Vitamin D once during pregnancy reduced infant health care costs (300 times ROI) – RCT
Effects of Pre-Natal Vitamin D Supplementation with Partial Correction of Vitamin D Deficiency on Early Life Healthcare Utilisation: A Randomised Controlled Trial.
PLoS One. 2015 Dec 23;10(12):e0145303. doi: 10.1371/journal.pone.0145303. eCollection 2015.
 Extensive detail on health care costs. Costs are in UK ~0163~
ROI = Return on Investment
Cost differences were not statistically significant after “correcting” for ethnicity
Note: They “corrected” for lower levels of vitamin D in darker skinned women
Probably far more cost effective (>1000 times?) if gave periodic doses to mother AND infant
See also VitaminDWiki
* Pregnancy helped by single dose of 60,000 IU of Vitamin D – RCT March 2015
* 18 fewer hospital days if given 500,000 IU of vitamin D while ventilated in ICU – RCT June 2016
* Vitamin D supplementation of all pregnant women (in UK) would be cost effective – just considering preeclampsia – March 2016
* Heart Attack ICU costs reduced $37,000 by $20 of Vitamin D – Nov 2015
* Cost savings with Vitamin D **category listing has items along with related searches**
Pregnancy category starts with
{include}
- - - - - - - - - -
Healthy pregnancies need lots of vitamin D has the following summary
{include}
Extensive detail on health care costs. Costs are in UK ~0163~
ROI = Return on Investment
Cost differences were not statistically significant after “correcting” for ethnicity
Note: They “corrected” for lower levels of vitamin D in darker skinned women
Probably far more cost effective (>1000 times?) if gave periodic doses to mother AND infant
See also VitaminDWiki
* Pregnancy helped by single dose of 60,000 IU of Vitamin D – RCT March 2015
* 18 fewer hospital days if given 500,000 IU of vitamin D while ventilated in ICU – RCT June 2016
* Vitamin D supplementation of all pregnant women (in UK) would be cost effective – just considering preeclampsia – March 2016
* Heart Attack ICU costs reduced $37,000 by $20 of Vitamin D – Nov 2015
* Cost savings with Vitamin D **category listing has items along with related searches**
Pregnancy category starts with
{include}
- - - - - - - - - -
Healthy pregnancies need lots of vitamin D has the following summary
{include}
Griffiths M1, Goldring S1, Griffiths C2, Shaheen SO2, Martineau A2, Cross L2, Robinson S3, Warner JO1, Devine A2, Boyle RJ1.
1Department of Paediatrics, Imperial College London, London, United Kingdom.
2Centre for Primary Care and Public Health, Blizard Institute, Queen Mary University of London, London, United Kingdom.
3Department of Endocrinology, Imperial College London, London, United Kingdom.
📄 Download the PDF from VitaminDWiki
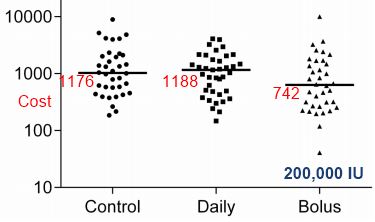
A portion of Table 6
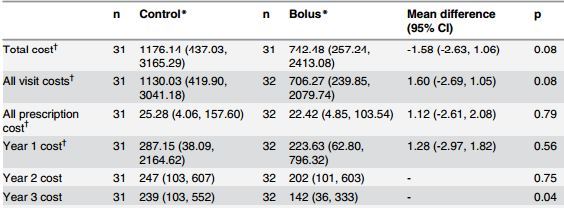
(40% lower cost. 40% fewer office visits)
BACKGROUND:
Some observational studies have suggested that higher prenatal Vitamin D intake may be associated with improved health outcomes in childhood. However there have been mixed results in this area with some negative studies, especially for effects on atopic and respiratory outcomes. We examined the effect of prenatal Vitamin D on healthcare utilisation in the first three years of life.
METHODS:
In an ethnically stratified randomised controlled trial conducted at St Mary's Hospital London, 180 women at 27 weeks gestation were allocated to no Vitamin D, 800 IU ergocalciferol daily until delivery, or a single oral bolus of 200,000 IU cholecalciferol. Participants were randomised in blocks of 15 using computer-generated numbers and investigators were blinded to group assignment. Supplementation increased maternal and cord blood 25(OH) vitamin D concentrations, but levels remained lower than current recommendations. Primary health economic outcome was overall cost of unscheduled healthcare utilisation in the first three years of life as documented in the child's electronic health record. Secondary outcomes included cost attributable to: primary and secondary healthcare visits, respiratory and atopic complaints, cost in years 1, 2 and 3 of life and cost and frequency of prescribed medication. All costs were calculated as pounds sterling. Differences between groups were analysed using unpaired t-test or Mann-Whitney U test, and analysis of variance for adjusted analyses.
RESULTS:
We assessed 99/180 (55%) complete electronic health records, control (n = 31), daily (n = 36) and bolus (n = 32). We found no difference in total healthcare utilisation costs between the control and daily (mean difference in costs in pounds sterling 1.02, 95%CI -1.60, 1.65; adjusted 1.07, 95%CI -1.62, 1.86) or control and bolus groups (mean difference -1.58, 95%CI -2.63, 1.06; adjusted -1.40, 95%CI -2.45, 1.24). There were no adverse effects of supplementation reported during the trial.
CONCLUSIONS:
We found no evidence that prenatal vitamin D supplementation from 27 weeks gestation to delivery, at doses which failed to completely correct maternal vitamin D deficiency, influence overall healthcare utilisation in children in the first 3 years.
TRIAL REGISTRATION: Controlled-Trials.com ISRCTN68645785.
PMID: 26698303 PMCID: PMC4689556 DOI: 10.1371/journal.pone.0145303
