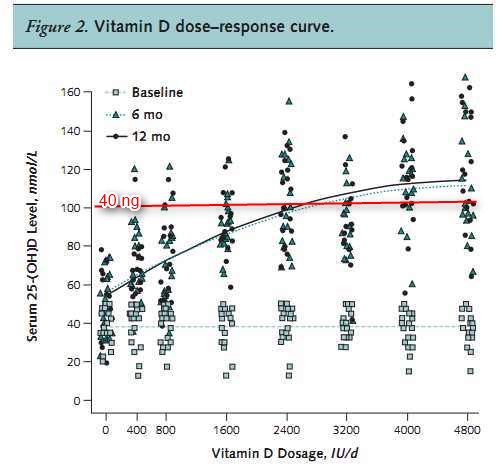
Vitamin D response: 800 IU: 20 ng, 3200 IU: 45 ng – RCT
Dose response to vitamin d supplementation in postmenopausal women: a randomized trial.
Ann Intern Med. 2012 Mar 20;156(6):425-37.
Gallagher JC jcg@creighton.edu, Sai A, Templin T 2nd, Smith L.
Bone Metabolism Unit, Creighton University School of Medicine, and College of Public Health, University of Nebraska Medical Center, Omaha, Nebraska.
Background: Serum 25-hydroxyvitamin D (25-[OH]D) is considered the best biomarker of clinical vitamin D status.
Objective: To determine the effect of increasing oral doses of vitamin D(3) on serum 25-(OH)D and serum parathyroid hormone (PTH) levels in postmenopausal white women with vitamin D insufficiency (defined as a 25-[OH]D level ?50 nmol/L) in the presence of adequate calcium intake. These results can be used as a guide to estimate the Recommended Dietary Allowance (RDA) (defined as meeting the needs of 97.5% of the population) for vitamin D(3).
Design: Randomized, placebo-controlled trial. (ClinicalTrials.gov registration number: NCT00472823)
Setting: Creighton University Medical Center, Omaha, Nebraska.
Participants: 163 healthy postmenopausal white women with vitamin D insufficiency enrolled in the winter or spring of 2007 to 2008 and followed for 1 year .
Intervention: Participants were randomly assigned to receive placebo or vitamin D(3),
- 400, 800, 1600, 2400, 3200, 4000, or 4800 IU once daily.
Daily calcium supplements were provided to increase the total daily calcium intake to 1200 to 1400 mg.
Measurements: The primary outcomes were 25-(OH)D and PTH levels at 6 and 12 months.
Results: The mean baseline 25-(OH)D level was 39 nmol/L.
The dose response was curvilinear and tended to plateau at approximately 112 nmol/L in patients receiving more than 3200 IU/d of vitamin D(3).
The RDA of vitamin D(3) to achieve a 25-(OH)D level greater than 50 nmol/L was 800 IU/d.
A mixed-effects model predicted that 600 IU of vitamin D(3) daily could also meet this goal.
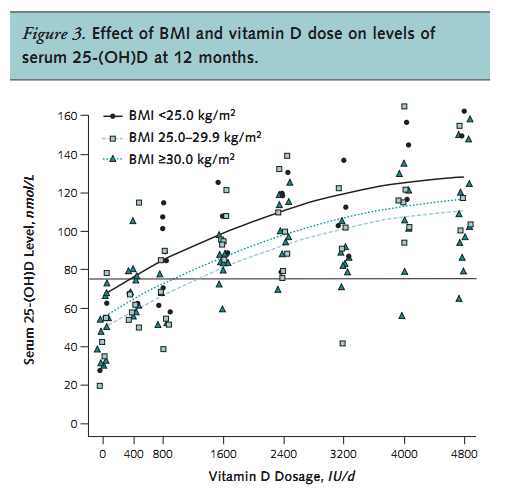
Compared with participants with a normal body mass index (<25 kg/m(2)), obese women (?30 kg/m(2)) had a 25-(OH)D level that was 17.8 nmol/L lower.
Parathyroid hormone levels at 12 months decreased with an increasing dose of vitamin D(3) (P = 0.012).
Depending on the criteria used,
hypercalcemia occurred in 2.8% to 9.0% and
hypercalciuria in 12.0% to 33.0% of participants;
- events were unrelated to dose.
Limitation: Findings may not be generalizable to other age groups or persons with substantial comorbid conditions.
Conclusion: A vitamin D(3) dosage of 800 IU/d increased serum 25-(OH)D levels to greater than 50 nmol/L in 97.5% of women; however, a model predicted the same response with a vitamin D(3) dosage of 600 IU/d.
These results can be used as a guide for the RDA of vitamin D(3), but prospective trials are needed to confirm the clinical significance of these results.
Obese had less response to the same vitamin D dose (perhaps just due to extra weight)
Primary Funding Source: National Institute on Aging.
PMID: 22431675
PDF of study is attached at bottom of this page
See also VitaminDWiki
All items in category How Much Vitamin D 257 items as of Jan 2024
Overview Vitamin D Dose-Response
- 14,000 IU to get 50 ng, lots of graphs
Must balance co-factors when increasing vitamin D which has the following graphs
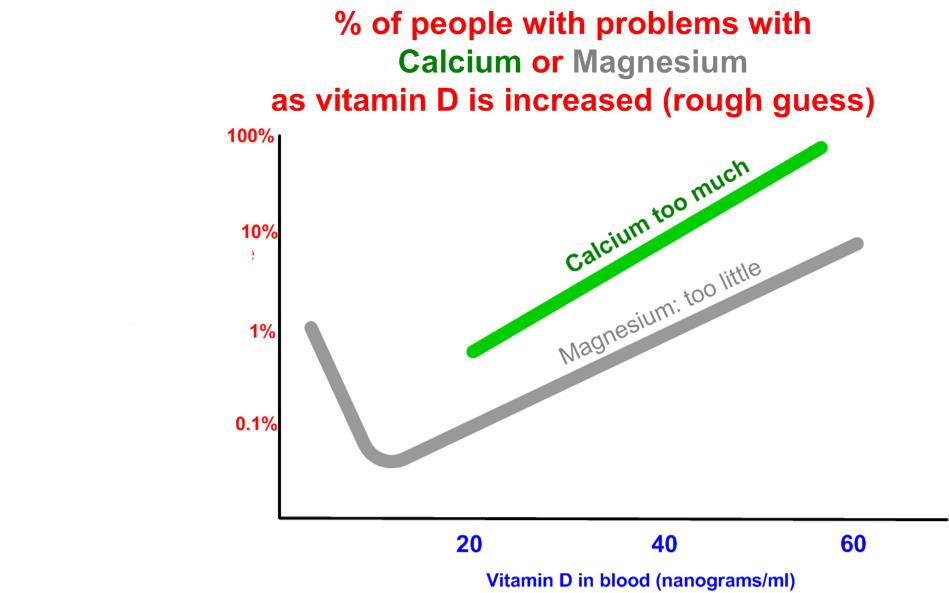
The amount of Calcium intake in this study (1200 to 1400 mg) was borderline or in the dangerous region reported by previous studies
Additional reasons that they did not seem to consider for having low response to vitamin D CLICK HERE for entire list
Soft drink cola - uses up Calcium which uses up vitamin D
Some drugs consume or block vitamin D
Antiseizure, Prednisone, AIDS drugs, Orlistat, Questran, Dilatin, Phenobarbital, Rifampin, Steroids, Calcium channel blockers
Cholestyramine, Mineral Oil, , St Johns wort
Use of polyunsaturated fats decreased bio-availablity of vitamin D
Less Magnesium in foods - Magnesium is needed to utilize vitamin D (as well as build bones)
Undergoing Chemotherapy
Have MS prevented AND treated by vitamin D, a mountain of evidence
Had a condition which Prevents Adsorption in the gut
Colon Cancer more than 10 years before
IBD UC and CD at risk of being vitamin D deficient
Have +Gluten Intolerance
Have Celiac Disease
Have HIV both prevents conversion and consumes vitamin D
Have a condition which requires more vitamin D - or time in the sun
Surgery and trauma within the past year
