Infant HIV, Malaria, and high vitamin D
Vitamin D Status Is Associated with Mortality, Morbidity, and Growth Failure among a Prospective Cohort of HIV-Infected and HIV-Exposed Tanzanian Infants.
J Nutr. 2015 Jan;145(1):121-7. doi: 10.3945/jn.114.201566. Epub 2014 Nov 12.
Sudfeld CR 1 csudfeld@hsph.harvard.edu , Duggan C2, Aboud S3, Kupka R4, Manji KP5, Kisenge R5, Fawzi WW6.
 See also VitaminDWiki
* Malaria in mice brains, and associated inflammation, prevented by Vitamin D intervention – July 2014
* Overview HIV and vitamin D
* Severe malaria 9 percent less likely with each extra 1 nanogram of vitamin D – 2014
* Search VitaminDWiki for MALARIA 486 items as of July 2020
* Vitamin D and malaria – many studies
* Is too much vitamin D bad – possible causes and cures
See also Web
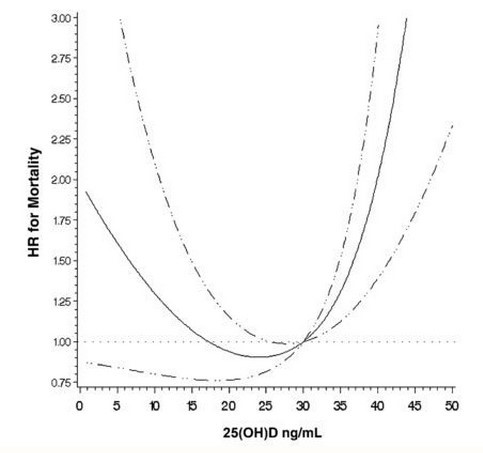
* New study suggests U-shaped curve for vitamin D and risk of mortality among infants with HIV
* Vitamin D Council Jan 2015 – behind a paywall
* Vitamin D Insufficiency Is Common in Ugandan Children and Is Associated with Severe Malaria
* PLOS Dec 2014 full text online
* Vitamin D status: Association with iron therapy effectiveness and risk of malaria infection
* Children with malaria need more Iron to use Vitamin D effectively
See also VitaminDWiki
* Malaria in mice brains, and associated inflammation, prevented by Vitamin D intervention – July 2014
* Overview HIV and vitamin D
* Severe malaria 9 percent less likely with each extra 1 nanogram of vitamin D – 2014
* Search VitaminDWiki for MALARIA 486 items as of July 2020
* Vitamin D and malaria – many studies
* Is too much vitamin D bad – possible causes and cures
See also Web
* New study suggests U-shaped curve for vitamin D and risk of mortality among infants with HIV
* Vitamin D Council Jan 2015 – behind a paywall
* Vitamin D Insufficiency Is Common in Ugandan Children and Is Associated with Severe Malaria
* PLOS Dec 2014 full text online
* Vitamin D status: Association with iron therapy effectiveness and risk of malaria infection
* Children with malaria need more Iron to use Vitamin D effectively
BACKGROUND:
Vitamin D is a potent immunomodulator, but its impact on morbidity and mortality among infants remains unclear.
OBJECTIVE:
The objective of the study was to prospectively assess the association of vitamin D status with mortality, morbidity, and growth during the first 2 y of life.
METHODS:
A prospective cohort of 253 HIV-infected and 948 HIV-exposed Tanzanian infants enrolled in a randomized trial of multivitamins (not including vitamin D) was studied. Serum 25-hydroxyvitamin D [25(OH)D] concentrations were measured at 5-7 wk of age and infants were followed at monthly clinic visits until 24 mo. Physicians performed a clinical exam every 3 mo or when an illness was noted.
RESULTS:
Serum 25(OH)D concentrations were (means ± SDs) 18.6 ± 10.3 ng/mL and 18.1 ± 9.2 ng/mL for HIV-infected and HIV-exposed infants, respectively. Unexpectedly, serum 25(OH)D concentrations ≥30 ng/mL were significantly associated with higher mortality as compared to the 20-29.9 ng/mL reference for HIV-infected (HR: 2.47; 95% CI: 1.13, 5.44; P = 0.02) and HIV-exposed (HR: 4.00; 95% CI: 1.67, 9.58; P < 0.01) infants after multivariate adjustment. We found no statistically significant association between 25(OH)D concentrations <10 ng/mL and mortality for HIV-infected (HR: 1.43; 95% CI: 0.74, 2.78; P = 0.29) and HIV-exposed (HR: 1.56; 95% CI: 0.60, 4.03; P = 0.36) infants. Among HIV-exposed infants, 25(OH)D concentrations ≥30 ng/mL were significantly associated with clinical [incidence ratio rate (IRR): 1.34; 95% CI: 1.06,1.70; P = 0.02] and confirmed (IRR: 1.71; 95% CI: 1.71; 1.15, 2.54; P < 0.01) malaria diagnoses, whereas concentrations of <10 ng/mL were associated with oral candidiasis (IRR: 1.47; 95% CI: 1.00-2.15; P = 0.046) and wasting (HR: 1.71; 95% CI: 1.20, 2.43; P < 0.01).
CONCLUSION:
The observational design of this study does not allow for causal interpretation; however, the results indicate a strong need for additional studies of vitamin D among HIV-infected and -exposed children, particularly in malaria-endemic settings. The parent trial was registered at clinicaltrials.gov as NCT00197730.
© 2015 American Society for Nutrition.
PMID: 25527666