Major review of Vitamin D – Holick 2013 part II
This is the second part of Major review of Vitamin D – Holick Feb 2013
TABLE 6.
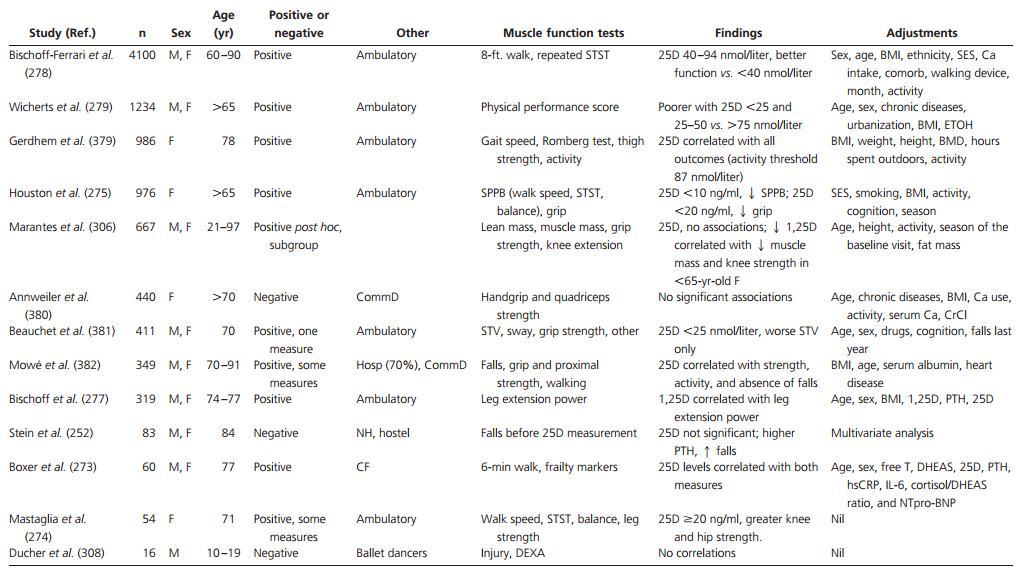
Cross-sectional studies assessing the correlation between vitamin D levels and muscle function (listed in order of number of study participants, highest to lowest)
Age Positive or CF, Cardiac failure (ejection fraction <40%); CommD, community dwelling; comorb, comorbid conditions; CrCl, creatinine clearance; DHEAS, dehydroepiandrosterone sulfate; ETOH, alcohol use; free T, percent free testosterone; Hosp, recently hospitalized; hsCRP, high-sensitivity C-reactive protein; NH, nursing home; NT-proBNP, N-terminal pro-brain natritretic peptide; SES, socioeconomic status; SPPB, short physical performance battery; STV, stride time variability.
in the Arabic women. Baseline 25D levels were independently associated with maximal voluntary knee extension. After vitamin D repletion, the Arabic women displayed significant improvements in parameters of muscle function at 3 and 6 months. At 6 months, a subgroup that was retested showed no difference in electrically stimulated muscle function vs. Danish controls. Subjective improvements in muscle and deep bone pain were reported by the treated Arabic women.
3. Randomized controlled studies
The randomized controlled studies are summarized in Table 7. Two studies discussed in Section VI.E and Table 6 [Bischoff et al. (259) and Pfeifer et al. (258)] reported improvements in muscle function as well as decreased falls in those randomized to receive supplemental vitamin D. Over a 12-wk treatment period, those on calcium and vitamin D demonstrated significant improvements in the summed score of knee flexor and extensor strength, grip strength, and TUAG compared with those receiving calcium alone (259). Significant improvements were reported in quadriceps strength and TUAG in another study with reduced falls after 12 months of dual supplements compared with calcium alone (258).
A two by two randomized study of patients treated with calcium 800 mg with or without resistance training, with or without vitamin D 400 IU daily for 9 months found that vitamin D improved physical performance (283). Quadriceps strength, physical performance test, and TUAG were significantly improved by vitamin D and by resistance training, with an additive benefit in the group that received both (283).
In a study of 139 ambulatory older subjects with a history of falls and vitamin D deficiency [25D <12 ng/ml (30 nmol/liter)], treatment with vitamin D2 (600,000 IU im) had a significant effect on aggregate functional performance time but no effect on either falls or quadriceps strength at 6 months follow-up vs. placebo (284).
Among 56 institutionalized persons over 60 yr of age, those randomized to receive calcium and vitamin D (two doses of 150,000 IU then 90,000 IU monthly) demonstrated significant improvements in maximal isometric strength of hip flexors and knee extensors after 6 months (285). Subgroup analysis demonstrated greater improvements in muscle function among subjects with lower baseline 25D levels [<20 ng/ml (50 nmol/liter)].
Similarly, among 302 older, community-dwelling women, those in the lowest tertile of 25D levels who received daily calcium (1000 mg) and vitamin D2 (1000 IU) displayed the most pronounced improvements in lower limb muscle function over 1 yr as opposed to those on calcium alone (286).
Among 69 postmenarcheal adolescent females, those randomized to receive 150,000 IU vitamin D2 orally every 3 months for 1 yr demonstrated significant improvements in movement efficiency, a composite of jump height and velocity measured by mechanography, compared with baseline (287). Additionally, at baseline, higher 25D levels correlated with greater jumping velocity.
In a short study of 42 postmenopausal women, 12 wk treatment with 1a-OHD3 (0.5 jug) and calcium led to significant improvements in quadriceps strength compared with those receiving calcium alone (288).
4. Muscle strength and function: negative studies
In a study of 70 vitamin D-deficient women [25D = 8-20 ng/ml (20-50 nmol/liter)], 6 months of vitamin D and calcium (400 IU and 500 mg) had no effect on grip or knee strength vs. calcium alone. Baseline 25D levels showed an inverse correlation with these parameters of muscle function (289).
In a study of 686 community-dwelling women over 70 yr, treatment with oral vitamin D3 (150,000 IU every 3 months) for a 9-month period had no significant effect on falls or hand grip strength compared with placebo (290). However, a randomly selected subgroup of 40 participants had a mean baseline 25D of 26 ng/ml (66 nmol/liter), suggesting that the group at large were vitamin D sufficient.
Other studies have failed to demonstrate improvements in muscle strength after vitamin D supplementation, regardless of baseline vitamin D status (291-295), as summarized in Table 7. A multicenter study of 243 frail, older patients reported no difference in parameters of physical performance between those randomized to receive a single dose of 300,000 IU of vitamin D vs. placebo (291). There was no effect in the subset with low baseline 25D levels [< 12 ng/ml (30 nmol/liter)] despite significant improvements in 25D levels. Some studies have examined other forms of vitamin D, namely 1,25D and 1a-OHD3, with variable effects. Among 98 older subjects with mild renal impairment, 1,25D (0.5 jug daily) resulted in no improvement over a 6-month period vs. placebo, and some subjects on 1,25D developed hypercalci-uria and required dose reduction (294).
One negative study examined 179 vitamin D-deficient adolescent females in Lebanon. Those randomized to receive vitamin D3 (doses of 1,400 or 14,000 IU/wk) did not demonstrate improved grip strength but did have greater increases in lean mass, bone area, and total hip bone mineral content vs. placebo after 1 yr (295).
Two studies have examined the effects of combining vitamin D supplementation with high-resistance training on muscle strength in older individuals (283, 293). In one study of 180 community-dwelling males (50-79 yr), those randomized to receive an intensive program of resistance training three times per week demonstrated improvements in strength. Those randomized to receive fortified milk alone (containing vitamin D 800 IU, calcium 1000 mg, and protein 13.2gdaily) demonstrated no additional improvements (293). Those receiving high-resistance training with vitamin D (400 IU) and calcium (800 mg) over a 9-month period showed improvements in TUAG but not in quadriceps strength compared with those who received resistance training and calcium (283).
5. Meta-analyses of muscle function
In one meta-analysis, the substantial variability in the parameters of muscle function among studies, use of measures without established validity or reliability, and lack of blinded outcome assessments were cited as reasons for inability to pool data (30).
On assessing 17 RCT involving 5072 participants, there was no significant effect of vitamin D supplementation on grip strength or proximal lower limb strength in adults with 25D levels over 10 ng/ml (25 nmol/liter) at baseline (24). However, for adults with deficiency [25D < 10 ng/ml (25 nmol/liter)], a beneficial effect on hip muscle strength was found.
In another meta-analysis of 16 RCT, in which baseline 25D levels were below 20 ng/ml (50 nmol/liter) in 11 studies, the authors noted the publication of a greater number of studies that showed no effect rather than a beneficial effect of vitamin D supplementation on muscle function and that there were no obvious characteristics to differentiate studies with positive and negative findings (296).
In a more recent meta-analysis of 13 RCT involving elderly subjects who were predominantly vitamin D deficient or insufficient, vitamin D supplementation with 800-1000 IU daily was associated with improvements in lower extremity strength and balance (297). The meta-analysis included only randomized trials of older individuals in whom baseline and posttreatment parameters of muscle function were assessed. Trials in younger individuals (295) or those that included muscle training as part of the treatment were not included (293). This meta-analysis found no effect on gait.
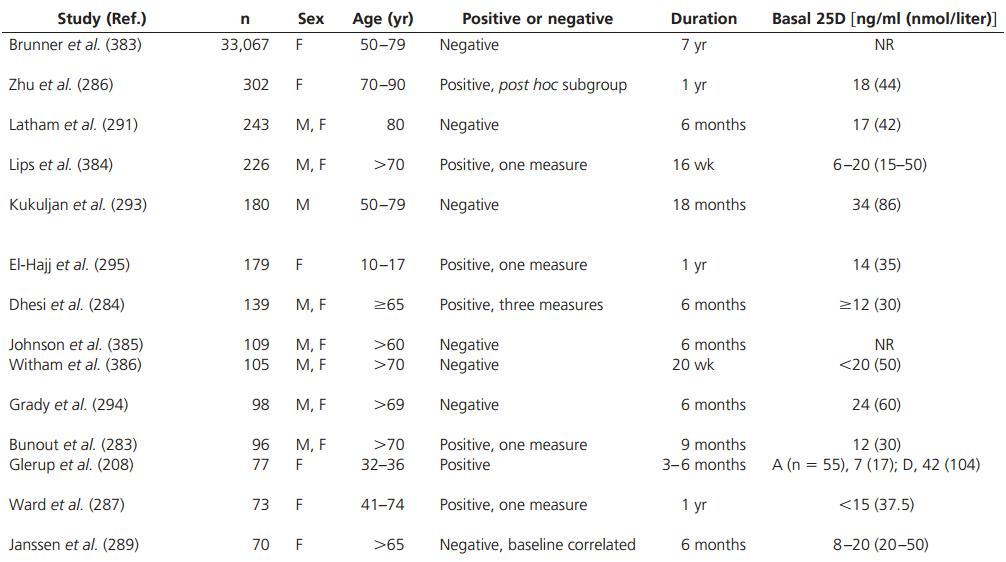
Doses for vitamin D and calcium are daily and administered orally (unless stated otherwise). A, Arab women; AFPT, aggregate functional performance time; CF, cardiac failure; CrCl, creatinine clearance; CRT, choice reaction time; CommD, community dwelling; D, Danish women; FEFA, frail elderly functional assessment score; Hosp, in hospital; ITT, intention-to-treat analysis; LSGC, long-stay geriatric care units; MCT, modified Cooper test; MRS, magnetic resonance spectroscopy; Quads, quadriceps strength; PAS, physical activity/performance score; TST, to stand test; WHI, Women's Health Initiative.
6. Summary: vitamin D, muscle strength, and physical performance
Although some data suggest a beneficial effect of vitamin D supplementation on muscle function, particularly in vulnerable populations and those with low baseline vitamin D levels (208, 286), the evidence base is limited by highly heterogeneous studies that assess muscle function by different methods. Hence, larger studies that use standardized, reproducible assessments of muscle strength and double-blinded treatment regimens are necessary to clarify this important issue and guide recommendations. Such studies should ideally consider baseline vitamin D status and confirm adequate replacement is achieved by a rise in 25D to the normal range.
G. Muscle morphology and electromyography (EMG)
Several reports, dating back to the 1970s, have characterized the morphological appearance of skeletal muscle among vitamin D-deficient subjects and thus provided some evidence in support of a direct role for vitamin D in the morphology and development of muscle.
TABLE 7. (just the top)
1. Open-label studies
In 1974, a case series of 13 patients with various degrees of proximal myopathy in the context of chronic renal failure was described (203). Ten of the 13 patients displayed significantly shorter mean action potential durations of the deltoid and quadriceps muscles on EMG. They also displayed moderate atrophy of type II (i.e. fast twitch) muscle fibers on the basis of myofibrillar ATPase staining and degenerative changes on electron microscopy with small foci of fiber necrosis, lytic vacuoles, and Z-band degeneration in four patients. Although vitamin D levels were not determined, because this was before the era ofthe standardized assay, substantial improvement in muscle strength after im vitamin D treatment in a proportion of the patients was reported. In another series of four uremic patients, the finding of type II muscle fiber atrophy was linked to vitamin D deficiency on the basis of significantly elevated PTH levels (298).
In 1975, gluteal muscle biopsies of 12 patients with laboratory evidence of osteomalacia displayed nonspecific muscle fiber atrophy (299). A distinction was made between patients with isolated nutritional deficiency in whom biopsy changes were mild compared with those with an additional condition including hyperparathyroidism, hyperthyroidism, or uremia who also demonstrated myofibrillar degeneration and infiltration with amorphous material.
One year later, Irani (201) reported a case series of 15 women with nutritional osteomalacia who demonstrated significantly shorter motor unit action potentials and a greater proportion of polyphasic potentials on EMG compared with controls. Muscle biopsies from those with osteomalacia demonstrated nonspecific muscle fiber atrophy. Complete resolution in EMG changes after a 5-wk course of high-dose vitamin D supplementation (600,000 IU of vitamin D2 weekly or fortnightly) was noted in the three patients who were retested. In 1979, two patients with osteomalacia demonstrated type II muscle fiber atrophy in addition to scattered necrosis and derangement of the intermyofibrillar network on muscle biopsy (300).
Eleven patients with a condition described as bone loss of aging had muscle biopsies from the vastus lateralis before and after treatment with 1a-OHD3 and calcium for 3-6 months (301). The predominant finding was an increase in the proportion and cross-sectional size of fast-twitch type IIa fibers. Measures of the oxidative capacity of muscle, succinate dehydrogenase, and total phosphorylase activity were low at baseline and increased with treatment. Lactate dehydrogenase activity, a measure of anaerobic metabolism, did not change. Interestingly, the proportion of type IIb fibers (very-fast-twitch fibers) decreased significantly with treatment. This was the first report to demonstrate changes in muscle morphology and oxidative capacity after treatment of presumably vitamin D-deficient subjects with a vitamin D analog.
Three years later, Young et al. (302) confirmed these findings by demonstrating significant increases in the proportion of type II muscle fibers in biopsies of the vastus lateralis muscle after 3 months of vitamin D supplementation among 12 patients with osteomalacia. In association with these findings, quadriceps muscle strength also improved significantly using an isodynamic dynamometer. However, this body of evidence dating back to the 1970s may be confounded by the many biochemical abnormalities associated with renal failure and osteomalacia such as hyperparathyroidism and disturbances in calcium and phosphate levels. These provide indirect mechanisms that may independently alter muscle function (Fig. 4). Nevertheless, the changes in muscle morphology and performance after vitamin D supplementation in these subjects are important preliminary observations.
Recent studies have reported an association between significantly higher skeletal muscle fat content and vitamin D deficiency. In one study of 90 postpubertal females in California, the proportion of muscle fat, assessed by comparing the attenuation signal of a 2-cm2 section of the rectus femoris with the adjacent sc fat on computed tomography, was found to strongly correlate in an inverse fashion with serum 25D levels (303). This was independent of body mass or computed tomography measures of sc and visceral fat. The percentage of muscle fat was significantly lower in women with normal vs. subnormal serum 25D levels.
In another study of 366 older patients receiving magnetic resonance imaging (MRI) of one shoulder for the investigation of potential rotator cuff injury, a correlation between higher fatty infiltration of rotator cuff muscles and lower serum levels of 25D was reported (304). After multivariate linear regression analysis, this association remained statistically significant in two muscle groups (i.e. supraspinatus and infraspinatus muscles) but only among those whose MRI also demonstrated a full-thickness rotator cuff tear (228 patients).
A third study using MRI of the thigh in 20 older subjects also reported an inverse correlation between muscular fatty degeneration and 25D (305). Interestingly, selective and near-total fatty degeneration of at least one muscle was observed among 11 vitamin D-deficient patients [25D <20 ng/ml (50 nmol/liter)].
A recent cross-sectional study demonstrated a positive correlation between 1,25D levels and total skeletal muscle mass as measured on DEXA among subjects younger than 65 yr (306). This was supported by greater isometric knee extension moment in women with higher 1,25D levels. However, no association was found between 25D levels and muscle mass or strength or in those over 65 yr of age. Among 26 subjects with chronic kidney disease, thigh muscle cross-sectional area on MRI correlated significantly with a model including 1,25D levels, calcium levels, and daily physical activity (307). Functional parameters assessing gait and proximal musculature also independently correlated with 1,25D.
Although a majority of highly trained adolescent male ballet dancers had low vitamin D levels [25D <20 ng/ml (50 nmol/liter) in nine of 16 study participants], there was no correlation between 25D, body composition on DEXA, or reports of muscle injury in this study (308).
2. EMG and muscle biopsies: randomized study
A study that randomized 96 elderly women with post-stroke hemiplegia and severe vitamin D deficiency [<10 ng/ml (25 nmol/liter)] to vitamin D2 (1000 IU daily) or placebo for 2 yr reported significant and dramatic increases in the proportion and diameter of type II muscle fibers (85). These parameters deteriorated significantly in the placebo group.
3. EMG and muscle biopsies: summary
In summary, it appears that vitamin D deficiency results in significant and reversible changes in EMG and type II muscle fiber atrophy, the latter being an independent predictor for falls in one study (85). However, the changes are nonspecific, being similar to those seen in other conditions. Although fatty infiltration in skeletal muscle has been suggested by three recent studies, these are cross-sectional and based on imaging modalities that may not be validated for the assessment of muscle fat. Muscle becomes fatty with disuse, and thus this measure may be confounded by decreased exercise associated with both increased muscle lipid and lower vitamin D. These modalities are not equipped to identify intracellular fat, perhaps of greater pathophysiological significance.
H. Insulin sensitivity and glucose handling
A broad range of epidemiological and randomized clinical studies together with specific research on molecular pathways and animal models have drawn links between vitamin D and insulin sensitivity. This is relevant to the topic of vitamin D and muscle because under normal physiological conditions, skeletal muscle is responsible for approximately 85% of whole-body insulin-mediated glucose uptake (102).
Insulin resistance, a highly prevalent condition that contributes to the pathogenesis of type 2 diabetes, is primarily due to defective insulin-stimulated glucose uptake in skeletal muscle resulting from the production of various inflammatory mediators, adipokines, and FFA by adi-pocytes in predominantly overnourished and obese individuals (309). However, in recognizing the complex processes involved in insulin resistance, a number of reversible factors with potential etiological relevance to this condition are being considered. One of these factors is vitamin D deficiency. In this section, we will review human clinical studies that examine the association between vitamin D status and insulin sensitivity.
I. Cross-sectional studies: vitamin D and insulin sensitivity
Studies have examined the association between parameters of insulin resistance and vitamin D status in nondi-abetic individuals. In one report, 25D was inversely correlated with the homeostasis model assessment of insulin resistance (HOMA-IR) among 214 Arab-American men, but no such association was found among the 317 women of the same ethnicity included in this study (310). Among 808 nondiabetic participants of the Framingham Offspring Study, plasma 25D concentrations were inversely associated with fasting insulin concentrations and HOMA-IR after adjustment for age, sex, and BMI (311). A similar association between 25D levels and HOMA-IR was found in a group of 712 subjects at risk of diabetes (312).
Among 1941 adolescents who participated in the National Health and Nutrition Examination Survey from 2001-2006, adjusted concentrations of insulin were significantly higher among male subjects who were vitamin D deficient [<20 ng/ml (50 nmol/liter)] compared with those with higher vitamin D levels [>30 ng/ml (75 nmol/ liter)], suggesting a potential role vitamin D status in insulin sensitivity (313).
However, a recent study that employed the gold-standard technique in the assessment of insulin sensitivity, namely the hyperinsulinemic-euglycemic clamp, found that the association between insulin sensitivity in 39 non-diabetic subjects and 25D levels become nonsignificant after adjustment for other factors including BMI (314). Similarly, among 381 nondiabetic university students in Lebanon and 510 nondiabetic subjects from a largely obese ethnic minority in Canada (i.e. Canadian Cree), the inverse association between 25D levels and HOMA-IR also became nonsignificant after adjustment for BMI in addition to other factors (315, 316). In another study of 126 healthy young adults, there was a significant association between 25D levels and insulin sensitivity on a hy-perglycemic clamp study that remained after adjustment for a range of factors (317).
Therefore, it is clear that the inverse correlation between 25D and BMI, as reported in a number of studies (314,318), may particularly confound the assessment of these observational data. In fact, a recent study suggests that it may be more accurate to consider adiposity rather than BMI per se as the particular confounding factor (319). In a study of 1882 non-diabetic individuals, it was the inclusion of a computed tomography measure of visceral adiposity rather than BMI and waist circumference in the multivariate analysis that caused the inverse association between vitamin D status and markers of insulin resistance, namely HOMA-IR and log insulin levels, to be insignificant (319).
Several mechanisms associating vitamin D deficiency with obesity have been proposed, including the great capacity of adipose tissue to store vitamin D (80, 320) and the avoidance of sunlight exposure and outdoor activity among potentially self-conscious, obese individuals (320). In confirmation of the former mechanism, a study of 116 obese women reported that fat mass measured by isotope dilution method was a strong predictor of serum 25D levels both 5 yr before and 10 yr after bilio-pancreatic diversion surgery and that vitamin D levels did not correlate with insulin sensitivity at either time on the basis of the euglycemic-hyperinsulinemic clamp studies (321).
The impact of PTH, which has an inverse relation to vitamin D status and is also associated with diabetes (322), has been addressed in a small number of studies. A study including 15 subjects with secondary hyperparathyroidism (serum PTH >6.4 pmol/liter) and 15 controls found that after adjustment for BMI, age, and sex, serum 25D levels were significantly associated with the insulin sensitivity index on a 3-h hyperglycemic clamp, but PTH levels were not (323). Similarly, a significant adjusted association between 25D and fasting insulin was reported in a study of 654 adult subjects from Canada, but PTH was not associated with this parameter after multivariate adjustment (324).
Apart from insulin resistance of skeletal muscle, the pathophysiology of type 2 diabetes comprises a range of other factors. Vitamin D may play a role in these other processes with cross-sectional studies and meta-analyses reporting an association between vitamin D deficiency/ insufficiency and the incidence of diabetes in various populations (325-328). However, not all studies confirm this observation, and there is substantial heterogeneity between studies in their design and adjustment for confounders (329-331).
2. Prospective studies: vitamin D and insulin sensitivity
Observational studies have examined the relationship between 25D and the prospective risk of developing insulin resistance.
In the prospective Ely study (1990-2000), baseline 25D levels of 524 nondiabetic men and women were inversely associated with the 10-yr risk of insulin resistance, on the basis of HOMA-IR and fasting insulin after adjustment for a range of factors including age, sex, BMI, and calcium and PTH levels (332). Each 10-ng/ml (25 nmol/ liter) increase in baseline 25D was associated with a significant decrease in HOMA-IR score (i.e. 0.16 U) at 10 yr.
In a recent study that assessed 5200 participants of the Australian Diabetes, Obesity, and Lifestyle (AusDiab) study, lower baseline 25D levels were associated with a higher risk of developing diabetes over the 5-yr follow-up period (333). After adjustment for a range of factors, the authors reported that each 10-ng/ml (25 nmol/liter) increment in serum 25D was associated with a 24% reduced 5-yr risk of diabetes. Regarding insulin resistance, a positive and independent association with HOMA-IR at 5 yr was also reported. In contrast to an earlier report (334), no association between dietary calcium intake and diabetes risk or the follow-up homeostasis model assessment of insulin sensitivity score was found (333).
Apart from insulin resistance, a number of studies have also reported an association between baseline 25D levels and the long-term risk of diabetes (334-336). However, not all such studies have supported this association (337-339).
3. Interventional studies: vitamin D and insulin sensitivity
Mixed results have emerged from a number of interventional studies that have sought to address the impact of vitamin D supplementation on glucose homeostasis and parameters of insulin sensitivity.
There was no difference in parameters of glucose homeostasis among 238 postmenopausal women who were randomized to receive 2 yr of treatment with vitamin D3 (2000 IU daily) or la-OHD3 (0.25 jug daily) or 1 yr of treatment with 1,25D (0.25-0.50 jug) daily vs. placebo (340). Similarly, no differences in insulin-mediated glucose uptake on the euglycemic clamp study were found in 18 healthy males randomized to receive either 1,25D 1.5 ug daily or placebo; however, treatment in this study was only 7 d (341).
Studies examining subjects at risk of diabetes have suggested improvements in glucose homeostasis with vitamin D supplementation. In three studies, significant improvements were reported in insulin sensitivity, insulin secretion, and/or the disposition index in subjects at risk of diabetes who were randomized to receive supplemental vitamin D3 and calcium (2000 IU and 500 mg, respectively) vs. calcium alone for 16 wk, high-dose vitamin D3 (120,000 IU) every 2 wk vs. placebo for 6 wk, and vitamin D3 and calcium (700 IU and 500 mg daily, respectively) vs. placebo for 3 yr (342-344).
A double-blind randomized trial of 81 South Asian women living in New Zealand who were found to be both insulin resistant on HOMA-IR and vitamin D deficient [25D <20 ng/ml (50 nmol/liter)] reported significant reductions in insulin resistance and fasting insulin levels among those randomized to receive vitamin D3 (4000 IU daily) vs. placebo for 6 months (345).
In a recent randomized trial including 90 diabetic subjects, those randomized to receive vitamin D-fortified yogurt twice daily (each containing 500 IU) or vitamin D- and calcium-fortified yogurt demonstrated improved glycemic control on glycated hemoglobin (HbA1c) and improved insulin resistance on HOMA-IR compared with those receiving plain yogurt for 12 wk (346). Importantly, an inverse correlation was observed between changes in serum 25D and HOMA-IR in this study.
In another study, 10 females with type 2 diabetes who were predominantly vitamin D deficient reported a significant reduction in a marker of peripheral insulin resistance after 1 month of vitamin D3 supplementation (1332 IU daily) (347). However, this study had no control group.
Conversely, a number of small studies have failed to demonstrate any benefits in association with vitamin D supplementation in patients with type 2 diabetes. In 20 diabetic subjects, a randomized trial reported no improvements in fasting or stimulated glucose, insulin, C-peptide, or glucagon concentrations among those receiving 1,25D (1 ug daily) for 4 d vs. placebo (348). Among 28 Asian Indian patients with type 2 diabetes, those randomized to receive vitamin D supplementation for 4 wk did not demonstrate a significant difference in markers of insulin resistance (i.e. fasting insulin, post-oral glucose tolerance test serum insulin levels, and HOMA-IR) compared with those receiving placebo (349). Similarly, in 32 diabetic subjects, 6 months of supplemental vitamin D (40,000 IU/wk) had no effect on fasting insulin, C-peptide, or HbA1c levels compared with baseline or those receiving placebo (350). It is probably reasonable to conclude that these studies were underpowered to answer the question in either direction.
In one case series of three British Asians with diabetes and vitamin D deficiency [25D <6 ng/ml (15 nmol/liter)], high-dose vitamin D supplementation (300,000 IU im) was associated with subsequent deterioration in glycemic control on HbA1c and progression of insulin resistance on fasting insulin resistance index (351).
Recent post hoc analyses of eight trials including participants with normal glucose tolerance at baseline and three small trials of patients with established type 2 diabetes demonstrated no effect of vitamin D supplementation on glycemic outcomes (352). However, two trials examining patients with baseline glucose intolerance reported improvements in insulin resistance among those receiving vitamin D supplementation (349, 350).
4. Summary: vitamin D and insulin sensitivity
Substantial differences in study design, duration, and type of vitamin D supplementation and the particular populations studied in these trials make collective assessment of these results difficult. Although some large trials suggest a beneficial effect of vitamin D supplementation in the reduction of insulin resistance, others do not. Furthermore, to ascertain whether the potential glycemic benefits of supplemental vitamin D are more pronounced in those with vitamin D deficiency or poor glycemic control at baseline, larger trials of longer duration are necessary. More than 20 trials are currently under way to address this question (www.clinicaltrials.gov).
VII. Conclusions
See Table 8 for conclusions.
In his 1922 publication on the cure of rickets by sunlight, Alfred Hess (35) remarked that "although we have realized the importance of light in the growth of plant life, we have [until now] accorded it too little significance in the development of animal life." Since that time, we have come a long way in recognizing the role of UV radiation in the photochemical synthesis of vitamin D, the role of vitamin D in calcium and mineral homeostasis, and the similarity of 1,25D to members of the steroid family with their cholesterol precursor, carbon-ringed structures, and ability to bind to specific nuclear receptors in the genomic mediation of developmental and functional effects.
Although steroid hormones are known to exert diverse effects in multiple organs and tissues, a role for vitamin D beyond its predominant effects on bone and mineral homeostasis has been hotly contested. Muscle stands at the frontier of the emerging concept of vitamin D's extraskeletal role because it shares its ancestral origin with bone in the common mesenchymal stem cell and relies heavily on intracellular calcium handling for contraction, insulin sensitivity, and cellular plasticity (99).
TABLE 8. Conclusions and outstanding questions
Conclusions
Vitamin D exerts rapid and genomic effects in primary muscle cells and cell lines. These effects relate to intracellular calcium handling,differentiation and contractile protein composition.
In vivo, it is not clear whether VDR is expressed in adult skeletal muscle.
Whole-body VDRKO mice and vitamin D-deficient animals display significant defects in muscle function and development.
In humans, single nucleotide polymorphisms in the gene encoding VDR have been associated with differences in muscle strength.
Changes in muscle morphology in humans with severe vitamin D deficiency have been reported since the 1970's.
Proximal myopathy and muscle pain in subjects with severe vitamin D deficiency resolve following vitamin D supplementation.
Associations between vitamin D deficiency, muscle weakness and falls are confounded by factors including frailty and lower exposure to sunlight.
- Clinical parameters of muscle function are not standardized making data aggregation difficult.
Randomized data suggest that vitamin D supplementation may reduce falls in older individuals but not all studies support this conclusion.
The recommended dose of vitamin D supplementation and vitamin D targets remain hotly contested issues.
Outstanding questions
Does the VDR exist in fully differentiated adult muscle and does it have physiological relevance at this site?
- Or rather, as suggested by in vitro studies, is its role predominantly related to the function of immature muscle cells such as in myogenesis?
Are changes in muscle function and morphology directly related to vitamin D or indirectly to its effects in calcium and mineral homeostasis?
Does skeletal muscle possess the ability to 1-a-hydroxylate 25D at any stage in its development?
- As suggested by studies on phosphate handling in myocytes, does 25D itself exert direct effects on muscle?
- Is vitamin D deficiency or its reversal an important consideration among those with other muscle disorders such as congenital dystrophies and acquired immune-related myositis?
In this review, we have adopted a multilayered approach in examining evidence from human clinical studies as well as reports on animal and cell models to piece together the current knowledge of vitamin D's effects in skeletal muscle. The broad evidence base is generally in favor of a role for vitamin D in the development and function of skeletal muscle.
The strongest evidence comes from studies that report distinct morphological changes in the muscle of vitamin D-deficient subjects, others that describe significant impairments in the muscle function of VDRKO mice, and molecular studies that have mapped out the various intracellular responses of cultured muscle cells to vitamin D (129, 173, 174). As a result, we have come closer to answering the perennial question as to whether vitamin D's influence on muscle is direct or indirect, and the answer appears to be both.
Outstanding questions remain, including the precise role of vitamin D in muscle differentiation, the possibility of specific biological activity of 25D in muscle, and the current controversy regarding the in vivo presence of the VDR in muscle tissue.
In the clinical domain, observations of reversible myopathy in subjects with severe vitamin D deficiency have been reported for some time. Cross-sectional data reporting a high prevalence of vitamin D deficiency among subjects with falls, muscle weakness, and insulin resistance are also present (211, 274,327). However, confounding variables are a caveat in the interpretation of this circumstantial evidence. Furthermore, the demonstration of unequivocal improvements in muscle function among subjects with mild to moderate degrees of vitamin D deficiency randomized to receive vitamin D supplementation has been elusive. Possible reasons for this include heterogeneity in study design and supplemental regimens and the general lack of large-scale trials to address this issue. These challenges and others remain to be addressed.
There is reasonable evidence from cellular, animal, and at least some human studies that muscle responds to vitamin D. Although molecular pathways by which vitamin D acts on the myocyte have been identified, there is scope for more clarification. Studies are also needed to clarify the therapeutic potential of vitamin D in the treatment of age-related sarcopenia and perhaps other myopathies. In the meantime, it would be prudent for clinicians to seek and manage vitamin D deficiency in individuals at risk of these conditions.
Acknowledgments
The authors gratefully acknowledge Professor John Eisman (Garvan Institute of Medical Research, Sydney, Australia) for reviewing the manuscript.
Address requests for reprints to: Dr. Christian M. Girgis or Associate Professor Jenny E. Gunton, Garvan Institute of Medical Research, 384 Victoria Street, Darlinghurst, New South Wales, Australia. E-mail: c.girgis@garvan.org.au or j.gunton@garvan.org.au.
Disclosure Summary: C.M.G. received salary support from a postgraduate scholar award from University of Sydney. J.E.G. received funding from the Diabetes Australia Research Trust and the National Health and Medical Research Council. The remaining authors have no conflicts of interest to report.
