Masterjohn on relationships between Vitamin A D and K
Is Vitamin D Safe? Still Depends on Vitamins A and K! Testimonials and a Human Study
Christopher Masterjohn in WAPF Blog on 12/15/10
In the last several weeks, two momentous occasions have occurred in the world of vitamin D.
First, the Institute of Medicine (IOM) released its new report. It tripled the recommended intakes, doubled the upper limit, and commissioned researchers to go forth and test the effects of intakes higher than the upper limit, as this would be safe under proper supervision and provide valuable information.
This sucker is 999 pages long. When I finish reading it, you can look forward to one heck of a blog post on the matter. Stay tuned, folks.
The second momentous occasion occurred two days ago (Tuesday, December 14, 2010) when bestselling business author and tango champion Tim Ferriss released The 4-Hour Body. Tim's last book, The 4-Hour Workweek, was number one on the New York Times, Business Week, and Wall Street Journal bestseller lists and has been translated thus far into 35 languages.
In his new book, he discusses my research on the interactions between vitamins A, D, and K, and gives the following warning:
Supplemental vitamin D increases your need for vitamin A, so don't forget the aforementioned cod liver, which includes both.
Hooray! It's wonderful to see someone with this type of reach get this information out there.
I first raised the issue of vitamin A-and-D interactions in the spring of 2006 in my article on vitamin A and osteoporosis. I developed these thoughts further and introduced their interactions with vitamin K in the fall of 2006 in my article, From Seafood to Sunshine: A New Understanding of Vitamin D Safety, and in the spring of 2007 in my article, On the Trail of the Elusive X Factor: A 62-Year Mystery Finally Solved, Vitamin K2 Revealed.
I formally published my hypothesis that vitamin D toxicity results not so much from hypercalcemia but moreso from causing the excessive production of vitamin K-dependent proteins, leading to defective forms of these proteins in the absence of adequate vitamin K, in my December, 2007 Medical Hypotheses paper, Vitamin D Toxicity Redefined: Vitamin K and the Molecular Mechanism. Tufts University researchers confirmed the first prediction of this hypothesis the following year, showing that when vitamin A protects against vitamin D toxicity, it curbs the excessive production of vitamin K-dependent proteins.
When I wrote these articles, all the most compelling research I had was from animal studies. I wish that when I wrote them I had known that proof of principle for vitamin A-and-D interactions had already been experimentally demonstrated in humans. This revelation, however, had to wait for my 2009 Wise Traditions lecture, Cod Liver Oil: Our Number One Superfood. (You can get the DVD here).
In 1941, Irwin G. Spiesman published a human trial in the Archives of Otolaryngology, a journal published by the American Medical Association, Massive Doses of Vitamins A and D in the Prevention of the Common Cold.
Spiesman treated 54 individuals who suffered from frequent colds (five to seven colds per winter) with massive doses of either vitamin A alone, vitamin D alone, or vitamins A and D together. He treated them during the winter, for as many as three years, with a dosing schedule reaching a maximum of 40,000 IU for vitamin A and 300,000 IU for vitamin D.
Spiesman found that vitamins A and D only reduced colds when fed together:
Vitamins A and D Only Prevent Colds When Supplied Together
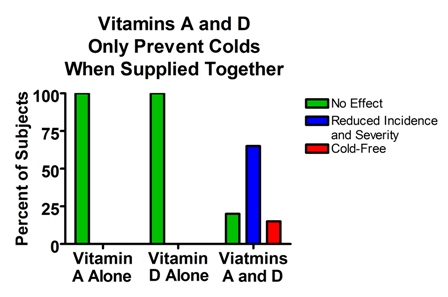
Likewise, he found that vitamins A and D were only safe when provided together:
Vitamins A and D are toxic when provided alone, but safe when provided together.
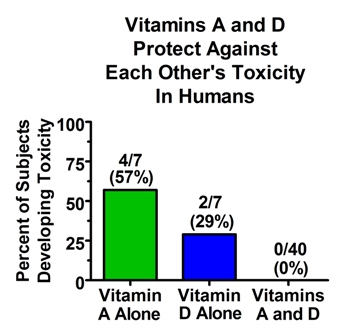
This study is not perfect. As you can see from the numbers on top of the bars in the second graph, there were far fewer people in the groups receiving either vitamin alone than in the group receiving both vitamins together. Spiesman reported that this was because it was difficult to get people receiving no benefit to continue the study for very long. It makes the study more difficult to interpret. On the other hand, given the toxicity figures in the second graph, we can be happy for safety's sake that so few people were given massive doses of one or the other vitamin alone.
It would also have been better to have had a vitamin-free control group. And it would have been better to see the effects of more realistic doses of vitamins.
Nevertheless, the study quite clearly provides proof of principle in humans that vitamins A and D are most beneficial and safest when provided together, just like in the animal experiments.
Several commenters on this blog and on my Facebook Fan Page have provided testimonials about their negative experiences with vitamin D supplementation that support the protective effects of vitamins A and K:
Cynthia Frederick, March 2010 I, and many others I've met on forums, have adverse reactions to Vit D3, even the lower amounts of 2,000 IU/day and even though we were tested and were deficient. And we do not have the conditions that would make Vit D contraindicated. . . . I'm waiting for the long-term effects to take place in people taking these higher amounts who are not simultaneously increasing their Vit A and K levels. In 10 years I wager we will be hearing about the negative effects that the higher doses of this 'miracle nutrient' have had on those taking it. . . [in a later comment] As I mentioned before, there seems to be a subset of us for whom even low doses (1,000 IU/day) of Vit D cause kidney stones, chest pain, fatigue, and aches and pains, even though our 25 OH D levels were 'low' (23). We get these symptoms as soon as a week after using the D. . . . I saved myself a trip to the ER with the above symptoms by remembering previous articles of yours about balancing the fat-soluble vitamins, and took about 100,000 IU of Vit A from fish oil and 5 mg of K2. Within 1/2 hour ALL the symptoms disappeared. This happened more than once so I know it is not coincidence. You are definitely on to something here.
Lynn Razaitis, June 2010 I certainly know what happens when you get these ratios off. I naively had a vitamin D shot of 200,000 units after a serious viral infection that used up my vit A. I wrecked my kidneys, thyroid and who knows what else. It took 6 months and Chris's articles to figure out what the heck was going on with me. Within weeks of getting my vit A up with cod liver oil and a ton of liver (and I was thyroid blood testing monthly so I had test results to compare) my thyroid hormones all normalized. It was fairly stunning.
Andrea Schüler, June 2010 I stopped taking D3 because I developed tendonitis, bursitis, tendon calcification and aches and pains. I brought my level from 20 to 50 in the 25 OH test but maybe the 2000 - 4000 IU daily was not good for me or I have not enough A and K. I will test again to see where my levels are after several months without D3 pills. Maybe I should check Vit. A and K levels too. ^
I have received a number of other testimonials by email from people who have developed problems such as kidney stones and bladder stones after supplementing with "safe" amounts of vitamin D — within the IOM's new upper limit — and these symptoms quite readily develop in animals fed vitamin D with no vitamin A under experimental conditions. I have not shared these because they were sent to me in private. If you have such a testimonial and are willing to share it publicly, please post it in the comments section.
If you are a blogger or a practitioner and have commenters or patients willing to share these stories, please help me compile them into a single source by posting them here or contacting me privately.
So how much do we need of each of these vitamins and in what ratio? I do not know. We do not even know what the ideal vitamin D level is, and all of the vitamin D studies are confounded by their failure to account for the status of vitamins A and K.
Dr. Robert Heaney apparently knows what the ideal vitamin D level is:
Finally, I believe that the presumption of adequacy should rest with vitamin D intakes needed to achieve the serum 25(OH)D values (i.e., 40–60 ng/mL) that prevailed during the evolution of human physiology. Correspondingly, the burden of proof should fall on those maintaining that there is no preventable disease or dysfunction at lower levels. The IOM has not met that standard.^
If I had access to Dr. Heaney's time machine, I would love to replicate this study. All my requests for NIH funding for a time machine have been denied without any reviewer comments on how to improve my proposal. If we cannot measure paleolithic man's 25(OH)D, perhaps we can study the fossils that his clothing has left behind, or study the residue that the melanin in his skin has left on his bones, or inspect these bones for the fossilized remains of light-absorbing coconut polyphenols from the coconut oil he may have rubbed into his skin.
But alas, I know of no studies that have quantified the decay rate of melanin or coconut polyphenols over a timescale of thousands of years, or determined the effects that sun spots, lunar cycles, planetary arrangements, and innumerable possible climate changes might have on these decay rates.
Dr. Michael Holick has a more conservative opinion. He believes that 25(OH)D should be at least 30 ng/mL. I believe there is more scientific backing for this level, which I've expressed in my post, "Are Some People Pushing Their Vitamin D Levels Too High?"
But that doesn't mean we have scientific evidence that higher levels aren't better, or that they wouldn't be if people were getting enough vitamins A and K. I don't see any reason to believe that this is the case, since vitamin A seems to increase the turnover and utilization of vitamin D, which should produce a "low" level despite "high" status, but this is currently in the stage of hypothesis and guesswork.
Stephan Guyenet recently commented that it would be nice to know what the vitamin D levels of Kitavans and members of other traditional, healthy groups are:
I don't know what their 25(OH)D3 status is, but I wish I did. I'd love to know what their 1,25(OH)D3 levels look like too. I agree that it's important to have a baseline for comparison so that we can decide what's biologically normal. I've been looking for data to answer that question but I haven't found it yet.
Knowing this would help, but there is still the question of the optimal A-to-D ratio, and how this might further be affected by vitamin K status.
A paper that Dr. Holick recently co-authored suggested that ratios between four and eight may be ideal. The lead author, Dr. Linda Linday, had used cod liver oil with a ratio within this range to successfully protect against upper respiratory tract infections. These authors also cited research showing this range of ratios to be ideal in chickens. They also cited Sally Fallon's summary of my A-and-D interaction work as evidence that there was growing concern among the public about the proper ratio of A and D.
Their findings about cod liver oil are somewhat convincing, but they can't account for the vitamin D the subjects were getting from the sun, and they didn't test different ratios. The chicken research is more rigorous, but it's, well, it's in chickens.
From an evolutionary perspective, the usefulness of data from chickens depends on whether you believe the evolutionary trees (or bushes, if you prefer) derived from morphology, which place birds as closer to crocodiles than to mammals by 65 million years, or the evolutionary tree/bushes derived from molecular biology, which place birds with mammals and not with crocodiles. (See this review.) Or perhaps we should consider binding proteins and enzymatic pathways directly related to vitamin D metabolism. With respect to D2 versus D3, for example, primates are much more similar to birds than to rats. (See this review).
Ah, the mired network of divergent and convergent evolution. Perhaps we should follow Setphan's ingenius idea of studying humans. Living ones.
Paul Jaminet of Perfect Health Diet (here, down a few comments) suggests the ideal amounts are 10,000 IU A and 4,000 IU D. This also sounds quite plausible to me, but again, we can't say it's more than a semi-educated guess.
This brings us back to Tim Ferris. Ferriss tripled his testosterone by bringing his 25(OH)D up to 50 ng/mL and by following a number of other parts of his testosterone-boosting protocol including getting vitamin A from cod liver oil and eating plenty of vitamin K-rich foods. Ferriss didn't conduct a dose-finding study on himself, and there's just about zero reason to believe that the ideal level in Ferriss is going to be the ideal level in anyone else, except that we know that Ferriss is human and will therefore fall within the distribution of human requirements instead of outside of it.
But "follow me and do what I do" is not the point of his book. The point of his book is to advocate self-experimentation and to provide a starting point for each individual from among his massive audience based on his own self-experimentation.
We should still do the science, but it's going to take a long time, folks. The best thing to do now is to eat a well rounded whole foods diet and experiment with the levels of cod liver oil and/or vitamin D supplementation that make you feel the best, resolve your symptoms, increse your performance, and normalize your clinical tests if they're out of whack or don't throw them out of whack if they're normal.
And share your results with the rest of us!
See also at VitaminDWiki
Vitamin D and Vitamin K for bones and heart - LEF Sept 2010 PDF
Price and Masterjohn on Vitamin A Vitamin D and Vitamin K – 2010
Response by Masterjohn on vitamin A thwarting vitamin D – Mar 2010
Vitamin A may thwart the ability of vitamin D to reduce risk of osteoporosis – June 2010
Search for Masterjohn in VitaminDWiki 324 items as of July 2020
Interactions of Vitamins D, A, and K, should measure calcitriol, calcification – Masterjohn Aug 2013
Synergism between Vitamin D, Vitamin K-2, and Vitamin A: Masterjohn – Sept 2013
