Digestive tract cancer death rates reduced a bit by a bit of vitamin D – RCT
Effect of Vitamin D Supplementation on Relapse-Free Survival Among Patients With Digestive Tract Cancers – The AMATERASU Randomized Clinical Trial
JAMA. 2019;321(14):1361-1369. doi:10.1001/jama.2019.2210
Mitsuyoshi Urashima, MD1; Hironori Ohdaira, MD2; Taisuke Akutsu, MD1; et al Shinya Okada, MD3; Masashi Yoshida, MD2; Masaki Kitajima, MD2; Yutaka Suzuki, MD2
 Other
* Chemotheraphy not work as well with low Vitamin D (colon cancer this time) – Aug 2018
* Esophageal Cancer 40 percent less likely in parts of UK with more sun (vitamin D) – Feb 2018
* Gastric Cancer 8.8 times more likely if low vitamin D – Sept 2016
* Chemotherapy (cisplatin) and vitamin D synergistically stop stomach cancer – Feb 2014
* Advanced Colorectal Cancer survival is increased somewhat with 4,000 IU of vitamin D – RCT April 2019
* In the same JAMA issue as the study on this page
Cancer category starts with the following
{include}
---
1. Vitamin D Receptor and Cancers
1. Items in both categories Vitamin D Receptor and Cancer - Colon:
{category}
1. Items in both categories Vitamin D Receptor and Cancer
{category}
1. Items in both categories Vitamin D Receptor and Cancer - other:
{category}
Other
* Chemotheraphy not work as well with low Vitamin D (colon cancer this time) – Aug 2018
* Esophageal Cancer 40 percent less likely in parts of UK with more sun (vitamin D) – Feb 2018
* Gastric Cancer 8.8 times more likely if low vitamin D – Sept 2016
* Chemotherapy (cisplatin) and vitamin D synergistically stop stomach cancer – Feb 2014
* Advanced Colorectal Cancer survival is increased somewhat with 4,000 IU of vitamin D – RCT April 2019
* In the same JAMA issue as the study on this page
Cancer category starts with the following
{include}
---
1. Vitamin D Receptor and Cancers
1. Items in both categories Vitamin D Receptor and Cancer - Colon:
{category}
1. Items in both categories Vitamin D Receptor and Cancer
{category}
1. Items in both categories Vitamin D Receptor and Cancer - other:
{category}
📄 Download the PDF from Sci-Hub via VitaminDWiki
Key Points
Question Does vitamin D supplementation improve survival among patients with digestive tract cancers?
Findings In this randomized clinical trial that included 417 patients with digestive tract cancers (from esophagus to rectum), the 5-year relapse-free survival rate for those randomized to vitamin D, 2000 IU/d, vs placebo was 77% vs 69%, a difference that was not statistically significant
Meaning Vitamin D supplementation did not improve relapse-free survival among patients with digestive tract cancer.
Importance Randomized clinical trials of vitamin D supplementation for secondary prevention in patients with cancer are needed, given positive results of observational studies.
Objective To determine whether postoperative vitamin D3 supplementation can improve survival of patients with digestive tract cancers overall and in subgroups stratified by 25-hydroxyvitamin D (25[OH]D) levels.
Design, Setting, and Participants The AMATERASU trial, a randomized, double-blind, placebo-controlled trial conducted at a single university hospital in Japan. Enrollment began in January 2010 and follow-up was completed in February 2018. Patients aged 30 to 90 years with cancers of the digestive tract from the esophagus to the rectum, stages I to III, were recruited. Of 439 eligible patients, 15 declined and 7 were excluded after operation.
Interventions Patients were randomized to receive oral supplemental capsules of vitamin D (2000 IU/d; n = 251) or placebo (n = 166) from the first postoperative outpatient visit to until the end of the trial.
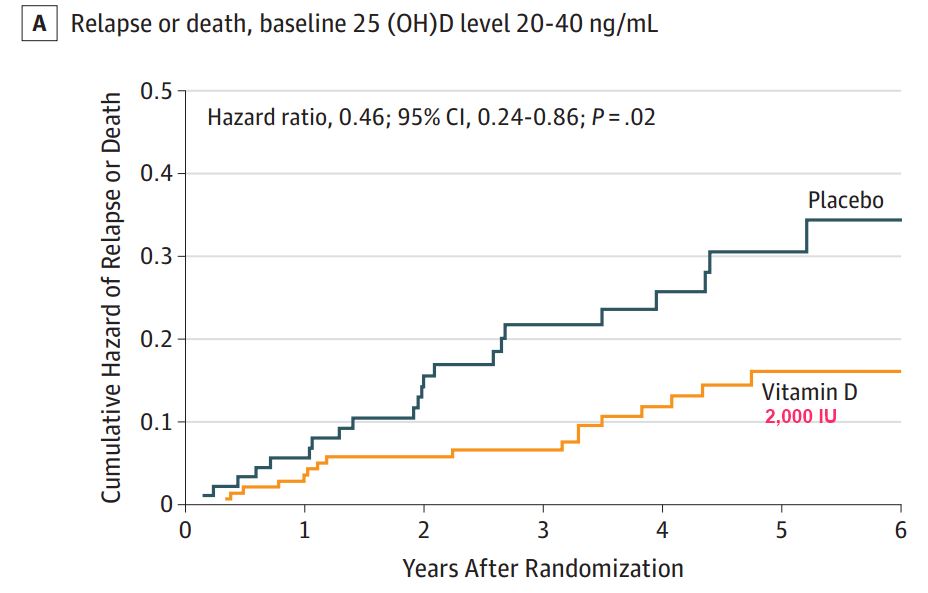
Main Outcomes and Measures The primary outcome was relapse-free survival time to relapse or death. The secondary outcome was overall survival time to death due to any cause. Subgroups analyzed had baseline serum 25(OH)D levels of 0 to less than 20 ng/mL, 20 to 40 ng/mL, and greater than 40 ng/mL; because of small sample size for the highest-baseline-level group, interactions were tested only between the low- and middle-baseline-level groups.
Results All 417 randomized patients (mean age, 66 years; male, 66%; esophageal cancer, 10%; gastric cancer, 42%; colorectal cancer, 48%) were included in the analyses. There was 99.8% follow-up over a median 3.5 (interquartile range, 2.3-5.3) years, with maximal follow-up of 7.6 years. Relapse or death occurred in 50 patients (20%) randomized to vitamin D and 43 patients (26%) randomized to placebo. Death occurred in 37 (15%) in the vitamin D group and 25 (15%) in the placebo group. The 5-year relapse-free survival was 77% with vitamin D vs 69% with placebo (hazard ratio [HR] for relapse or death, 0.76; 95% CI, 0.50-1.14; P = .18). The 5-year overall survival in the vitamin D vs placebo groups was 82% vs 81% (HR for death, 0.95; 95% CI, 0.57-1.57; P = .83). In the subgroup of patients with baseline serum 25(OH)D levels between 20 and 40 ng/mL, the 5-year relapse-free survival was 85% with vitamin D vs 71% with placebo (HR for relapse or death, 0.46; 95% CI, 0.24-0.86; P = .02; P = .04 for interaction). Fractures occurred in 3 patients (1.3%) in the vitamin D group and 5 (3.4%) in the placebo group. Urinary stones occurred in 2 patients (0.9%) in the vitamin D group and 0 in the placebo group.
Conclusions and Relevance Among patients with digestive tract cancer, vitamin D supplementation, compared with placebo, did not result in significant improvement in relapse-free survival at 5 years.
