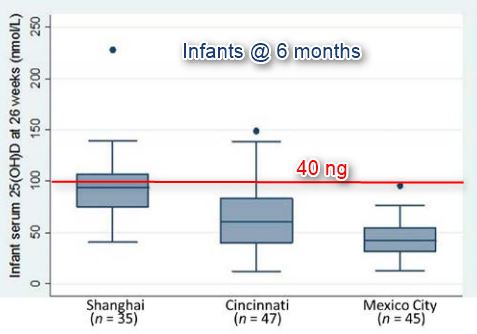
Mexico has low levels of vitamin D (less than 20 ng)
Vitamin D deficiency in children. An opportunity for prevention
Medical Bulletin of the Children's Hospital of Mexico, doi: 10.1016 / j.bmhimx.2015.01.011
Desiree Lopez-Gonzalez to ,Lucia Mendez-Sanchez to ,Miguel Angel Guagnelli to ,Patricia Clark a , b , [osteoclark@gmail.com]
📄 Download the Spanish PDF from VitaminDWiki
The prevalence of vitamin D deficiency in the pediatric population has increased in recent years and are believed to still underdiagnosed and undertreated. According to data from the National Health and Nutrition Survey 2006, Mexico has been estimated prevalence of 16% in children aged 2-12 years . Vitamin D plays a critical role in the formation and bone homeostasis and consequently on growth. Its deficiency is associated with diseases such as rickets and osteomalacia, and has been linked to other conditions such as obesity, metabolic syndrome, diabetes, cancer, respiratory infections and immune system problems. In the literature described specific risk groups for vitamin D deficiency in the supplement could provide a benefit. Currently there is still controversy in defining adequacy serum and supplement dose. In Mexico, the suggested daily intake of vitamin D is 5.6 mg / day (224 IU), which is significantly less than the recommendations in the United States and Europe (between 400 and 1,000 IU). Due to increased vitamin D deficiency in recent years and the lack of consensus regarding the levels of vitamin D sufficiency (as cutoff values ranging from 20 to 30 ng / ml considered by the association of endocrinology) The objective of this review was to provide an overview of the problem in the pediatric population, and to describe those groups at risk and analyze the current recommendations for vitamin D supplement
Vitamin D deficiency has been considered rare in Mexico, and the lack of evidence did not allow to establish the recommended daily intake, according to the National Institute of Medical Sciences and Nutrition Salvador Zubirán. Today, however, must be recognized as a health problem, worthy of attention and action. We suggest that prospective studies are carried out in our country, where the relationship between serum vitamin D deficiency and poor bone mineralization is established.
Abstract
The prevalence of vitamin D deficiency in the pediatric population has Increased in recent years and any continues to be underdiagnosed and undertreated. , According to data from the "ENSANUT 2006" (National Health and Nutrition Survey), the prevalence of vitamin D deficiency in Mexico was 16% in children aged 2-12 years. Vitamin D plays a critical role in the formation and bone homeostasis and consequently on growth. Its deficiency is Clearly Associated With diseases: such as rickets and osteomalacia, and it has-been linked to other diseases: such as obesity, metabolic syndrome, diabetes, cancer, respiratory infections and immune system disease. Specific risk groups Have Been Described in the medical literature for deficiency in vitamin D supplementation Which May offer a benefit. Currently, there is still controversy in defining the serum levels of proficiency and dose supplementation. In Mexico, the Suggested daily intake of vitamin D is 5.6 micrograms ( 224 IU ), Which is Significantly lower than the Recommendations in the US and Europe (ie, Between 400 and 1000 IU / day).
An Increase in vitamin D deficiency Has Been Reported in recent years. There is no consensus Regarding the sufficiency levels of vitamin D. Cut-off values vary from 20 to 30 ng / ml. THEREFORE, the objective of esta review was to Provide an overview of the problem in the pediatric population and to describe the groups at risk, as well as to analyze the current Recommendations for vitamin D supplementation.
Vitamin D deficiency was rare in Mexico Considered ACCORDING to the National Institute of Medical Science and Nutrition Salvador Zubirán. Lack of evidence did not help to Establish the international recommended daily intake. Currently, vitamin D deficiency must be Recognized as a health problem, worthy of attention and action. We Suggest That prospective studies are Carried out in our country Where the relationship Between serum vitamin D deficiency and poor bone mineralization will be established.
1. Introduction
In recent years a growing interest has been reported in the metabolism and physiology of vitamin D. In addition to being an essential micronutrient, it is considered a prohormone involved in bone homeostasis. They have published several studies worldwide where an increase in the prevalence of vitamin D deficiency (defined as serum ≤20 ng / ml or 50 nmol / l), from 10 to 41.6% in population studies documented one . However, this condition remains underdiagnosed and untreated. That is why it has increased the need for national guidelines on the supplement, as well as the monitoring of serum levels of vitamin D in vulnerable population.
The objective of this review was to identify the pediatric age groups at risk for vitamin D deficiency and the consequences of this shortfall on health.
2. Physiology
Vitamin D is a group of prohormones identified from the discovery of antiraquitismo effect of cod liver oil in the early twentieth century 2 . Vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are the two main biologically inert precursors 3 and 4 . Vitamin D3 is formed from exposure of 7-dehydrocholesterol in the skin to solar B (UVB 290 to 320 nm) ultraviolet, and becomes previtamin D3. In a heat-dependent process, previtamin D3 is converted to vitamin D. Furthermore, vitamin D2 is derived from plants and exogenously produced by irradiation of ergosterol, and enters the circulation through diet 2 . In our body, both precursors (D2 and D3) suffer a first hydroxylation in the liver to become 25-hydroxyvitamin D [25 (OH) D], metabolite measured in blood for serum levels of vitamin D. 25 (OH) D requires a second hydroxylation in the kidney to become 1,25-dihydroxyvitamin D [1,25 (OH) 2D], calcitriol, the active metabolite of vitamin May .
Vitamin D plays a critical role in maintaining serum calcium and phosphorus. Without this vitamin, it would absorb only 10 to 15% of ingested dietary calcium and about 60% of phosphorus. For this reason vitamin D has a great effect on the formation and maintenance of bone 6 and 7 .
3. nutritional requirements for healthy children
In 2010, the committee of the Institute of Medicine (IOM) has updated recommendations for vitamin D intake in the general population, so the upper limit of toxicity [to maintain serum levels of vitamin D below 50 ng / ml ( 125nmol / l)] as in the definition of deficiency [20 ng / ml (40nmol / l) requirements for 97.5% of the healthy population]. Recommends maintaining serum vitamin D levels above 20 ng / ml to optimize peak bone mass, prevent bone loss and reduce the risk of osteoporotic fracture in August and September .
The IOM report provides recommendations for vitamin D intake for healthy children including referral for children over 1 year of 600 IU per day, in order to achieve serum 25-hydroxyvitamin D of 50 nmol / l. It is recognized that serum 25 (OH) D in healthy children is more identified as a marker of exposure to vitamin D as a value that can be attributed to specific health benefits. Controversy exists regarding the daily recommendation of 600 IU per day; that is, if this value meets the needs of all healthy children, especially those who remain healthy are at risk of having serum levels below 50 nmol / l. The guide is based on minimal sun exposure, indicating that sunscreen is widely used in children. In particular, guidance on the nutritional intake of 600 IU / day includes African American, Latino or those with darker skin pigmentation 1 .
According to ESPGHAN (The European Society of Paediatric Gastroenterology, Hepatology and Nutrition) of infants under one year of age should receive oral supplement of 400 IU / day under supervision of a health professional. Children and adolescents should continue with a healthy lifestyle and a diet with foods rich in vitamin D. However, children considered at risk of deficiency, those with dark skin, those who receive little sun exposure and children obesity should receive an oral supplement. ESPGHAN considered serum vitamin D levels above 50 nmol / l sufficient, and values less than 25 nmol / l classifies them as a serious deficiency 10 .
In Mexico, the suggested daily intake of vitamin D is found in the Mexican Official Standard NOM-051-SCFI / SSA1-2010, "General specifications for labeling of food and non-alcoholic beverages prepackaged commercial and health-information" 11 . In this standard a daily intake of 5.6 micrograms (224 IU) of vitamin D based on the recommendations of the National Institute of Medical Sciences and Nutrition Salvador Zubirán (INCMNSZ), which is significantly lower than the recommendations of the United States and Europe suggests , ie between 400 and 1000 IU / day. This recommendation is based on the official letter issued by the INCMNSZ in 2007, where it is said that "there are no studies that demonstrate the need for the addition of vitamin D to foods in the Mexican population. In Mexico, only isolated cases of rickets are, and calcium deficiency is not considered a public health problem; therefore there is no program to combat " 12 . Since then there have been no new recommendations issued in the country nor have formal studies documenting the average intake of vitamin D in Mexican children.
4. Vitamin D deficiency
Vitamin D deficiency is associated with rickets in children and osteomalacia in adults. Nutritional rickets is a preventable disease. Its main feature is the lack of calcium in the bones, which affects children during growth. This disease is characterized by deformities of long bones and widening of the wrists and cost-chondral joints; in infants causes delayed closure of fontanelles and craniotabes and hypotonia, seizures and hypocalcemia with heart failure 13 and 14 .
Although the prevalence of stunting had declined significantly with dietary supplements, it is now recognized that this disease has resurfaced in several countries, especially among groups with little exposure to UVB rays, infants born to mothers with low serum levels Vitamin D during pregnancy, and those breast-fed exclusively 14 .
An adequate intake of vitamin D and calcium during childhood reduces the risk of poor skeletal mineralization, loss of bone strength, reduction of peak bone mineral mass at the end of puberty and osteoporosis 15 . In the 2000s grew the scientific interest in the relationship between vitamin D deficiency and chronic diseases not skeletal, such as infections, autoimmune diseases (multiple sclerosis, rheumatoid arthritis), breast, ovary, prostate, colon and rectum, and type II diabetes mellitus, cardiovascular and metabolic diseases. However, there has been a causal link established. In the meta-analysis UMBRELLA, published in 2014, evidence it based on a systematic review from reviews and meta-analysis of observational studies and clinical trials evaluating the association between vitamin D levels and a wide range of presents diseases. The association of vitamin D concentrations with birth weight, the presence of dental caries in children, maternal vitamin D levels, the pregnancy to term and concentrations of parathyroid hormone (PTH) in chronic kidney disease was reported in patients requiring dialysis. In contrast to other studies, these findings call into question the efficacy of vitamin D as the sole measure for prevention of osteoporosis and falls. This review points out the lack of meta-analysis in relation to autoimmune diseases as well as randomized clinical trials of vitamin D supplementation in cancer, infectious diseases and cognition 16 . Some prospective studies suggest that vitamin D supplements consumed during childhood can reduce the incidence of these diseases 17 .
In Mexico there has been little research into the prevalence of vitamin D. In the few reports, serum vitamin measurements were carried out with different methods. Within these studies in the Mexican population it is of importance comment multicenter study conducted in 2008 in four representative centers of Mexico City, with 117 healthy children aged 3-8 years old, in whom serum vitamin levels were measured D by radioimmunoassay.
An overall average of 59.12 ± 12.82 nmol / l was reported.
25% of the children had deficiency and
63% failure.
Also, the National Institute of Public Health analyzed data from 1,025 children of 2-12 years of age, who participated in the 2006 ENSANUT whose vitamin D levels were determined by ELISA. An average serum 25 (OH) D3 94.6 ± 47 nmol / l was reported. Preschoolers had a higher prevalence of vitamin D (24.6%) compared with children of school age (10.2%).
Of the total sample,
16% had vitamin D deficiency (25 (OH) D3 <50 nmol / l).
23% of the children had failure (25 (OH) D3 between 50 and 75 nmol / l) 18 .
Finally, in another investigation in Mexico, in 261 children aged 5-14 years, the median concentration of 25 (OH) D was 26.13 ng / ml and PTH was 25 pg / ml. Deficiency prevalence of 25 (OH) D (<20 ng / ml) was 10% (n = 26) of failure (20-29 ng / ml) was 60.9% (n = 159) and adequacy ( > 30 ng / ml) of 29.1%. To analyze the possible risk factors for vitamin D deficiency, a significant relationship with the use of sunscreen, sun exposure and skin type was found.
5. Groups at risk for vitamin D deficiency
5.1. Preterm infants
During the last trimester of pregnancy it is when the product receives the highest contribution of minerals to the skeleton. According to studies by Widdowson and co corpses is known to calcium accretion in utero during the third quarter varies from 100 to 130 mg / kg / day, and reaches the maximum accretion between weeks 32 and 36 gestation (SDG) 19 . Because of this, preterm infants (<37 SDG) have low mineral reserves, which, coupled with its low weight (<2,250 g) and associated diseases, increases the risk of failure and lead to mineral bone metabolism . The risk of not achieving the proper development compared with reference growth charts is high 20 . It has been reported that adults with a history of prematurity have lower bone density compared to controls without history 21 . The levels of vitamin D in the mother are crucial to the mineralization of the products. According to the review by Garza et al there is evidence on the association between maternal levels of vitamin D (25 (OH) D), and bone mass newborn. Mothers with vitamin D deficiency in the last period of pregnancy had products with lower bone mineral content in products for mothers with "full" vitamin D levels (mean 1.04 kg ± 0.16 vs. 1.16 ± 0.17 kg, p = 0.002). The association between low levels of 25 (OH) D of the mother and bone mineral accretion in childhood persists up to 9 years of age 22 .
There are no population studies on the prevalence of rickets in preterm infants. Approximately 10 to 20% of newborns hospitalized low birthweight (<1,000 g) have radiographic evidence of rickets (metaphyseal changes), although the nutritional practices that are carried out 23 . This frequency is much lower as compared to the 50% incidence previously reported for this population, before fortification of human milk and the routine use of formulas for premature high mineral content 24 .
IOM recommendations relate only to supplement eutrophic children to prevent rickets associated with a deficiency of vitamin D (400 IU daily). They not considered special populations, such as newborns (RN) preterm. Preterm have unique bone mineral requirements, they can not be considered similar to those of term infants. The guidelines made in the United States limited its recommendations to term infants, so the ESPGAHN described enteral nutritional recommendations for preterm babies. ESPGHAN recommends an intake of 800 to 1,000 IU / day for preterm, with the aim of improving serum 25 (OH) D and plasma 1,25 (OH) 2D, and so subsequently rates of calcium absorption. The recommendation is the same for preterm infants breastfed to those fed with formula 25 .
According to findings published by Abrams in 2013, the routine management of preterm infants, especially those of low birth weight (<1,800 to 2,000 g), should include human milk fortified with minerals or formulas designed for preterm infants. Routine assessment of bone mineral status by biochemical methods is recommended for infants of low birth weight (<1,500 g). These tests should be performed 4-5 weeks after birth. When infants reach a weight> 1,500 g tolerate full enteral feeding, they must be supplemented with vitamin D from 400 IU / day up to 1000 IU / day 26 .
5.2. Infants exclusively breast feeding
Currently it has reported a resurgence of rickets in breastfed infants. Babies who are exclusively breast-fed and not receiving vitamin D supplementation and adequate sun exposure are at risk for vitamin D deficiency or rickets 13 . Rickets Vitamin D deficiency occurs more often in dark-skinned infants breast-fed children of mothers deficient vitamin D, and exclusive breastfeeding 27 , 28 and 29 . Preliminary studies suggest that breast-fed infants whose mothers who take supplements with high doses of vitamin D 3 , achieve levels of vitamin 25 (OH) D circulating like that infants who receive oral supplementation with vitamin D 3 30 .
The content of vitamin D in human milk depends on maternal vitamin D status A nursing woman receiving a supplement of 400 IU / day of vitamin D, have milk with vitamin D content of 25-78 IU / l 13 .
The recommendation to prevent child rickets, both in Europe and in the United States, is the supplement with 400 IU / day of vitamin D, which is equivalent to a teaspoon of cod liver oil. Fed exclusively or partially breast-infants should receive a supplement of 400 IU / day of vitamin D, beginning from the first days of life. This supplement should continue until the infant is weaned and consume at least 1 l / day of vitamin D-fortified formula or whole milk. Whole milk should not be given before the age of 12 months. For children between 12 months and 2 years of age are overweight or obese, or have a family history of obesity, dyslipidemia or cardiovascular disease, use of reduced-fat milk it is recommended 13 .
5.3. Obesity
It has been reported that obese have lower serum 25 (OH) D 31 and 32 . Although several studies have shown that skin levels of 7-dehydrocholesterol (precursor of vitamin D3) are similar in obese and non-obese subjects 33 , it is thought that subcutaneous fat (reservoir of vitamin D) kidnaps vitamin D synthesized in the skin , which results in less release of vitamin D from the skin into the circulation in obese subject as compared to non-obese subjects 34 . Children and adults with overweight and obesity have shown vitamin D deficiency Mexico, Elizondo and colleagues determined the prevalence of vitamin D deficiency and its association with obesity and lifestyle among schoolchildren in six public schools in Monterrey 35 . This study reported 61.2% failure (21 to 29 ng / ml) and 20.2% deficiency (<20 ng / ml) of a sample of 198 subjects. By stratifying the sample by body mass index (presence or absence of obesity), a significant difference was found in concentrations of 25 (OH) D between groups: obese patients had lower concentrations (23.05 ± 5.396 ng / ml) non-obese subjects (26.39 ± 6.066 ng / ml), with a mean difference of 3.34 (95% CI 1.73-4.95 p = 0.001).
In children with obesity, circulating levels of 25 (OH) D may be low, but the body reserves are not deficient. Until now it has not been proven, through clinical trials, a specific clinical benefit of dose intake of vitamin D greater than the daily recommendations for healthy children 36 .
In studies where moderate weight loss is achieved, it found an increase in circulating serum levels of 25 (OH) D, despite maintaining steady intake of vitamin D, and this increase was proportional to the loss of weight. There is no evidence of any effect on bone health, and other health conditions, a higher intake of vitamin D to the requirements suggested in people with obesity 37 .
6. diseases associated with alterations in the metabolism of vitamin D
6.1. Chronic renal failure
Among the disorders derived from chronic kidney disease (CKD) is a lower activity of the 1-alpha-hydroxylase, which leads to decreased production of calcitriol, resulting in a decreased intestinal calcium absorption and renal excretion of phosphate, with consequent hypocalcemia and hyperphosphatemia. Hypocalcemia reduces the activity of calcium-sensitive receptors in the parathyroid gland and stimulates the secretion of PTH. PTH, in response to low serum calcium and high phosphate levels, increase tubular reabsorption of calcium and phosphate secretion; likewise, it stimulates renal enzyme 1-alpha-hydroxylase to produce 1,25 (OH) 2D. However, patients with CKD are unable to produce adequate amounts of 1,25 (OH) 2D. In addition, these patients may have nutritional deficiencies from inadequate intake secondary to hypoxia and uremic dietary restriction to which they are subjected, resulting in an inadequate amount of substrates for the conversion of calcitriol 38 . This observation indicates the need to maintain surveillance of vitamin D deficiency in patients with compromised renal function, regardless of the regular replacement with calcitriol. Current guidelines of the Kidney Disease Outcomes Quality Initiative suggest measuring the levels of 25 (OH) D if serum PTH levels are above the expected range for the CKD stage II and beyond as an attempt to delay secondary hyperthyroidism and its effects 39 .
Children with kidney failure are at high risk of developing bone disorders renal osteodystrophy with concomitant vitamin D deficiency levels of vitamin D deficiency in this disease reaches a prevalence of up to 75% (serum 25 (OH) D <37.5 nmol / l) in this population 40 . Similarly, the prevalence of hyperparathyroidism in CKD is high and significant relationship between levels of PTH and 25 (OH) D, regardless of the levels of calcitriol. Optimizing the levels of vitamin D may provide an additional benefit in preventing or ameliorating hypoparathyroidism in patients with early CKD, and it is important as part of adjuvant treatment of children with CKD 41 , 42 and 43 .
Recently published multiple clinical guidelines on vitamin D supplementation in children and adults with CKD. The latest guide emphasizes the need to support the results supplement ERC and recommend correction of vitamin D deficiency using the same strategies for the general population. Observational studies in patients with CKD have linked vitamin D deficiency with mortality, insulin resistance, anemia, inflammation and progression of kidney disease 44 , 45 and 46 .
6.2. Cancer
The development of curative therapies for pediatric oncology diseases has generated a growing population of surviving children at risk for bone metabolism, since cancer treatment can interfere with attainment of peak bone mass, and potentially predispose to early onset osteopenia and osteoporosis, or more serious complications. Bone mineral deficiencies have been reported after cancer treatment, and represent a disease that can be reduced or prevented through changes in lifestyle and early diagnosis to be suspected as sequelae of cancer (such as hypogonadism) 47 .
The etiology of the deficit in bone mineral density (BMD) in pediatric cancer patients is multifactorial and includes direct and indirect effects of cancer and its treatment that result in bone loss, reduced growth and decreased bone mineral deposit. Malignant infiltration and some chemotherapeutic agents such as methotrexate and glucocorticoids can directly interfere with mineral metabolism, reducing bone mineral accretion during therapy 47 , 48 and 49 . Also inadequate nutrition and physical inactivity (Result of cancer and treatment), and some side effects of treatment, such as hypothalamic-pituitary endocrine disorders and primary hypogonadism, can cause BMD deficit.
The adverse effects of chemotherapeutic agents on bone metabolism have already been described. Alkylating agents may contribute to BMD deficit, and impaired gonadal function. Similarly, radiation may lead to osteopenia, causing alterations of the hypothalamic-pituitary gonadal axis, or dysfunction. Finally, the mineral deficit in survivors treated with hematopoietic cells may result from the treatments described and total body radiation or their drug used to maintain the grafts and prevent complications, such as graft-versus-host disease or treatment for endocrinopathies. Likewise, genetic predisposition, such as Caucasians, and lifestyle may confer an additional risk to the patient. Genetic factors are not modifiable. However, the lifestyle, such as poor secondary to surgery or low intake of calcium and vitamin D mobility can have a negative impact on bone modeling and achieve peak bone mass. Therefore, these patients may benefit from an intake of calcium and vitamin D based on the daily recommendations 50 .
In studies using dual x-ray absorption it is shown a reduction in BMD in the treatment of disease 51 . Longitudinal studies of bone mineral content in survivors of acute lymphoblastic leukemia (ALL) in pediatric patients (without receiving cranial radiation) suggest that treatment of ALL does not result in harmful long-term effects on bone development. However, the lack of a complete normalization of cortical and trabecular BMD indicates that these patients require adequate supplementation with vitamin D. Children with ALL, during and shortly after treatment, have a six times greater risk of vertebral fractures compared to controls 52 .
It is still uncertain benefit of vitamin D supplementation during chemotherapy, specifically of calcitriol, as has been reported a modest deterioration dexamethasone cytotoxicity and induction of apoptosis in human cells pre-LLA 53 .
6.3. Fat malabsorption
Vitamin D is a fat soluble vitamin which requires the presence of dietary fats in the intestine for absorption. This is why it has been documented vitamin D deficiency by some pathological conditions associated with malabsorption of fats, such as intestinal Crohn's disease, cystic fibrosis (CF), celiac disease, or partial gastric resection. CF patients suffering from exocrine pancreatic insufficiency, resulting in malabsorption of fat soluble vitamins, including vitamin D. CF patients absorb less than 50% of normal vitamin D, depending on the degree of exocrine insufficiency 54 .
6.4. Inflammatory bowel disease
Inflammatory bowel diseases (IBD), including Crohn's disease and ulcerative colitis, are multifactorial conditions characterized by inflammation of the intestine, malabsorption of nutrients and bone demineralization. Studies in vivo in animal models indicate that 1,25 (OH) 2D plays a role in the pathophysiology of experimentally induced forms of IBD. In mice, it was able to inhibit the development of IBD with this active form of vitamin D 55 . Some recent studies have involved the manipulation of aberrant innate immunity of the intestinal microbiota as an initiator of adaptive immunity damage associated with Crohn's disease 56 . It is proposed that the effect of vitamin D in this disease may involve both pathways, activation of innate immunity with suppression of adaptive immunity and inflammation associated. For 5 years it has been recognized that bone demineralization, including osteopenia and osteoporosis, it has resulted in clinically significant disease in patients 57 and 58 . Multiple studies report an incidence of over 30% of low 25 (OH) D in patients with IBD 59 and 60 . In a controlled clinical trial safety and efficacy of vitamin D repletion in patients with IBD (from 5-21 years) and serum 25 (OH) D <50 nmol / l was analyzed. In this study daily oral dose of 2,000 IU vitamin D3 and dose of 50,000 IU of vitamin D2 weekly for 6 weeks were compared, and it was found that the dose of 2,000 IU daily for 6 weeks better elevated serum levels of 25 (OH) D 60 .
6.5. Asthma
The failure and vitamin D deficiency is common in children with asthma. Many of the risk factors that have been associated with vitamin D deficiency (as are African-American ethnicity and obesity) are also associated with asthma. Brehm and colleagues reported a prevalence of 35% of serum 25 (OH) D <75 nmol / L among a sample of 1,024 children with moderate persistent asthma; likewise, it was associated an increased risk of requiring hospitalization or go to the emergency services among these children 61 .
We have studied vitamin D supplementation as a control measure risk of asthma and acute respiratory infections. In the study of Majak et al patients who received 500 IU of cholecalciferol a day for six months they had a lower risk of exacerbation of asthma triggered by an infection of the respiratory tract. These results suggest a beneficial effect of vitamin D supplementation in deficient children with asthma thereof and acute respiratory infections 62 .
6.6. Eating disorders
Within eating disorders several clinical entities, such as anorexia nervosa, bulimia nervosa, eating disorders alcoholism and other disorders not otherwise specified are grouped. The eating disorders put adolescents and young adults at risk of harm bone health. Low BMD observed in those suffering from eating disorders is caused by a fault in the accretion of peak bone mass during adolescence and bone loss during early adulthood 63 and 64 . Patients with eating disorders and bone loss may be asymptomatic or suffer from bone pain, and have a high incidence of fractures. Adolescents with eating disorders are prone to stress fractures, kyphoscoliosis, and loss of height or lack of growth 65 . Bone loss in eating disorders is often irreversible and limited treatment modalities. Bone loss in these disorders can occur within the first 12 months of the onset of the disease 66 .
Many mechanisms influence the decrease in BMD of subjects with eating disorders, including low caloric intake and malnutrition, with low serum-like factor (IGF-1) growth; low body weight and low reserves of adipose tissue, with low and high levels of leptin peptide YY; impaired thyroid function; hypogonadism, with decreased levels of sex hormones; and high levels of circulating cortisol 67 . Food restriction combined with excessive exercise in healthy women has adverse effects on bone formation and resorption 68 .
The greatest accumulation of bone mass in girls occurs between 11 and 14 years old. Environmental factors that most influence the accumulation of bone mass in adolescents are estrogen levels, exercise, body weight and nutrition. All these factors intersect in adolescents with eating disorders, amenorrhea thinness and 69 . Altering these factors and the disruption of normal physiological processes for the acquisition of bone may result in lower than expected bone mass. Body weight, adjusted for height and influenced by genetics, and environmental factors is the variable that, in isolation, more influence bone mass 69 . Thinness during adolescence leads to low bone mass in adulthood and lower bone reserves, to reach menopause with low BMD and increased risk of fractures 70 and 71 .
Minerals such as calcium, phosphorus, magnesium and vitamin D are essential nutrients for bone mineralization. Calcium metabolism is abnormal in patients with eating disorders. The bioavailability of vitamin D in patients with anorexia nervosa is similar to subjects with normal weight, and can not be any different dosing them with vitamin D 72 .
It has not been able to demonstrate the effectiveness of supplementation of calcium and vitamin D to increase BMD in anorexia nervosa 73 . However, it is recommended to optimize the intake of calcium and vitamin D. Vitamin D deficiency may exacerbate the deterioration of bone metabolism in anorexia 74 . The IOM recommends 1,300 mg / day of calcium, with a limit of 3,000 mg and vitamin D3 600 IU / day, with a limit of 4,000 IU for ages 9-18 years.
7. Drug treatments associated with vitamin D deficiency
7.1. Intensive therapy
It has reported a high prevalence (40-69%) of low vitamin D (<50 nmol / l) in critically ill children hospitalized in intensive care services. There has been a major deficiency in older children and dark skin. Found levels of vitamin D significantly reduced in patients with severe at the time of hospital admission disease. Hypocalcemia, use of catecholamines and volume bolus administration have often been associated with decreased circulating levels of vitamin D. A more serious and more days in intensive care units, are more likely to have vitamin D deficiency
There are no consensus guidelines for vitamin D supplementation in these patients. Therefore, it requires more research and a study protocol on the supplement in intensive care units, as it has been observed that children who received supplementation with vitamin D or ingested supplemented formulas with vitamin D had higher levels of concentration of 25 (OH) D 75 , 76 and 77 .
7.2. Use of anticonvulsant drugs
The long-term use of antiepileptic drugs, also called antiepileptic drugs used to treat seizures and bipolar disorder, such as phenobarbital, phenytoin and carbamazepine and the antibiotic rifampicin may cause osteomalacia 78 , 79 and 80 . Such deleterious side effect is produced by induction catabolism of 1.25 (OH) 2D.
7.3. Chronic steroid use
Steroids exert their effect on bone through multiple pathways, including a decrease in osteoblast activity, increased bone resorption, interfering with the growth hormone-IGF axis-1, reduced muscle strength and altering the balance of calcium intestinal and renal level 81 . Children and adolescents who are exposed to high doses of steroids (equivalent to 900 mg / m dose 2 prednisone), are at greater risk of decreased bone density, and at the end of treatment will not be possible to restore normal This 48 . Thus, the use of more potent glucocorticoids, such as dexamethasone, has been associated with a high incidence of fractures and BMD deficit 82 .
8. Monitoring supplement with vitamin D
Despite the supplement with 400 IU / day, children with vitamin D deficiency can continue with this deficiency as they may require higher doses of vitamin D to maintain normal levels. In these children the circulating levels of vitamin D should be determined by laboratory tests (serum 25 (OH) D, PTH levels and bone mineral status determination). If vitamin D supplementation starts, serum levels should be monitored every 3 months until normal levels are reached. The bone mineral status and PTH levels can be monitored every 6 months until they return to normal.
9. Conclusions
Childhood and adolescence are critical periods for the development of a healthy skeleton; however, these periods of life many morbid conditions, including vitamin D deficiency there is important that clinicians recognize that there are populations where it should recommend a universal supplement populations such as newborns and preterm infants children breast-fed exclusively.
It has reported an increase in vitamin D deficiency in recent years. There is no consensus regarding the levels of vitamin D sufficiency, plus cutoff values ranging from 20 to 30 ng / ml. The recommendations of dietary intake in the international literature have been adjusted to between 400-1,000 IU, depending on age group. Vitamin D deficiency has been considered rare in Mexico, and the lack of evidence did not allow to establish the recommended daily intake according to the considerations of the National Institute of Medical Sciences and Nutrition Salvador Zubirán. Today, however, must be recognized as a health problem, worthy of attention and action. It is suggested that prospective studies in Mexico, where the relationship between serum vitamin D deficiency and poor bone mineralization is established are carried out.
Conflict of interests
The authors declare no conflict of interest.
References (in English) in PDF
