Why Mendelian randomization fails with Vitamin D
When Mendelian randomisation fails
BMJNPH: first published as 10.1136/bmjnph-2021-000265 on 22 March 2021
Martin Kohlmeier mkohlmeier@unc.ed , Emmanuel Baah
📄 Download the PDF from VitaminDWiki
Mendelian randomisation (MR) is the ingenious approach of using the consistent long-term modulation of interesting exposure variables by inborn genetic differences to mimic the effect of different levels on outcomes of interest. This type of analysis is particularly important for evaluating the causal impact of nutritional exposures on longterm health outcomes. The MR approach is predicated on equivalent effects of exposure and genetic proxy on the outcome. But what happens when the proxy is not a good predictor of the outcome of interest? MR analysis of the hypothesised role of vitamin D in the pathology related to SARS-CoV-2 infection illustrates this conundrum.
Up to this point, a growing number of observational studies appeared to link low 25-hydroxy vitamin D (25- OHD) concentrations to higher risk of infection and worsening COVID-19 outcomes.1 For instance, the analysis of 25-OHD measurements in more than 190 000 clinical samples from across the USA found that the likelihood to test positive for SARS-CoV-2 was more than twice as high for samples with low 25-OHD
concentration (<20 ng/mL) than for samples with high concentration (>55 ng/mL).2 The findings based on UK Biobank data which include clinical outcomes are possibly different because the observed 61% higher mortality risk for the univariate association with low vitamin D concentration disappeared after adjustments.3 An argument can be made that adjustments for age, sex, ethnicity and body mass index were inappropriate because it is exactly these variables that are well-known causes of low vitamin D concentrations. No plausible rationale was offered that they actually confound the association, that is, that ethnicity is the cause for higher risk and not lower capacity for producing vitamin D in people with darker coloured skin.
Vitamin D concentrations tend to be low in patients with COVID-19. Thus, the majority of patients with COVID-19 in a Belgian hospital was found to be vitamin D-deficient, and the ones most severely affected by the illness had the lowest levels.4 This is apparently not just an acute response to the infection and due to pathological changes occurring with COVID-19. Individuals with low 25-OHD concentrations measured long before infection were over-represented among patients hospitalised because they needed treatment for COVID-19.5
Risk of infection and severity of illness also appear to be related to vitamin D intake. Based on data from the UK Biobank, habitual users of vitamin D-containing supplements had a 34% lower risk of infection.6 Another large study of dietary supplement use assessed with a widely distributed app also found slightly lower risk of infection in people using vitamin D supplements.7 As described below, a randomised controlled trial (RCT) found high-dose vitamin D to be highly effective in ameliorating COVID-19 in hospitalised patients.8
Finally, ecological studies demonstrate a strong latitudinal gradient of high to low COVID-19 mortality from North to South.9 10 This has been attributed to the diminished ability of people living at higher latitudes, such as in the UK, Central and Northern Europe, Canada and the northern parts of the USA, to get UV-B light for vitamin D production in skin during the darker months.
The reliability of these findings is now put in doubt by MR analyses. Two papers in this Journal suggest that the genetic variants responsible for much of the variation in vitamin D concentration in serum/plasma do not predict COVID-19 outcomes,11 12 confirming previous findings.13 What could be the underlying reason for this discrepancy between the previously reported results and the lack of a genetically linked causal effect detectable by MR?
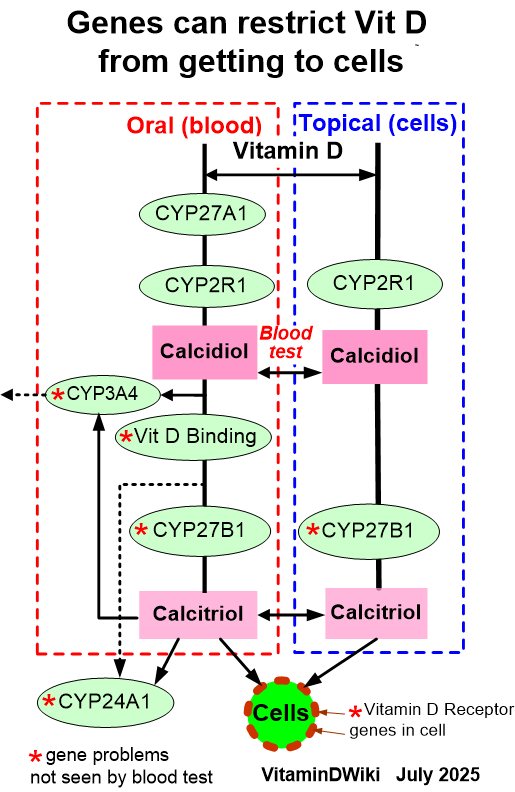
It may all come down to the use of 25-OHD concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response.14 For most other purposes, it may not matter much that unbound (free) 25-OHD is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25-OHD and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all.15 As shown in figure 1, total vitamin D concentration was 30% lower in people with two copies of rs4588A/rs7041T than in those with none, but the difference in free vitamin D concentration was much smaller and statistically not significant (figure 1). Hence, much of the genetic variation used by the instrument for the MR analysis is likely to have little impact on the risk of deficiency. It has been argued before that the correct metric for predicting vitamin D functional adequacy is the concentration of unbound (free) 25-OHD, not the total 25-OHD concentration.16 When the genetic proxy does not reliably predict functional vitamin status, it loses its ability to assess the causality of the link with COVID-19 outcomes.
As this MR analysis fails, it specifically cannot tell us whether supplemental vitamin D intake reduces COVID-19 risk. Instead, we need to take seriously actual reports of beneficial effects of vitamin D supplements on COVID-19 risk because this direct measure sidesteps altogether the reliance on vitamin D concentrations as a surrogate marker for the assessment of vitamin D status.6 7
More guidance from a well-designed RCT would be nice to have at this stage. A modestly sized RCT tested the effect of high-dose vitamin D supplementation in patients with COVID-19 and found a powerful benefit.8 No such benefit with supplementation was found in another RCT conducted in Brazil.17 In that study, a single high dose (200 000 IU vitamin D3) was started on average more than l0 days after symptomatic disease had begun. Supplementation was probably too late to make up for pre-existing deficiency and to affect disease outcome. Yet another small RCT, conducted in India with confirmed vitamin D-defi- cient patients with COVID-19 getting high doses (60 000 IU vitamin D3 per day), found that the virus had become undetectable after 3 weeks three times as often in supplemented patients as in non-supplemented ones, which is a beneficial effect.18
More RCTs are planned or underway. Until more such data become available, daily use of a moderately dosed vitamin D supplement to prevent deficiency would be preferable.19 Once infected, it is particularly important to start supplementation at the earliest possible time after virus detection. Waiting for the initiation and completion of additional RCTs until everybody is convinced about the effectiveness of vitamin D comes with staggering costs for each further day of delay. Currently, many thousands of people are dying daily and many more are suffering from the
ravages of severe COVID-19 in regions where vitamin D deficiency and insufficiency are common at this time of the year. The economic costs, societal losses and other detrimental consequences of a persisting pandemic are undeniably enormous. And yet, where are the decisive public health measures and policies to correct with high priority the known seasonal epidemic of vitamin D deficiency? Where are the urgent efforts to generate the critically needed RCTs to test the vitamin D hypothesis?
In some sense, COVID-19 can be seen as a deficiency disease because respiratory viruses spread opportunistically across populations with nutritionally diminished innate immune defences. The nutrients most needed for innate immune response are likely to include vitamin D and a few other food constituents.
If the considerations outlined above about the disconnect between GC genotype-related 25-OHD concentration differences and functional outcomes are correct, several implications follow:
The GC genotypes that modulate concentrations of both VDBP and 25-OHD are probably not good predictors of vitamin D requirements and should not be used for MR studies.
Total vitamin D concentrations measured in blood may be less useful in some people and under some circumstances, when they are strongly influenced by genetic or non-genetic modulators of VDBP concentration.
Unbound (free) vitamin D concentrations may have to be reconsidered as the measurement of choice for the assessment of vitamin D status.
REFERENCES
Yisak H, Ewunetei A, Kefale B, e't a/. Effects of vitamin D on COVID-19 infection and prognosis: a systematic review. Risk Manag Hea/thc Po/icy 2021;14:31-8.
Kaufman HW, Niles JK, Kroll MH, eta/. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One 2020;15:e0239252.
Hastie CE, Mackay DF, Ho F, et a/. Vitamin D concentrations and COVID-19 infection in UK Biobank. Diabetes Metab Syndr 2020;14:561-5.
De Smet D, De Smet K, Herroelen P, et al. Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality. Am J Clin Pathol 2021;155:381-8.
Meltzer DO, Best TJ, Zhang H, et al. Association of vitamin D status and other clinical characteristics with COVID-19 test results. JAMA Ne^ Open 2020;3:e2019722.
Ma H, Zhou T, Heianza Y, et al. Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank. Am J Clin Nutr 2021:nqaa381.
Louca P, Murray B, Klaser K. Dietary supplements during the COVID-19 pandemic: insights from 445,850 users of the COVID symptom study APP. BMJ Nutr Prev Health 2021.
Entrenas Castillo M, Entrenas Costa LM, Vaquero Barrios JM, et al. "Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study". J Steroid Biochem Mol Biol 2020;203:105751.
Kohlmeier M. Avoidance of vitamin D deficiency to slow the COVID-19 pandemic. BMJ Nutr Prev Health 2020;3:e000096:67-73.
Rhodes J, Dunstan F, Laird E, et al. COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D. BMJ Nutr Prev Health 2020;3:e000110:118-20.
Amin HA, Drenos F No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data. BMJ Nutr Prev Health 2021;8:bmjnph-2020-000151.
Patchen BK, Clark AG, Hancock DB. Genetically predicted serum vitamin D and COVID-19: a Mendelian randomization study. BMJ Nutr Prev Health 2021.
Butler-Laporte G, Nakanishi T, Mooser V. Vitamin D and Covid-19 susceptibility and severity: a Mendelian randomization study. MedRxiv 2020.
Calder PC. Nutrition, immunity and COVID-19. BMJ Nutr Prev Health 2020;3:e000085:74-92.
Sollid ST, Hutchinson MYS, Berg V, et al. Effects of vitamin D binding protein phenotypes and vitamin D supplementation on serum total 25(OH)D and directly measured free 25(OH)D. Eur J Endocrinol 2016;174:445-52.
Bikle DD. The free hormone hypothesis: when, why, and how to measure the free hormone levels to assess vitamin D, thyroid, sex hormone, and cortisol status. JBMR Plus 2021;5:e10418.
Murai IH, Fernandes AL, Sales LP, et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. JAMA 2021;325. doi:10.1001/jama.2020.26848. [Epub ahead of print: 17 Feb 2021].
Rastogi A, Bhansali A, Khare N, et al. Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (shade study). Postgrad Med J 2020. doi:10.1136/ postgradmedj-2020-139065. [Epub ahead of print: 12 Nov 2020].
Lanham-New SA, Webb AR, Cashman KD, et al. Vitamin D and SARS-CoV-2 virus/ COVID-19 disease. BMJ Nutr Prev Health 2020;3:e000089:106-10.
