With just 200 IU vitamin D in intravenous feeds, deficiency results
It seems incredible that the Vitamin D levels in IVs has not increased in many many decades.
See also VitaminDWiki
Use Google to search VitaminDWiki for intravenous 1440 items as of May 2017
Importance of Magnesium - which can be provided intravenously
Injection category listing has items along with related searches
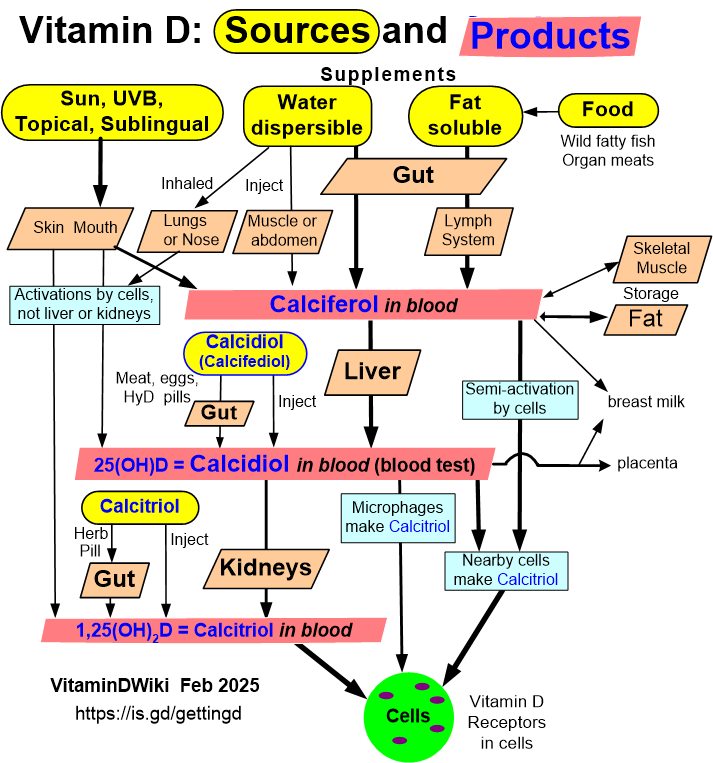
Getting Vitamin D into your blood and cells has the following chart
Recommendations for Changes in Commercially Available Parenteral Multivitamin and Multi–Trace Element Products
A.S.P.E.N. Position Paper
Nutr Clin Pract August 2012 vol. 27 no. 4 440-491
Vincent W. Vanek, MD, FACS, FASPEN (Chair)1
Peggy Borum, PhD, FASPEN2
Alan Buchman, MD, MSPH, FACP, FACG, FACN, AGAF3
Theresa A. Fessler, MS, RD, CNSC4
Lyn Howard, MB, FRCP5
Khursheed Jeejeebhoy, MBBS, PhD, FRCPC6
Marty Kochevar, MS, RPh, BCNSP7
Alan Shenkin, MB, ChB, PhD, FRCP, FRCPath8
Christina J. Valentine, MD, MS, RD9
Novel Nutrient Task Force, Parenteral Multi-Vitamin and Multi–Trace Element Working Group
American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Board of Directors
1 St. Elizabeth Health Center, Youngstown, Ohio
2 University of Florida, Gainesville, Florida
3 Northwestern University School of Medicine, Chicago, Illinois
4 University of Virginia, Charlottesville, Virginia
5 Albany Medical College, Albany, New York
6 Polyclinic, Toronto, Ontario
7 A.S.P.E.N., Silver Spring, Maryland
8 Royal Liverpool University Hospital, Liverpool, England
9 University of Cincinnati, Cincinnati, Ohio
Vincent W. Vanek, St. Elizabeth Health Center, 1044 Belmont Ave, PO Box 1790, Youngstown, OH 44501-1790; e-mail: vince_vanek@hmis.org.
The parenteral multivitamin preparations that are commercially available in the United States (U.S.) meet the requirements for most patients who receive parenteral nutrition (PN).
However, a separate parenteral vitamin D preparation (cholecalciferol or ergocalciferol) should be made available for treatment of patients with vitamin D deficiency unresponsive to oral vitamin D supplementation.
Carnitine is commercially available and should be routinely added to neonatal PN formulations.
Choline should also be routinely added to adult and pediatric PN formulations; however, a commercially available parenteral product needs to be developed.
The parenteral multi–trace element (TE) preparations that are commercially available in the U.S. require significant modifications. Single-entity trace element products can be used to meet individual patient needs when the multiple-element products are inappropriate (see Summary/A.S.P.E.N. Recommendations section for details of these proposed modifications).
PDF is attached at the bottom of this page
From the PDF: Current intravenous feeding
Only 200 IU of vitamin D, and it might be Vitamin D2, the PDF does not indicate
No Vitamin K2 – apparently just vitamin K1
No Magnesium
No Calcium – perhaps cannot make into a liquid
No Boron – perhaps cannot make into a liquid
No Silcon – perhaps cannot make into a liquid
Vitamin D deficiency in patients receiving home parenteral nutrition.
JPEN J Parenter Enteral Nutr. 2011 Jul;35(4):499-504. doi: 10.1177/0148607110381269. Epub 2011 May 3.
Thomson P, Duerksen DR.
Hospital, Winnipeg, Manitoba, Canada. duerksn@cc.umanitoba.ca
BACKGROUND:
In addition to its role in bone metabolism, vitamin D has important immunomodulatory and antineoplastic effects. Patients on home parenteral nutrition (HPN) receive most of their vitamin D from intravenous (IV) supplementation. Vitamin D deficiency is common in the general population, and the adequacy of vitamin D supplementation in HPN patients is unclear. The purpose of this study is to determine the vitamin D status of patients on HPN.
METHODS:
Consecutive patients seen in a regional home nutrition program had their oral and IV vitamin D intakes determined. Plasma 25-hydroxyvitamin D levels were measured in all patients. Intake of calcium, magnesium, and phosphate were also determined.
RESULTS:
The mean 25-hydroxyvitamin D level in 22 patients receiving HPN for a mean of 33.5 months (range, 1-177) was 42 nmol/L. Vitamin D deficiency was present in 15 (68%) patients and vitamin D insufficiency in 6 (27%) patients. The mean dietary vitamin D intake was 79.5 IU per day, while the mean IV supplementation was 166 IU per day.
CONCLUSIONS:
In this study of a regional Canadian HPN program, there was a high prevalence of vitamin D deficiency/insufficiency affecting virtually all patients. All patients receiving HPN should be supplemented with vitamin D and have their 25-hydroxyvitamin D levels monitored. Further studies are required to determine optimal methods and dosing of vitamin D replacement using oral supplements or ultraviolet light therapy.
PMID: 21540352 FULL TEXT online
Vitamin D Deficiency and Low Bone Mineral Density in Pediatric and Young Adult Intestinal Failure.
J Pediatr Gastroenterol Nutr. 2013 May 20.
Ubesie AC, Heubi JE, Kocoshis SA, Henderson CJ, Mezoff AG, Rao MB, Cole CR.
Division of Gastroenterology, Hepatology and Nutrition, Cincinnati Children Hospital Medical Center, Cincinnati, Ohio, USA †Department of Paediatrics, University of Nigeria Teaching Hospital, Ituku/Ozalla, Enugu, Nigeria ‡Department of Biostatistics, University of Cincinnati, Ohio, USA.
OBJECTIVES: To determine the prevalence and predisposing factors for vitamin D deficiency and low bone mineral density (BMD) in patients with intestinal failure (IF). METHODS: A retrospective review of patients with IF managed at the Cincinnati Children's Hospital Medical Center. IF was defined as history of parenteral nutrition (PN) >30 days. Vitamin D deficiency was defined as serum 25-OH vitamin D [25(OH) D] <20 ng/dL. Reduced bone mineral density (BMD) was defined using dual x-ray absorptiometry (DXA) Z-score ≤ - 2. A binary logistic regression model was used to test for association of significant risk factors and the outcome variables after univariate analyses. RESULTS: One hundred and twenty three patients with median age of 4 years (range 3-22 years) were evaluated. Forty-nine (39.8%) patients had at least a documented serum 25 (OH) D deficiency during the study interval while 10 out of 80 patients (12.5%) with DXA scans done had a low BMD Z-score. Age at study entry was associated with both 25 (OH) D deficiency (P = 0. 01) and low BMD Z-score (P = 0. 03). Exclusive PN at study entry was associated with reduced bone mass (P = 0.03). There was no significant association between vitamin D deficiency and low BMD Z-score (P = 0.31). CONCLUSION: The risk of 25 (OH) D deficiency and low BMD Z-score increases with age among patients with IF. Strategies for monitoring and preventing abnormal bone health in older children receiving exclusive PN need to be developed and evaluated.
PMID: 23698025
