering Committee. Overview of the Cohort Consortium Vitamin D Pooling Project of Rarer Cancers. Am J Epidemiol. 2010;172(1):4-9.
Wolpin BM, Ng K, Bao Y, et al. Plasma 25-hydroxyvitamin D and risk of pancreatic cancer. Cancer Epidemiol Biomarkers Prev. 2012;21(1):82-91.
Chlebowski RT, Anderson GL, Lane DS, et al. Predicting risk of breast cancer in postmenopausal women by hormone receptor status. J Natl Cancer Inst. 2007;99(22):1695-705.
Melamed ML, Michos ED, Post W, Astor B. 25-hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168(15):1629-37.
Fiscella K, Franks P. Vitamin D, race, and cardiovascular mortality: findings from a national US sample. Ann Fam Med. 2010;8(1):11-8.
Heinonen OP, Albanes D, Virtamo J, et al. Prostate cancer and supplementation with alpha- tocopherol and beta-carotene: incidence and mortality in a controlled trial. J Natl Cancer Inst. 1998;90(6):440-6.
Lippman SM, Klein EA, Goodman PJ, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 2009;301- 39-51.
Klein EA, Thompson IM Jr, Tangen CM, et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 2011;306:1549-56.
Sessions 3 and 4 Joint Panel Discussion: Balancing Risk and Intervention
Dr. Mayne moderated a panel discussion that included the participants from Sessions 3 and 4.
Dr. Mayne began the panel discussion by correcting a misconception—that the Institute of Medicine (IOM) committee on dietary reference intakes (DRI) for vitamin D did not consider observational data.
As a member of the IOM committee, she explained that the Agency for Healthcare Research and Quality (AHRQ) systematic reviews described, organized, and rated observational data that the committee incorporated into its work. Because both observational and randomized controlled trial (RCT) data have strengths and weaknesses, it was important for the committee to carefully consider the totality of the evidence and assess its strengths and weaknesses.* Assessing Status in the Clinical Setting *Dr. Mayne suggested that, in the context of evidence-based decision-making for primary care, the task for this discussion might be to consider future directions for vitamin D research. Evidence shows that vitamin D has both benefits and harms, but the evidence on vitamin D outcomes is inconsistent and incomplete. Moreover, assaying serum 25(OH)D concentration, the measure that primary care physicians use to guide their decisions about vitamin D supplements, is challenging. Likewise, bioavailability and a host of other issues create an environment of uncertainty surrounding vitamin D. Furthermore, cut-points used to determine adequacy are not evidence-based or consistent across laboratories. Dr. Mayne noted that Dr. Carriquiry had described the use of z-scores and probabilities of inadequacy based on patient characteristics as alternatives to using cut-points. Dr. Mayne also stated that clinicians are generally familiar with z-scores, and endocrinologists in particular use them to interpret measures such as bone mineral density. She asked panelists for their thoughts about moving forward into primary care based on this conference's discussions so far.
Dr. Aloia said that laboratory reports on vitamin D status present a significant problem, in part because primary care physicians have limited time to review them. These reports usually include reference information using one column to show "normal" values and a second column listing "low" or "high" values. This is a concern because laboratories select their own "normal" values. Many laboratories seem to interpret available information incorrectly, such as turning to the IOM's Recommended Dietary Allowances (RDAs) for vitamin D and using the RDA as the bottom instead of the top of the normal range. He noted that Dr. Carriquiry had explained this very well. Unfortunately, no authoritative body is responsible for establishing these cut-points, so laboratories do this on their own. Issues surrounding the establishment and use of cut-points must be addressed to improve clinical decision-making.
Dr. Shapses supported the use of z-scores in primary care practice, noting that z-scores have been useful for bone measurement. and clinicians seem able to adapt to their use. A probability measure can be helpful when the data contain considerable uncertainties. Dr. Bouillon pointed out that vitamin D is a hormone precursor. Because people need a certain amount of vitamin D as a substrate, clinicians might need to use a specified threshold for adequacy, which would be about 20 ng/mL in adults. Dr. Bouillon said the use of a range did not appeal to him.
Neil Binkley from University of Wisconsin, Madison noted that he is a past president of the International Society for Clinical Densitometry and commented that the t-score was an advance in the field. However, he argued strongly against the use of t-scores or z-scores for vitamin D. Rather, he urged laboratories to improve the measurement of serum 25(OH)D and suggested giving concise guidance to primary care providers. He commented that using probabilities and z-scores to assess vitamin D adequacy in primary care would be disastrous. Clinicians would need to adjust these scores for age, sex, and race and make decisions about what is a normative database. Determining the standard deviation would be difficult.* Supporting Informed Decision-Making *Dr. Mayne asked panelists to next consider patient-based, informed decision-making. This conference had included graphics that convey information to patients, but she asked how these approaches can be operationalized for vitamin D. She added that operationalization may be difficult because vitamin D requirements are based on bone health, but vitamin D has other benefits and possible adverse effects. Moreover, communicating effectively with different segments of the population to support patient-informed decision-making is challenging when the science suggests that different populations have different risks and needs. African Americans, for example tend to have lower serum 25(OH)D concentrations but better bone health than whites. Personalized, informed decisionmaking is complex, and one approach might be more effective than others for certain interventions.
Dr. Bouillon stated that authorities in Europe do not generally have a favorable attitude toward dietary supplements. From his perspective, it is best to be simple. He noted that because there was unanimous agreement that infants need a vitamin D intake of 400 IU/day, there should be no discussion, and mothers must ensure this total intake. He also suggested that there is wide agreement on the amounts needed by the elderly, and it is therefore not necessary to engage in shared decision-making discussions with these individuals. Rather, in general, the goal is to ensure that the intake needs are met, although questions remain about who is responsible for achieving this goal. Dr. Bouillon suggested that different approaches would be required for different target groups, and that a community-based effort is needed. Attending physicians should address the needs of patients with a disease on a case-bycase basis.
Dr. Thadhani commented that based on earlier presentations at this conference, patients should be involved in decisions about interventions. Physicians ultimately treat a patient, not a serum concentration. The question is whether physicians should continue to ignore patients in favor of serum concentrations when making decisions about supplemental vitamin D. Both the IOM and the U.S. Preventive Services Task Force reports emphasized the need to focus on patients.
Dr. Montori said that ensuring that patients take recommended supplements and medications is challenging. Nonadherence rates are high and telling adults, particularly those who are healthy, that they must do something every day is inefficient. In the case of vitamin D, nutrition scientists do not agree that supplementation is potentially beneficial, and they have raised questions about its potential harms as well. For joint decision-making about vitamin D interventions, physicians must be able to tell patients their risk of adverse health consequences. The presentations and discussions at this conference indicate that the field has not advanced sufficiently to enable physicians to have those conversations with patients. Rather, the focus may need to be less on clinical care and more on public-health strategies.
Dr. Montori added that his experience suggests that, at times, shared decision-making may, unfortunately, take the form of presenting statistics in the office, including curves and standard deviations. This may overwhelm patients and is probably not very effective. However, similar to the development of a FRAX score for osteoporosis interventions, it might be possible to convert evidence into a score that allows physicians to discuss the risks associated with and without vitamin D treatment.* Vitamin D Alone or in Combination with Calcium Dr. Mayne, noting that the conversation had turned to fractures, referred to the data presented by Drs. Montori and Shapses showing that combinations of vitamin D and calcium are beneficial for bone health, but vitamin D alone has no effect. Therefore, the message from clinicians to patients might be that calcium and vitamin D are necessary to maintain bone health. Dr. Montori agreed, although he noted that taking too much supplemental calcium can have adverse effects, and vitamin D alone appears to be effective in preventing falls. Dr. Dawson-Hughes added that the difficulty of distinguishing the effects of calcium and vitamin D is exacerbated by the fact that trials that used higher doses of vitamin D also used calcium supplements. Dr. Mayne pointed out that the ongoing Vitamin D and Omega-3 Trial is assessing the effects of vitamin D alone, but the results are not yet available. At this time, bone health and fracture—the strongest indicator for vitamin D health outcomes—is best addressed through supplementation with both calcium and vitamin D, and not with vitamin D alone. Vitamin D Supplementation *Dr. Young remarked that groups that publish clinical guidelines would say that people with a 20% risk of cardiovascular disease over 10 years should take a statin. However, the vast majority of the conference's audience, when presented with the information on risk, had said that they would decline to take a statin. And of course, the information on the benefits and risks of vitamin D supplements is much weaker than that for statins. These reactions are examples of situations in which individuals disagree with the conclusions of guidelines bodies and choose to take different actions. He also commented that any problem with vitamin D has to be addressed in the public-health arena rather than by expecting members of the public to take supplements. Perhaps food fortification with vitamin D offers a solution because it prevents rickets and reduces the risk of falls in the elderly.
Dr. Mayne shared a question from an online audience member: Do people who benefit from vitamin D supplements or have adverse effects have anything in common? Dr. Mayne responded that people with very low serum 25(OH)D concentrations appear to benefit the most from supplements. This finding holds across different health outcomes, as shown from observational data. People with very high serum 25(OH)D concentrations, in contrast, have the greatest risk of adverse effects. In short, the risk curve for vitamin D supplements is U shaped. Of course, these observations might be affected by confounding. However, the data that Dr. Albanes presented earlier suggested that people with the highest vitamin D status at baseline had adverse effects, including an increased risk of certain cancers, after taking supplements containing vitamin D plus calcium. This finding cannot be a result of confounding, which was controlled in these trials. Given that expert groups have not recommended screening for vitamin D deficiency, Dr. Mayne wondered how to identify people at the low end of the serum distribution who might benefit from supplements.
Michael McCaskill from Tulane University said that he is a toxicologist who is very aware that "the dose makes the poison." If people at the very low end of the 25(OH)D serum distribution benefit from a vitamin D supplement, the focus should be on raising their serum 25(OH)D to an acceptable concentration. Supplementing those at the highest end of the distribution is wasteful because the impact is minimal and they might be vulnerable to adverse effects.* Racial/Ethnic Differences *Michael McCaskill then asked Dr. Albanes for insights into the information he presented suggesting that low concentrations of serum 25(OH)D among African American men are not associated with a reduced risk of prostate cancer, as is the case for whites. Dr. Albanes replied that studies do show that African American men have lower serum 25(OH)D concentrations but a higher incidence of prostate cancer than men from other ethnic/racial groups. Dr. Albanes and colleagues are still examining these outcomes, so he was unable to provide additional insights at this time.
Dr. Mayne pointed out that much of the available data come from studies in Caucasian populations. Therefore, there is a clear research need to determine whether other populations, including African Americans, have similar vitamin D response patterns. Unfortunately, the very limited data that are available for specific racial and ethnic groups are inconsistent.* Interpreting 25(OH)D Concentration Data *Christopher Sempos from the Office of Dietary Supplements asked how clinicians should take inflammation into account when interpreting 25(OH)D concentration data. Dr. Albanes replied that inflammation is likely an underlying factor in many morbidities and deaths. If vitamin D plays a role in health outcomes, clinicians should consider the impact of inflammation when interpreting data on serum 25(OH)D concentrations.
Dr. Mayne stated that earlier presentations had indicated that vitamin D and vitamin D-binding protein (DBP) concentrations seem to decline during the acute-phase response when patients enter the hospital, but the meaning of this information is not clear. Research needs to clarify how to interpret vitamin D concentrations not only in these acute situations, but also in the chronic setting when inflammation is present. This issue applies to a number of nutrients. Dr. Albanes added that vitamin D supplements can interact with other micronutrients (particularly at higher dosages) and with medications. When high-enough doses of supplements are administered, the same detoxifying cytochrome p450s affect all of these micronutrients.* Applications in Clinical Settings *F. Alex Pirie from the Immigrant Services Provider Group/Health at Tufts University said that communicating with and informing people who are vulnerable or economically disadvantaged or who do not speak English about complicated issues is difficult. This is especially true when the target audience is children, given the concerns about neurological and other developmental issues. He wondered how to communicate easily with communities that are most at risk of vitamin D inadequacy.
Dr. Carriquiry noted that physicians may not be able to understand and communicate probability of risk and likely need to be better educated on this topic. However, with respect to an earlier comment by Dr. Binkley, even if it is possible to measure 25(OH)D without error, individuals' concentrations will continue to be different, and appropriate concentrations for individuals will vary. These differences are due to several unavoidable factors, such as genetics, physiological conditions, and environment. In turn, these factors lead to a distribution of acceptable concentrations, not a single value associated with a desirable concentration. The cut-point approach will continue to be inappropriate regardless of how well one measures 25(OH)D because individuals do not have the same need. It is a simple fact of life. She agreed that healthcare providers should not talk about t tables and plus-or-minus standard deviations with patients. However, providers should find a way to communicate probabilities and uncertainties to patients. The fact that this is not being done well now does not mean that clinicians should not try to do a better job.!!!Session 5: The Uncertainties—What Are Issues
Surrounding Laboratory Measures of Serum 25(OH)D?
The measurement of serum 25(OH)D concentrations faces many challenges. This session identified uncertainties surrounding the measurement assays and included a panel discussion focused on the implications of these uncertainties for clinical practice.
MEASUREMENT OF SERUM 25(OH)D: PERSPECTIVES FROM THE CLINICAL LABORATORY* Presenter: Andrew Hoofnagle, M.D., Ph.D. University of Washington *This presentation focuses on the accuracy and precision of the measurement of serum 25(OH)D concentrations as well as the need to promote standardization and harmonization for measurement. I set the stage for this topic by considering the case of a 56-year-old female who reports no stamina, exhaustion, knee pain, and an allergy to dairy products since age 5 years. Her mother experienced vertebral fractures at age 60 years. The first question is: Should the clinician test her serum 25(OH)D concentration? [About half the audience members raised their hands, indicating that they would refer the patient for a vitamin D laboratory test.] As an aside, I would note that the Centers for Medicare and Medicaid Services would not reimburse the patient, the clinician, or the laboratory for the costs of the test in this case study. There are no International Classification of Diseases (ICD) codes that legitimize reimbursement for the costs of screening this patient for vitamin D. However, if the clinician measured her serum 25(OH)D concentration anyway and the result was 20 ng/mL, the second question is: Would you treat her? [Fewer audience members raised their hands, but some indicated that they would treat this patient.] Again, as an aside, if a clinician did order a vitamin D supplement for this patient, neither Medicare nor Medicaid would cover this cost.
Let us consider a third question: How accurate is the assay used to measure this patient's serum 25(OH)D concentration?* Accuracy and Precision *For this discussion, the accuracy of a laboratory test is defined as the closeness in agreement between the true value (real or actual result) defined by nature and the value measured in the laboratory (test result). Because the laboratory has only one opportunity to complete the measurement, accuracy is fundamentally influenced by precision. Variability and imprecision exist within batches, between batches, and between laboratories. Bias is the systematic error that can occur in each batch due to calibration of the assay. In addition, researchers often overlook the role that sample-specific matrix effects may play in introducing bias. Precision is often eroded by reagent lot-to-lot variability, as shown by challenges experienced in the National Health and Nutrition Examination Survey (NHANES) when the survey replaced one lot of the DiaSorin radioimmunoassay reagent with another.
Importantly, imprecision inflates the confidence intervals surrounding the estimated cut-offs used to define vitamin sufficiency and deficiency. The Vitamin D Standardization Program specifies that an acceptable variance in assay precision is 10%. In practice, if the test value from an assay with this level of precision is 30 ng/mL, researchers can be 95% (not 100%) certain that the true value is between 24 and 36 ng/mL. This is not very comforting, given that clinicians making treatment decisions usually assume that vitamin D tests are considerably more precise. Although a second measurement might provide some clarity, clinicians rarely have the opportunity to conduct one and must make decisions based on a single measurement.
Available assays offer different levels of precision. Assays used to measure serum 25(OH)D can be grouped as follows:
Immunoassay and protein-binding methods: Rely on competitive protein binding
o Assays using a radioactive tracer (e.g., radioimmunoassay)
o Chemiluminescent assays labeled with light emitting tracer
High-pressure liquid chromatography (HPLC) methods: Rely on extraction and detection
o HPLC with ultraviolet (UV) detection
o HPLC with liquid chromatography-mass spectrometry (LC-MS) detection
The immunoassay, which has been used for quite some time, detects the concentration of a molecule—in this case, 25(OH)D—through the use of an antibody. This method non-covalently binds the antibody to a labeled analyte, or tracer. If present, 25(OH)D competes with the tracer and occupies the antibody-binding site instead of the tracer, reducing the amount of tracer bound to the antibody, and is thus detected.
Because the process is competitive, vitamin D immunoassays (and all small-molecule immunoassays) have a limitation because the antibody has affinities for different metabolites of vitamin D. These other metabolites could include the C3 epimer of 25(OH)D, 24,25(OH)2D, 1,25(OH)2D, and other dihydroxylated molecules. The binding of these molecules by the antibody in addition to 25(OH)D affects the measurement. In this situation, 25(OH)D cannot be uniquely detected using this methodology. Scientists ask a great deal of these antibodies, and the antibodies simply are not specific enough for these small molecules. Imprecision in measurement is a likely result.
Furthermore, many immunoassays face challenges in detecting D2 form of vitamin D. This may be of concern because our work suggests that the D2 form is clinically important. Our examination of the Multi-Ethnic Study of Atherosclerosis cohort revealed that more than one-third had serum 25(OH)D2 concentrations that contributed more than 5% to their total 25(OH)D concentrations. In our clinical population, serum 25(OH)D2 is the predeominant form of 25(OH)D in more than 20% of patients.
A proficiency-testing program associated with the College of American Pathologists assessed the ability of assays to detect vitamin D2. For the seven assays studied, recovery rates of serum 25(OH)D2 ranged from 40% to 120%. In a separate study, when one sample was spiked with 24,25(OH)2D3, we saw absurdly high recovery rates in some immunoassays. These results clearly suggested that the 24,25 form can compete for antibody-binding sites, leading to false measurement results for 25(OH)D, especially results that are too high. However, this experiment could have been affected by an artifact
because it was carried out in vitro, and the substance was spiked into a normal human sample. As a result, extremely high cross-reactivities with 24,25 in some of these immunoassays are likely to be artifactual. Our next step will be to study samples from healthy individuals, but the in vitro data will guide the next steps.
Now, let us turn back to our 56-year-old female. It is likely that if she had undergone another laboratory test using a different assay, the reported serum concentration would have been meaningfully different. Evidence shows that when an FDA-approved immunoassay is used in two different laboratories, the results can differ by as much as 40%. If assays are not harmonized, different clinics produce different results and, in turn, different treatment plans. A report from one laboratory may trigger use of a medication, whereas a report from a different laboratory for the same patient might lead to no treatment.
How do we fix these problems? The LC-MS methodology appears to have great value in ensuring precision and accuracy in research studies and clinical applications. The mass spectrometer, when paired with HPLC, is a very specific detector. The fundamental steps of chromatography involve injecting a sample onto a chromatographic column, followed by the separation and elution of the molecules of interest. MS makes it possible to select for specific mass-to-charge ratios. It is possible to select a specific precursor mass in the first quadrupole, fragment the molecules in a collision cell, and then select specific fragments in another quadrupole. In short, this process results in the correct precursor mass and fragment mass. Furthermore, if the fragments are eluted from the column at the correct time, three dimensions of specificity are the result.* Harmonization and Standardization *The next concern is harmonization of assays, which can be defined as "trying to make things as similar as possible." Reported measures might not hit the bull's eye exactly, but the measures should be close together. Ideally, two different platforms in the same laboratory produce the same result, or the same platform in two different laboratories gives the same result. This can be achieved by use of reference materials (even if not a certified material), cooperation through formation of a consortium, or recalibration to the results from a single, central laboratory. However, although these efforts determine which answer is "right" and encourage all laboratories to calibrate their assays to obtain the same answer, the result is not necessarily the true value. This leads to the question of standardization.
The goal of standardization is for all platforms used in all laboratories to produce the same true result—that is, to hit the bull's eye every time. Standardization requires certified reference materials or at least calibration materials that are traceable to a certified reference material. Ideally, all or as many clinical laboratories as possible participate in the standardization effort to ensure that the right answer is obtained when the assays are carried out. Examples of such programs in other fields include the Hormone Standardization Program administered by the Centers for Disease Control and Prevention and the Hemoglobin A1c Standardization Program. Another example is the Vitamin D Standardization Program, which has made great strides in improving vitamin D assays. A key component of standardization is a set of pre-established criteria for assays calling for a minimum quality level, use of commutable materials, and a basis in clinical need.
As a final note relevant to harmonization and standardization of assay outcomes, there is the related question of a reference range for the measures reported. Dr. Aloia earlier pointed out that laboratories currently set their own reference ranges. It is true that clinical laboratories in the United States use the scientific literature to define their own reference ranges. It would, of course, be ideal if clinical laboratories had guidelines for reference ranges, but no such guidelines are available for vitamin D. In addition, research must define the health outcomes that drive the determination of the cut-off
values or reference ranges. The discussions at this conference indicate that the field has some work to do to reach this goal.* Proficiency Testing *Once improved assays are deployed in the field, an important question is: What can be done to ensure that the right answers are produced year after year? Proficiency testing is valuable for this purpose and typically involves sending spiked synthetic matrices to participating laboratories and determining whether these laboratories report similar results. Although this kind of testing helps ensure accuracy, the commutability of the material (ability to behave in the same ways as human samples across all platforms) becomes a concern. Proficiency-testing spiked samples does not always perform in the same way as human samples; their test results are difficult to compare among platforms and they give different results when used with different platforms. If minimally processed commutable human samples are used instead, proficiency testing improves. This, in turn, is likely to demonstrate that for some assays, particularly certain immunoassays, the outcomes are wrong. This is disheartening and raises the question of whether it is possible to achieve standardization. Perhaps feedback from standardization efforts and proficiency-testing programs using commutable materials (such as the Vitamin D Standardization Program) will spur manufacturers to examine, reformulate, and/or better calibrate their assays to improve their results.
PANEL DISCUSSION: WHAT DO THESE METHODOLOGY ISSUES MEAN FOR CLINICAL PRACTICE?
Dr. Coates served as panel moderator and began by explaining that the Office of Dietary Supplements initiated the Vitamin D Standardization Program mentioned by Dr. Hoofnagle. He stressed that it relies heavily on international collaborative efforts. The program's goal is to standardize the laboratory measurement of serum 25(OH)D to make the measurements accurate and comparable over time, location, and laboratory procedure.
Dr. Coates then asked the three panelists to make brief comments about the measurement of serum 25(OH)D concentrations. A general discussion with the audience followed.* Panelist: Ian S. Young, M.D. Queen's University Belfast *It seems as if vitamin D assays cannot be readily standardized because the different assays do not measure the same thing. In particular, immunoassays require fundamental reformulation to allow standardization, and that is unlikely to occur. Moreover, vitamin D experts do not agree on the fundamental parameters of the measurand.
However, it is possible to improve agreement, at least among the immunoassays. This could, however, result in a situation where the mean value on samples for assays would be the same, but for individual patient samples there would still be significant differences between them. This situation can only be addressed if all assays use liquid chromatography tandem mass spectroscopy (LC-MS/MS). Although this will likely occur eventually, it will not happen for years and will require advances in LC- MS/MS technology.
Panelist: John F. Aloia, M.D.
Winthrop University Hospital and Stony Brook University
Progress is being made in accurately measuring serum 25(OH)D concentration, but the inability to have confidence in the accuracy of the measures reported over time when assessing the relationships between serum concentrations and health outcomes is a concern. The studies used to generate recommendations and conclusions about vitamin D's benefits and harms are not reliable or are difficult to interpret because of questions about the accuracy of at least some of the assays used. Although little can be done to correct past research, awareness of the compromised condition of the data appears to be important.* Panelist: J. Sanford Schwartz, M.D. University of Pennsylvania *Any problem can be made more complicated, and this may be the situation for vitamin D. One of the more important underpinnings for clinical decision-making comes from a research team at the Tufts University School of Medicine that described a "threshold approach" [1]. According to this approach, the clinician's estimate of the probability that a patient has a particular disease is a principal factor in determining the next step. This step could be to withhold treatment, obtain more data by testing, or treat the patient without subjecting him or her to the risks of further diagnostic testing. For any disease or condition, clinicians should withhold treatment if the probability of disease is smaller than the testing threshold (i.e., the benefits do not exceed the risks). Conversely, clinicians should treat if the probability of disease is greater than the treatment threshold (i.e., the benefits outweigh the risks). Additional testing provides information that moves a patient above the treatment threshold or below the testing threshold. An important aspect of this model is that the thresholds are not fixed; they move in response to the benefits and harms of an intervention as well as the performance of the diagnostic test.
This conference has highlighted a failure in the first step of the hierarchy of evaluation of diagnostic technologies: the existing technical capacity to measure vitamin D is inadequate. Clinicians cannot be confident that the vitamin D test is performed reliably. What impact does the inaccuracy have on diagnosis, initiation of interventions, and ultimately on patient outcomes? From a clinical perspective, the issue must be patient-driven because clinicians treat patients, not numbers. What the practicing clinician needs to know is how to interpret the serum 25(OH)D measure in a way that is clinically meaningful.
My takeaway message from my observations of vitamin D is that a healthy person is a person who has not yet undergone enough tests. That different laboratories report different quantitative amounts of vitamin D for the same sample—and for which the results are different enough to support different decisions about interventions—reminds me of my experience with cholesterol testing. I allowed five different drug companies to test my cholesterol while attending a professional meeting.
The results differed enough that they resulted in different conclusions about whether treatment with statins was warranted according to the Adult Treatment Panel III guidelines. Such outcomes have helped change guidelines from focusing on use of a threshold for a measured number to consideration of the probability of risk.
I support shared decision-making. However, shared decision-making is an informed process, and I am uncertain of what to tell a patient about the benefits, harms, or risks of supplementation based on a test of a vitamin D serum sample.
Panel and Audience Discussion
Dr. Coates opened the discussion by underscoring Dr. Aloia's comment that what researchers believe about the relationship between vitamin D status and health outcomes as measured by serum 25(OH)D is based on a series of assays in which the field now has less confidence. Dr. Coates asked Dr. Hoofnagle what this means for the vitamin D field and, specifically, whether it is possible to correct the vitamin D concentration results in studies that have been completed.
Dr. Hoofnagle responded by referring to a roundtable discussion some time ago on adjusting National Health and Nutrition Examination Survey (NHANES) data to accommodate differences in the assays used over time. Statisticians on the roundtable devised a method to adjust and then compare at least the means of these data, which was encouraging. However, making similar adjustments for individuals as opposed to population groups is likely to be much more complicated. He underscored the importance of ensuring that LC-MS methodologies are the assay of choice because they are most likely to be accurate. However, LC-MS assays do have flaws, so they must be used with quality control measures, as with any assay.
Christopher Sempos of the Office of Dietary Supplements noted that one way to recalibrate existing data is to use a small subsample of previously measured and stored samples. This reference- measurement approach prevents the need to reanalyze all of the samples and, in particular, can yield reliable data for the lower part of the distribution of status measures.
Dr. Rosen asked Dr. Schwartz if it would be possible to act on one of the two thresholds (i.e., treatment or further diagnosis) that Dr. Schwartz mentioned if a gold standard for 25(OH)D measurement were available and accurate laboratory reports could be obtained. Dr. Schwartz responded that he would not be comfortable moving toward either of the two thresholds in the case of vitamin D. He added that although the first step is an accurate measurement, there is no consensus about the clinical meaning of the measure. He expressed some skepticism that there is a correlation between serum measures and physiologic health or pathophysiologic status, and he wondered whether cross-sectional measures are reliable. He joked that a cross-sectional study in South Florida, for example, could result in a conclusion that everyone is born Hispanic and dies Jewish.
Dr. Schwartz commented that there is considerable value in the type of dialogue characterizing this conference in that it has brought together "three legs of a stool" that have not interacted as effectively as they might have. The opportunity for people with different areas of vitamin D expertise and perspectives—laboratory and measurement skills, scientific research expertise, and clinical application experience—to communicate directly with each other make a worthwhile contribution. The important task now is to identify the key measures needed relative to vitamin D and how to interpret them.
Dr. Bouillon said that he was comforted by the observation that up-to-date LC-MS methodology supports the conclusion that administering 800 IU/day vitamin D maintains a serum 25(OH)D concentration above 20 ng/mL in 97% of the population. Dr. Hoofnagle noted that the 20 ng/mL cut- point comes from data from the use of assays that were not LC-MS based. He agreed that one could administer 800 IU/day vitamin D and maintain 20 ng/mL concentrations, but the 20 ng/mL cut-point is likely based on assays with inaccuracy rates of 15% or more. He suggested that the 20 ng/mL cut-point is rather arbitrary.
Michael McCaskill from Tulane University remarked that requiring all laboratories to use LC- MS/MS disadvantages small laboratories that lack access to these advanced techniques. His own laboratory is moving away from immunoassays and toward LC-MS, but it will be a long and expensive process. He suggested establishing a range for desirable serum 25(OH)D concentrations as a solution to the lack of accuracy of the 20 ng/mL cut-point.
Dr. Dawson-Hughes commented that it is extremely important to analyze samples using MS and to determine carefully the total amount of vitamin D ingested. She underscored the importance of specifically measuring the amount of vitamin D in the supplement to be used. The amount can vary considerably even when a clinician orders a specific supplement. Ensuring the accuracy of the intake and the serum measure is a critical step in correctly interpreting clinical trial data. Dr. Schwartz added that the conditions under which a supplement is administered (such as on an empty stomach) can also affect the total exposure to the nutrient. Overall, it is important to consider research protocol details, such as how specimens were drawn and handled as well as how the supplements were administered.
Rachel Ballard of the National Cancer Institute asked for comments—for the purposes of context and because of the variability associated with many clinical issues—on areas of medicine that are similar to vitamin D. Dr. Schwartz responded that he could not give a good answer at the moment, but he would think about it and hoped that others might consider this question in upcoming discussions.
References
[1] Paulker SG, Kassirer JP. The threshold approach to clinical decision making. N Engl J Med. 1980:302(20): 1109-17.!!!Session 6: What Can We Say About
Translating Evidence into Clinical Practice and the
Related Research Gaps?
Three panel members commented on the highlights of this conference and identified key next steps based on the presentations and discussions. This was followed by an audience-wide discussion of information gaps and special considerations.* Panelist: Bess Dawson-Hughes, M.D. Tufts University *The wealth of information presented at this conference is challenging to summarize. I will highlight a few areas that struck me as particularly interesting.
First, available clinical trials are a gold standard, but they have acknowledged limitations (e.g., specification of dosage, measuring compliance, and sufficient duration). Furthermore, investigators should consider the likelihood that trials will be complicated when the effects of the chronic disease occur during certain latency periods.
Second, measurement issues are very important. Researchers should determine the role of free (i.e., bioavailable) serum 25(OH)D, especially in the context of race and ethnicity questions pertaining to vitamin D status. Better serum 25(OH)D assays with sufficient standardization are required, and mass spectroscopy (MS) methodologies certainly show promise. Also, researchers should explore how the vitamin D-binding protein (DBP) genotypes influence the vitamin D-binding affinities. Moreover, potentially influential factors, such as inflammation, lead to many unanswered questions.
Third, with regard to shared decision-making, I—like Dr. Schwartz—am happy to share information with patients but what information should we share? What clinicians could tell patients about the relationship between vitamin D and certain diseases is unclear. Furthermore, clinicians do not know what to expect from vitamin D supplementation, which appears to have created an expensive and excessive culture of measurement and treatment.
Finally, the vitamin D field is in what might be considered a meta-analysis "war zone" in the sense that these reviews are at war with each other about the right answer. In addition, it is difficult to obtain study-level data to quantify and analyze important individual factors. In the near future, individual-level data from large trials will be available to researchers. Such data will be a powerful tool and can provide many opportunities to obtain a more informed and refined understanding of the contributions of these many factors to conclusions about the relationship between vitamin D and disease.* Panelist: Victor M. Montori, M.D. Mayo Clinic *I offer six summary points. First, the field needs clarity about whether a significant public health problem exists. Cited estimates suggest that 30%, 40%, or 50% of the U.S. population has vitamin D deficiency—or perhaps not. We have also heard at this conference that vitamin D deficiency has an impact on quality of life and mortality—or perhaps not.
Second, endocrinologists and primary care clinicians use reference ranges for vitamin D serum measures that come from various, and sometimes unknown, sources or from conferences they attend. These reference ranges determine whether a patient has deficiency and whether to treat deficiency with supplements on that basis. Such activities convey the impression that clarity exists about vitamin D deficiency rather than confusion. The result is an "epidemic" of over-testing and over-treatment.
Third, the following formula for calculating return-on-investment (ROI) is potentially helpful: ROI = estimated efficacy x knowledge transfer. The ROI in this case is the realization of the overall impact, which has two components. The first component, estimated efficacy, is unclear for most of the indications for which vitamin D is used. The second component, knowledge transfer, relates to the clinician's ability to identify the right patient for treatment and that patient's adherence to the treatment over time. Again, there is uncertainty. Thus, uncertainty is associated with the impact of both the science that has been conducted and the practices that have been promoted.
Fourth, managing the concerns about vitamin D as a clinical problem has led to disconnects. This conference has shown that the main reason why primary care providers administer vitamin D is to treat depression. This practice has "gone viral," leading to questions about who is feeding the idea and how it became viral. Moreover, clinicians on the front lines are using vitamin D to treat nonspecific pain and depression, whereas research experts are exploring the effects of vitamin D supplements on such conditions as cancer, other chronic diseases, calcium abnormalities, and parathyroid-hormone changes. Communication between researchers and clinicians is flawed, and they are focusing on different things. The use of vitamin D to treat depression or relieve pain should be addressed either by better education for clinicians or by trials that assess the vitamin's effectiveness for this purpose.
Fifth, managing the concerns about vitamin D as a public-health problem is an option and can be inspired by the experience managing obesity. Rather than trying to produce changes in individual patients on a case-by-case basis, it is better to address the environmental and societal components that surround the health problem. If vitamin D insufficiency is a real problem, people should collectively consider how they choose to live, work, and feed themselves. In other words, policies must be implemented that will prevent or resolve the problem instead of a clinical approach that focuses on one patient at a time. However, the suggested approach requires a great deal of effort and commitment. Before expending these resources, it is best to decide whether a problem exists.
Sixth and finally, if researchers ultimately decide that a clinical problem is present and must be addressed, do healthcare providers have time and effort to dedicate to shared decision-making with patients when the field appears to offer such limited information? In the absence of a clear message, values become an important aspect of shared decision-making. If conversations about vitamin D happen, those involved need to admit their ignorance and uncertainty. Furthermore, the conversations will have a cost in the form of patient-doctor interaction opportunities because clinicians could instead spend time and resources meeting other health needs or even offering psychotherapy that could more effectively manage mild to moderate depression.* Panelist: Michael L. LeFevre, M.D., M.S.P.H. University of Missouri *I am now speaking as a practicing clinician, not as chair of the U.S. Preventive Services Task Force. Let me first express my agreement with Dr. Montori's summary comments. And then I would like to go on to note that, despite the many presentations and discussions during this conference, I do not feel better about the state of vitamin D. I liken this feeling to the reaction of the girl in the movie The Sound of Music whose slightly injured finger is bandaged after the heart-breaking departure of Maria but asks, "Why don't I feel better?"
How many of you in the audience take a vitamin D supplements? How many are taking a statin? (Many more indicated that they used a vitamin D supplement than a statin.) Given the apparent senior- level ages of this audience, this result is noteworthy. More people are using a substance for which no clinical-trial data show clear benefits than are using a substance that has proven benefits for their age group. What is going on here?
I suggest that primary-care physicians ask themselves three questions about vitamin D before they see a patient:
Do I broach the topic of vitamin D screening or supplementation in the relatively small window of time I have to address preventive services with my patient?
If a patient asks about the appropriateness of screening and supplementation, what can I say?
When a patient presents with nonspecific symptoms (e.g., fatigue, weakness, pain with no specific pathology, or a clinical picture of depression or fibromyalgia), is there a role for screening and then treatment with vitamin D to make the patient feel better?
Discussions during this conference have suggested that 4-5% of all primary-care encounters result in vitamin D screening. This shows that primary-care providers have concluded that vitamin D "cures everything" (I am exaggerating for effect!) and that administering vitamin D takes care of many patients who have never found anything before to take care of their problems. Why should providers not check patients' vitamin D levels and give them vitamin D supplements? Well, decisions to act are best informed by randomized controlled trials, despite the limitations of these trials. Association is not enough. Furthermore, given my limited time and capacity to engage in shared decision-making with patients, I would choose to talk with my patients about statins, for example, before discussing vitamin D.
I argue against recommending that the public talk to their doctor about vitamin D. Clinicians are not well informed about the topic, and therefore the most honest message to convey during shared decision-making about vitamin D is, "I don't know." Patients can be told what clinicians know about vitamin D and health, but they need to understand that clinicians are not certain about the optimal blood level for health.
Finally, I offer an analogy to blood pressure studies. There is a strong association between blood pressure and cardiovascular outcomes in that as blood pressure increases, the risk of cardiovascular problems increases. However, the key question is whether cardiovascular risk is reduced if a person with a particular blood pressure is treated and the pressure is reduced. Likewise, for vitamin D, the field needs more studies to be certain that changes in serum levels will have benefits. For example, what are the effects of a serum 25(OH)D concentration of 40 ng/mL versus 20 ng/mL?
Clinicians have been addressing vitamin D using a cholesterol model rather than a blood pressure model. In the cholesterol model, people who meet certain eligibility criteria are given a fixed dose of medicine and are studied to find out whether their condition improves. During this conference, application of this type of model to vitamin D has been criticized, largely because the wrong dose has been used for vitamin D studies. Perhaps a blood pressure model is more appropriate. In this model,
clinicians treat low serum levels to achieve a target concentration and then monitor outcomes.
However, until foundational studies are conducted, clinicians are left with "I don't know" as the answer to patients' questions about vitamin D.** Panel and Audience Discussion__
Dr. Rosen, the panel moderator, opened the discussion by addressing a question from an online attendee to Dr. Dawson-Hughes about interactions between vitamin D and magnesium or vitamin K. Dr. Dawson-Hughes responded that fat-soluble vitamins, such as vitamin K, presumably have similar absorption mechanisms, but she was not aware of any competitive binding among these nutrients.
Another online attendee asked Dr. Hoofnagle whether vitamin D assays use serum or plasma.
Dr. Hoofnagle responded that the answer depends on the assay. High performance liquid chromatography-mass spectrometry (HPLC-MS), which relies on heptane or hexane, generates the same results for serum and plasma. Dr. Dawson-Hughes added that, to her knowledge, whether plasma or serum is measured by DiaSorin radioimmunoassay makes no difference.
Dr. Schwartz commented that a standard, precise, unbiased, and clinically meaningful measure of vitamin D status is needed. The first step should be epidemiological studies followed by randomized clinical trials. Furthermore, the distinction between relative risk and absolute risk is often overlooked. Even effective treatments have less incremental benefit or net benefit when they are administered in a population with a lower absolute risk than one with a higher absolute risk.
Dr. Schwartz added that, assuming that appropriate assays are developed and a National Health and Nutrition Examination Survey (NHANES) data reanalysis serves as the epidemiological foundation, an interesting question is: What areas of vitamin D research should clinical trials address? Dr. Rosen responded that a new trial on falls (Study to Understand Fall Reduction and Vitamin D in You) funded by the National Institute on Aging should provide answers about whether vitamin D reduces the risk of falls in persons aged 70 years and older at high risk of falling and about dose-response relationships. Dr. Dawson-Hughes highlighted the Vitamin D and Type 2 Diabetes (D2d) study funded by the National Institutes of Health (NIH) that is designed to examine the effect of vitamin D in adults with pre-diabetes. The study uses only one dose (4,000 IU) of vitamin D, so additional studies are needed to examine effects of lower doses. In addition, the Vitamin D and Omega-3 Trial funded by NIH is assessing the effects of both vitamin D and omega-3 fatty acids on cancer and cardiovascular disease. Dr. Montori advocated for studies on the effect of vitamin D on unexplained medical syndromes, including depression.
Dr. Young asked panel members whether they would prescribe a vitamin D supplement for a patient with a serum 25(OH)D concentration of 12 ng/mL. Drs. Rosen and Dawson-Hughes said that they would prescribe a supplement. Dr. LeFevre said he would also prescribe a supplement but added that this question is different than the question of whether to screen a patient in the first place. He noted that very few primary-care physicians are aware of the measurement controversies. Rather, they believe the laboratory report, and the only question they ask themselves is what the serum concentration should be. Dr. Rosen added that he agreed that practicing clinicians take the laboratory reports at face value. He believed that explaining the problems with vitamin D measurements to primary-care physicians would be a new variable for them and would increase their uncertainty regarding clinical approaches to vitamin D.
Federal Co-sponsors
NIH: National Cancer Institute (NCI)
NIH: National Center for Complementary and Alternative Medicine (NCCAM)
Now known as the National Center for Complementary and Integrative Health (NCCIH).
NIH: National Institute of Arthritis and Musculoskeletal Skin Diseases (NIAMS)
NIH: National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
NIH: National Institute on Aging (NIA)
Agency for Healthcare Research and Quality (AHRQ)
Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention (CDC)
Food and Drug Administration (FDA)
National Institute of Standards and Technology (NIST), U.S. Department of Commerce
Office of Disease Prevention and Health Promotion (ODPHP), U.S. Department of Health and Human Services!!!Agenda
Day 1 — Tuesday, December 2
8:00 a.m.
Welcome and Rationale for Conference
Conference Chair: Clifford Rosen, M.D. — Maine Medical Center Research Institute
Session 1: The Challenges—How Do We Evaluate and Apply Evidence for Primary Care Decision Making?
8:10 a.m.
Principles for Evaluating Evidence
Barry S. Kramer, M.D., M.P.H. — National Cancer Institute (NCI), National Institutes of Health (NIH)
8:40 a.m.
Translating Evidence into Guidelines
Victor M. Montori, M.D. — Mayo Clinic
9:10 a.m.
Revised Criteria for National Guidelines Clearinghouse
Mary Nix, M.S. — Agency for Healthcare Research and Quality
9:45 a.m.
Development of Endocrine Society Guidelines
Michael F. Holick, M.D., Ph.D. — Boston University School of Medicine
10:15 a.m.
Applying Systematic Reviews to Dietary Reference Intakes: Vitamin D as a Case Study
Patsy M. Brannon, Ph.D., M.S. — Cornell University
10:45 a.m.
U.S. Preventive Services Task Force: Screening for Vitamin D Deficiency
Michael L. LeFevre, M.D., M.S.P.H. — University of Missouri
11:15 a.m.
Panel: Perspectives on Evaluating Evidence in Primary Care Context
Moderator: Paul M. Coates, Ph.D. — Office of Dietary Supplements (ODS), NIH
Robert P. Heaney, M.D. — Creighton University
Gordon Guyatt, M.D., M.Sc., F.R.C.P.C., O.C. — McMaster University
Edward L. Giovannucci, M.D., Sc.D. — Harvard School of Public Health
Roger Bouillon, M.D., Ph.D., F.R.C.P. — KU Leuven, Belgium
Open Discussion: Panel and Audience
Session 2: What is the View from the Front Lines?
1:30 P.M.
The Vitamin D Landscape
Clifford Rosen, M.D. — Maine Medical Center Research Institute
1:45 P.M.
Panel: What Is the Vitamin D Experience?
Moderator: Clifford Rosen, M.D. — Maine Medical Center Research Institute
Ravi I. Thadhani, M.D., M.P.H. — Harvard University and Massachusetts
General Hospital
Peter S. Millard, M.D., Ph.D. — Seaport Community Health Center
Sylvia B. Rowe, M.A. — SR Strategy, LLC.
Open Discussion: Panel and Audience
Session 3: The Uncertainties—How Do We Think About Risk of Nutritional Inadequacy?
2:15 P.M.
Requirement Distributions and Clinical Practice
Alicia L. Carriquiry, Ph.D., M.Sc. — Iowa State University
3:00 P.M.
Groups at Risk: Is Lower Serum 25(OH)D Always a Concern?
Bonny Specker, Ph.D. — South Dakota State University
3:30 p.m.
African American Case Study: Serum 25(OH)D and Bone Health
John F. Aloia, M.D. — Winthrop University Hospital and SUNY Stony Brook
4:00 P.M.
African American Case Studies: Genetic Variants
Perspective 1
Ravi I. Thadhani, M.D., M.P.H. — Harvard University and Massachusetts General Hospital
Perspective 2
Roger Bouillon, M.D., Ph.D., F.R.C.P. — KU Leuven, Belgium
Open Discussion: Panel and Audience
Day 2 — Wednesday, December 3
Session 4: The Uncertainties—What Do We Know About Vitamin D Intake and Supplement Use?
8:00 a.m.
Current Exposure to Vitamin D: Food, Food Fortification, and Supplements
Valerie Tarasuk, Ph.D. — University of Toronto
8:30 a.m.
Changes in Serum 25(OH)D Concentrations with Amount and Nature of Intake
Sue A. Shapses, Ph.D., R.D. — Rutgers University
9:00 a.m.
Possible Adverse Consequences of Higher Vitamin D Status: Emerging Evidence from observational studies
Demetrius Albanes, M.D. — NCI, NIH
9:30 a.m.
Sessions 3 and 4 Joint Panel Discussion: Balancing Risk and Intervention
Moderator: Susan T. Mayne, Ph.D. — Yale School of Public Health
Valerie Tarasuk, Ph.D. — University of Toronto
Sue A. Shapses, Ph.D., R.D. — Rutgers University
Demetrius Albanes, M.D. — NCI, NIH
Bonny Specker, Ph.D. — South Dakota State University
John F. Aloia, M.D. — Winthrop University Hospital and SUNY Stony Brook
Ravi I. Thadhani, M.D., M.P.H. — Harvard University and Massachusetts
General Hospital
Roger Bouillon, M.D., Ph.D., F.R.C.P. — KU Leuven, Belgium
Open Discussion: Panel and Audience
Session 5: The Uncertainties—What are Issues Surrounding Laboratory Measurement of Serum 25(OH)D?
10:15 a.m. Measurement of 25(OH)D: Perspective from the Clinical Laboratory
10:45 a.m.
Andrew Hoofnagle, M.D., Ph.D. — University of Washington
Panel: What Do These Methodology Issues Mean for Clinical Practice?
Moderator: Paul M. Coates, Ph.D. — ODS, NIH
J. Sanford Schwartz, M.D. — Wharton University of Pennsylvania
John F. Aloia, M.D. — Winthrop University Hospital and SUNY Stony Brook
Ian S. Young, Ph.D. — Queen's University Belfast and Centre for Public
Health
Open Discussion: Panel and Audience
Session 6: What Can We Say About Translating Evidence into Clinical Practice and the Related Research Needs?
11:15 a.m. Panel Discussion: What Did We Hear and What Are the Next Steps?
Moderator: Clifford Rosen, M.D. — Maine Medical Center Research Institute
Bess Dawson-Hughes, M.D. — Tufts University
Victor M. Montori, M.D. — Mayo Clinic
Michael L. LeFevre, M.D., M.S.P.H. — University of Missouri
Open Discussion: Panel and Audience 12:00 noon Closing Comments and Adjourn
