Vitamin D acts as a compound
Nutrients are different from allopathic medicines, they are not 'medication against diseases' as they are sometimes marketed, but are necessary components of the metabolic processes in the body. If all these physical processes can run optimally, health emerges from the overall system of all these networked processes, which are interdependent and strongly interrelated. If, on the other hand, some of these processes are disturbed due to nutrient deficiencies, diseases arise. Since all these processes are closely interrelated, there are always several nutrients that interact. Also vitamin D is no exception:
| Vitamin D can only fulfill its role in the body, even if the supply of other nutrients is given, which strongly intervene in the action of the vitamin D. |
All effects of vitamin D are dependent on other nutrients. These include:
-
The conversion of vitamin D3 into its active form
-
The activation of genes
-
Activation of enzymes and proteins
-
The calcium recovery
In addition, there are numerous indirect interactions that affect the regulation of the vitamin D hormone.
The most important nutrient combinations
This article will discuss the most important direct interactions and nutrient combinations that are directly relevant to the effect of vitamin D and good vitamin D supply. Vitamin D interacts with the following nutrients:
| nutrient | interaction | Requirements * | Frequency of deficiency ** | Overdosing? | Combination with vitamin D recommended? |
| Calcium | Vitamin D controls the intake | 1000 mg | medium | Yes | Yes, at low calcium level. Together with magnesium. As a citrate. |
| phosphorus | Vitamin D controls the intake | 700 mg | Very low | Yes | No, supply is very good. |
| Vitamin K2 | Activated by vitamin D formed proteins, ensures the transport and the utilization of calcium | 70 μg | Medium to high | No | Yes, generally. Approximately 100 μg K2 per daily dose of vitamin D. Used as vitamin K2 MK7. |
| magnesium | Needs to convert vitamin D to its effective form | 400 mg | medium | medium | Yes, in the case of unsafe magnesium supply. As gluconate or citrate. |
| Vitamin A (retinol) & beta-carotene (vitamin A precursor) | Controls together with vitamin D genes, mutual regulation | 1 mg | Very low | Yes | Only in case of poor supply. The best thing about food. In preparations as a natural (9-cis) beta-carotene (vitamin A precursor) to prevent overdosage. |
| zinc | Needs to form vitamin D receptors | 10 mg | low | Yes | Only at low recording. |
| Boron | Contribute to the metabolism of the mineral | KA | No studies | From? | No recommendation possible |
* Required for adults, according to DGE * assessment where available according to the National Nutrition Survey II, otherwise lt in Germany. Corresponding studies
Vitamin D, calcium and phosphorus / phosphates
One of the best known functions of vitamin D is its important role in the uptake of calcium and phosphate in the intestine: only by vitamin D can the two substances from the diet be absorbed and made usable for bone formation and energy metabolism. Vitamin D is therefore important for bone health, but plays only the role of a mediator and can have no effect if the supply of calcium and phosphorus is not given.
Calcium: too little is just as harmful as too much
Calcium is important for bone formation, but also for muscles, nerves, the utilization of starch to sugar, cell division, the preservation of cell membranes, blood coagulation, the activation of numerous enzymes and hormones and the regulation of the pH. A good supply is therefore important, but today is also given in most cases. An under-supply with calcium, below the recommended daily intake of 1000 mg is to be assumed in the German-speaking area with only about 30 percent of the adults. (1-3) Those who regularly eat cheese can almost always meet their needs in this way - but there are also some well-plant sources, especially in seeds and nuts, dark green leafy vegetables and dairy products. The plant sources are much better than milk products, which have a very unfavorable mineral profile. (see below)
| food | Content of calcium mg / 100g |
| Poppy seeds | 1460 |
| Emmentaler | 1370 |
| Hard cheese (eg Parmesan) | 1100 |
| Butter cheese | 1000 |
| Gouda | 960 |
| sesame | 780 |
| Camenbert | 600 |
| almond | 250 |
| Hazelnuts | 225 |
| Amaranth | 215 |
| Kale | 210 |
| arugula | 160 |
| spinach | 120 |
| milk | 120 |
| Kidney beans | 100 |
Too much calcium, on the other hand, is not good because it can accumulate in the vessels and organs, which can cause severe health damage.
Calcium: Always together with magnesium
The intake of calcium by dietary supplements is only recommended in exceptional cases, since overdosing is harmful to health. If so, the chemical form of calcium citrate, which is best absorbed by the body, should be used. A good alternative is the Sango coral, which has an almost ideal mineral profile. Calcium should also always be taken together with magnesium in order to preserve the delicate balance of the two minerals . Magnesium ensures that calcium remains dissolved in the blood and does not accumulate as harmful plaque in the vessels. The ratio of calcium to magnesium in dietary supplements should be at least 2: 1, more preferably 1: 1, since the diet usually contains much more calcium than magnesium.
Phosphorus - a question of equilibrium
Vitamin D also regulates the uptake of phosphorus, which is next to calcium the most common mineral in our body. Conversely, phosphorus also regulates the conversion of vitamin D into its effective form. (4) Too much phosphorus intake in relation to calcium has negative effects: high phosphorus levels regulate the vitamin D hormone, which means that less calcium is absorbed. The body then releases calcium from the bones, which can lead to osteoporosis. Too much phosphorus also leads to a disturbed calcium utilization and to the calcification of muscles and arteries, which is a significant health hazard. (5, 6) The ratio of phosphorus to calcium should preferably be at most 1: 1, but today's diets usually contain a far higher phosphorus content. This is particularly critical in the case of excessive consumption of animal products, where the ratio is partly 20: 1 in favor of phosphorus. Just as critical are lemonades: A glass of cola something contains up to 500 mg of phosphorus - thus almost the entire day requirement. Milk is therefore not a suitable calcium source because of the high phosphorus content, despite the high calcium content. Phosphorus should not be included in food supplements other than some diseases.
Vitamin D and vitamin K2
Special attention has been paid to the relationship between vitamin D and vitamin K2. The relatively unknown vitamin K plays an important role in the transport and utilization of the absorbed calcium. (7) While vitamin D is responsible for the uptake of calcium, Vitamin K ensures that it gets to where it is needed. In addition, vitamin K is responsible for activating the proteins formed by the mediation of vitamin D and vitamin A - without vitamin K, these vitamins are therefore ineffective in many aspects.
Vitamin K2 protects against calcification
Without vitamin K2 there is a risk that the calcium can not be used by the body and that it accumulates in tissues and vessels as plaque. (8, 9) This can lead to calcifications in the form of kidney stones and arteriosclerosis and involves numerous health risks. (10) Vitamin K activates on the one hand the so-called Matrix GLA protein (MGP), which protects arteries and tissues from calcifications. An important function, because arterial calcification is one of the most important causes of coronary arterial disease and heart attacks. Vitamin K also activates the hormone osteocalcin synthesized by vitamin D, which is responsible for the incorporation of calcium into the bone matrix. (11-13)
| Without vitamin K the calcium absorbed by vitamin D can be harmful to the body. For this reason vitamin D should always be treated with sufficient vitamin K2. |
Vitamin K supply
Adults need 100-200 mcg of vitamin K2 that naturally only occurs in meat, some fermented foods and dairy products. Exact figures are currently not available. That some more common vitamin K1 can be converted to K2 in the body, but this way is impaired in many people. In dietary supplements, various forms of vitamin K2 are used which are referred to as MK4 and MK7. Good products should use the form MK7, which has a better absorption, better effectiveness and longer half-life than the other forms.
Vitamin D and vitamin A
The relationship of vitamin D and vitamin A is an interesting one because it requires a holistic look at the action of vitamins. The two vitamins support each other, but in other cases they are also direct opponents. All non-calcemic effects of vitamin D are indirectly dependent on vitamin A. (14, 15). Thus, the activation of numerous genes and the synthesis of important proteins requires both vitamin A and vitamin D in a balanced concentration. If this ratio is out of balance, the two vitamins behave like direct opponents. (16, 17) Provided they are sufficiently supplied with both vitamins, they regulate and support each other in the effect and also protect against the toxicity of the other vitamin. (18-20) A deficiency of vitamin A thus results that vitamin D can not fulfill its task correctly, while an oversupply affected with vitamin A the effect of vitamin D.
Vitamin A: best as a beta carotene
The supply of vitamin A is very good. Therefore, it is not advisable to eat larger amounts of vitamin A in food supplements. If at all, moderate amounts of beta-carotene should be used - a preform of vitamin A, found in many reddish fruits and vegetables. The body can form as much vitamin A from this pre-vitamin A as it needs for a balance without the risk of overdosing.
Vitamin A: Easily cover the food
Beta-carotene is found in almost all yellow and orange fruits and vegetables (carrots, pumpkins, apricots, peaches), but also in dark green vegetables (spinach, broccoli). The need for 1 mg of vitamin A can be easily covered by food - this is clearly preferable to the use of drugs. Beta-carotene content of various foods:
| food | Content of beta carotene / 100g | Corresponds to vitamin A |
| Apricot (dried) | 35000 μg | 5800 μg |
| Carrot (raw) | 9800 μg | 1630 μg |
| sweet potato | 7900 μg | 1300 μg |
| Green cabbage (raw) | 5200 μg | 860 μg |
| Mango (dried) | 5150 μg | 850 μg |
| spinach | 4800 μg | 800 μg |
| Honey melon | 4700 μg | 780 μg |
| fennel | 4700 μg | 780 μg |
| Mangold | 3500 μg | 580 μg |
| chicory | 3400 μg | 560 μg |
| Red peppers | 2125 μg | 350 μg |
| Kaki | 1600 μg | 260 μg |
| Organic mango juice | 1200 μg | 200 μg |
In the case of food supplements, care should therefore be taken to ensure that no synthetic vitamin A (retinol) is used, but natural beta-carotene. Synthetic beta-carotene should also be avoided, since synthetic (trans-) and natural (9-cis) beta-carotene differ chemically in principle.
Vitamin D and magnesium
Magnesium is involved in all conversion steps that are needed to the vitamin D3 from foods or the synthesis with the aid of the sun turn into its active form.
| Without sufficient magnesium, the body can not use vitamin D because it sticks in the inactive forms. (21) |
This explains, among other things, a "vitamin D-resistant" form of rickets that can only be cured by the administration of magnesium. (22) Only very small quantities of magnesium are required for the conversion of vitamin D, so that this mechanism usually still functions sufficiently well even in the case of medium magnesium supply. Detailed information also in the detailed article:
Alleged side effects of vitamin D are magnesium deficiency
The danger is in this context but also the reverse, namely, that taking high-dose vitamin D supplements can lead to easy to magnesium deficiency when the magnesium supply is bad anyway, the more vitamin D you are taking, the more vitamin D is converted by the body and the more magnesium is consumed. This leads in some cases to the partly reported alleged "side effects of high doses of vitamin D", such as heart stumbling, headaches, muscle cramps and angstacks. These symptoms are actually the consequences of a magnesium deficiency caused by the vitamin D.
Low vitamin D levels due to magnesium deficiency
At the same time can also be a possible cause of low an existing magnesium deficiency Vitamin D levels be. This is a possible explanation why in some people the vitamin D level does not increase despite good sun exposure and / or the intake of supplements: Since the vitamin D can not be converted, the blood level of the 25- (OH) -Vitamin D is not. (23)
Magnesium supply
Adults need about 400 mg of magnesium per day. High concentrations are found in, for example, whole grain products, amaranth, some algae, pumpkin seeds, sunflower seeds, sesame, chocolate, cashew nuts, tempeh and almonds. This is also the best way to ensure the magnesium supply.
| food | Content of magnesium / 100g |
| Sunflower seeds | 420 mg |
| sesame | 350 mg |
| Amaranth | 300 mg |
| Pumpkin seeds | 285 mg |
| Quinoa | 275 mg |
| Cashew | 270 mg |
| Tempeh | 230 mg |
| Almonds | 170 mg |
| peanuts | 160 mg |
| Kidney beans | 150 mg |
| lenses | 130 mg |
| oatmeal | 130 mg |
| Peas | 120 mg |
| Mangold | 80 mg |
| spinach | 60 mg |
In food supplements, magnesium gluconate or magnesium acetate should be used which have a slightly better usability than other forms. (24)
Vitamin D, zinc and boron
The vitamin D receptor, found in almost all cells and responsible for the action of vitamin D, has two zinc molecules at its base. In the case of a strong zinc deficiency, therefore, the vitamin D function can be restricted because the body can not form the corresponding receptors. (25, 26) The Boron trace element, on the other hand, supports the functions of vitamin D on the cell wall and various aspects of vitamin D metabolism. (27) Boron appears to play primarily a role in the metabolism of minerals. (28-30) In both cases, however, a deficiency must obviously be very pronounced in order to lead to a marked impairment of the vitamin D metabolism, which is why this relationship is hardly investigated.
Graph: Vitamin D and its interactions with other nutrients
The following figure shows how the various nutrients are related. 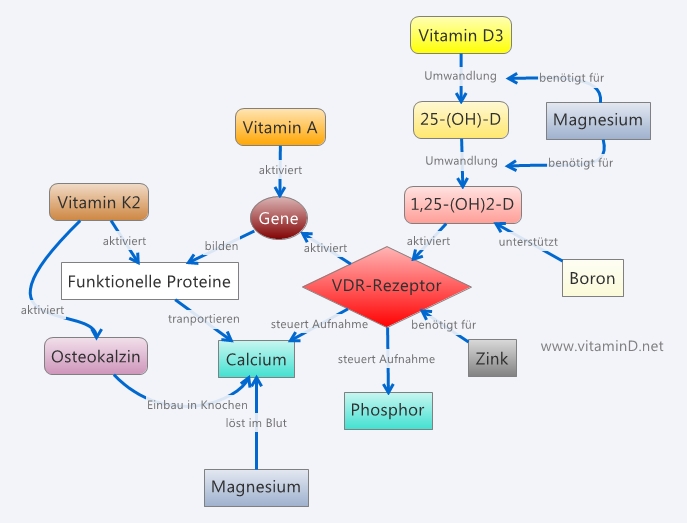
Possible dosage of the vitamin D complex
Food supplements should only be taken when needed. The comments in this article hopefully showed how sensitive the nutrient balance is and how much all nutrients affect. In some cases, however, it may be useful to take the entire vitamin D complex. For example, when problems of the intestine generally make the absorption of nutrients more difficult, or when strong drugs are taken. For these cases, here is a suggestion for a possible dosage in the right ratio of the nutrients.
| nutrient | dosage | form |
| Vitamin D | 2000 IU | Vitamin D3 (cholecalciferol) |
| Vitamin K | 100 μg | Vitamin K2 as MK7 |
| Beta-carotene | 400 μg | Natural (9-cis) beta carotene |
| Calcium | 300 mg | Calcium citrate or -orotate |
| magnesium | 200 mg | Magnesium gluconate or magnesium acetate |
| zinc | 5 mg | Zinc gluconate, zinc orotate |
Conclusion Vitamin D and cofactor
Vitamin D works closely with many other nutrients. Particularly when taking high doses of vitamin D preparations, care should be taken so that no imbalance occurs in this system and a sufficiently high supply with the cofactors is given. Especially vitamin K2 and magnesium are a recommended supplement, as long as the food supply is unclear. Meanwhile, some manufacturers of vitamin D preparations have also recognized these relationships and offer complex preparations that combine vitamin D with some or all co-factors.
sources
-
Heseker H, Adolf T, Eberhardt W, Hartmann S, Herwig A, Kuber W, Matiakse B, Moch KJ, Schneider R & Zipp A (1992) Food and nutrient intakes of adults in the German Federal Republic. In VERA-Schriftenriche, vol. 3; Pp. 188 - 189 W Kubler, HJ Anders, W. Heeschen and D Kohlmeier, editors. Neiderkleen: Fleck publishing house.
-
Van Dokkum W (1995) The intake of selected minerals and trace elements in European countries. Nutrition Research Reviews 8, 271-302
-
Kudlacek, S., Schneider, B., Peterlik, M., Leb, G., Klaushofer, K., Weber, K., Woloszczuk, W. and Willvonseder, R. (2003), Assessment of vitamin D and calcium status In healthy adult Austrians. European Journal of Clinical Investigation, 33: 323-331. Doi: 10.1046 / j.1365-2362.2003.01127.x
-
Portals, AA, et al. Oral intake of phosphorus can determine the serum concentration of 1, 25-dihydroxyvitamin. Journal of Clinical Investigation, 1986, 77th ed., No. 1, p. 7.
-
Jono, Shuichi, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circulation research, 2000, 87. Jg., No. 7, p. E10-e17.
-
Foley, Robert N., et al. Serum phosphorus levels associate with coronary atherosclerosis in young adults. Journal of the American Society of Nephrology, 2009, 20th ed., No. 2, pp. 397-404.
-
Vermeer C, Jie KS, Knapen MH. Role of vitamin K in bone metabolism. Annu Rev Nutr. 1995, 15: 1-22. Review. PubMed PMID: 8527213.
-
Masterjohn C. Vitamin D toxicity redefined: vitamin K and the molecular mechanism. Med Hypotheses. 2007, 68 (5): 1026-34. Epub 2006 Dec 4. PubMed PMID: 17145139.
-
Fu X, Wang XD, Mernitz H, Wallin R, Shea MK, Booth SL. 9-Cis retinoic acid reduces 1-alpha, 25-dihydroxycholecalciferol-induced renal calcification by altering vitamin K-dependent gamma-carboxylation of matrix gamma-carboxyglutamic acid protein in A / J male mice. J Nutr. 2008 Dec; 138 (12): 2337-41. Doi: 10.3945 / jn.108.093724. PubMed PMID: 19022954.
-
Berkner, KL and Runge, KW (2004), The physiology of vitamin K nutriture and vitamin K-dependent protein function in atherosclerosis. Journal of Thrombosis and Haemostasis, 2: 2118-2132. Doi: 10.1111 / j.1538-7836.2004.00968.x.
-
Gallop, Paul M., et al. Carboxylated calcium-binding proteins and vitamin K. New England Journal of Medicine, 1980, 302, ed., No. 26, pp. 1460-1466.
-
(K-dependent proteins in bone). Physiological ReviewsJul 1989,69 (3) 990-1047
-
MJ Shearer, Vitamin K metabolism and nutriture, Blood Reviews, Volume 6, Issue 2, June 1992, Pages 92-104, ISSN 0268-960X, http://dx.doi.org/10.1016/0268-960X(92)90011 -E.
-
Biesalski, Hans K. Vitamin D recommendations-beyond deficiency. Annals of Nutrition and Metabolism, 2011, 59. Jg., No. 1, pp. 10-16.
-
R.R. Sanchez-Martinez, A. Castillo, A. Steinmeyer, and A. Aranda, "The retinoid X receptor ligand restores defective signaling by the vitamin D receptor," EMBO Reports, vol. 7, no. 10, pp. 1030-1034, 200
-
Cannell JJ, Vieth R, Willett W, Zasloff M, Hathcock JN, White JH, Tanumihardjo SA, Larson-Meyer DE, Bischoff Ferrari HA, Lamberg-Allardt CJ, Lappe JM, Norman AW, Zittermann A, Whiting SJ, Grant WB , Hollis BW, Giovannucci E. Cod liver oil, vitamin A toxicity, frequent respiratory infections, and the vitamin D deficiency epidemic. Ann Otol Rhinol Laryngol. 2008 Nov, 117 (11): 864-70. Review. PubMed PMID: 19102134.
-
S. Johansson and H. Melhus, \ "Vitamin A antagonizes calcium response to vitamin D in man, \" Journal ofBone and Mineral Research, vol. 16, no. 10, pp. 1899-1905, 2001.
-
Spiesman IG. Massive doses of vitamins A and D in the Prevention of the Common Cold. Arch Otolaryngol Head Neck Surg. 1941, 34 (4): 787-791.
-
Sanchez-Martinez R., Castillo A, Steinmeyer A, Aranda A. The retinoid X receptor ligand restores defective signaling by the vitamin D receptor. EMBO Rep. 2006, 7 (10): 1030-4.
-
Sánchez-Martínez R, Zambrano A, Castillo AI, Aranda A. Vitamin D-dependent recruitment of corepressors to vitamin D / retinoid X receptor heterodimers. Mol Cell Biol., 2008, 28 (11): 3817-29.
-
Rude RK, Adams JS, Ryzen E, Endres DB, Niimi H, Horst RL, Haddad JG Jr, Singer FR. Low serum concentrations of 1,25-dihydroxyvitamin D in human magnesium deficiency. J Clin Endocrinol Metab. 1985 Nov, 61 (5): 933-40. PubMed PMID: 3840173.
-
Reddy V, Sivakumar B. Magnesium-dependent vitamin-D-resistant rickets. Lancet 1974 May 18; 1 (7864): 963-5. PubMed PMID: 4133647.
-
Zittermann, Armin. Magnesium deficit? Overlooked cause of low vitamin D status ?. BMC medicine, 2013, 11Jg., No. 1, p. 229.
-
Coudray, C., et al. Study of magnesium bioavailability from organic and inorganic Mg salts in Mg-depleted rats using a stable isotope approach. Magnesium research, 2005, 18th ed., No. 4, pp. 215-223.
-
Freedman, Leonard P. Anatomy of the steroid receptor zinc finger region. Endocrine reviews, 1992, 13Jg., No. 2, pp. 129-145.
-
Freedman, Leonard P .; TOWERS, Terri L. DNA binding properties of the vitamin D3 receptor zinc finger region. Molecular Endocrinology, 1991, 5Jg., No. 12, pp. 1815-1826.
-
Hunt, CD (1996), Biochemical effects of physiological levels of dietary boron. J. Trace Elem. Exp. Med., 9: 185-213. Doi: 10.1002 / (SICI) 1520-670X (1996) 9: 43.0.CO; 2-Q
-
Hunt, CD, Herbel, JL and Idso, JP (1994), Dietary Boron Modify the Effects of Vitamin D3. J Bone Miner Res, 9: 171-182. Doi: 10.1002 / jbmr.5650090206
-
Miljkovic, D., Miljkovic, N., & McCarty, MF. Up-regulatory impact of boron on vitamin D function-does it reflect inhibition of 24-hydroxylase ?. Medical hypotheses, 2004, 63rd ed., No. 6, pp. 1054-1056.
-
Hegsted, Maren, et al. Effect of boron on vitamin D deficient rats. Biological trace element research, 1991, 28th ed., No. 3, pp. 243-255.
