Before joint replacement surgery low Vitamin D associated with systemic disease
High prevalence and seasonal variation of hypovitaminosis D in patients scheduled for lower extremity total joint arthroplasty.
Ann Transl Med. 2018 Aug;6(16):321. doi: 10.21037/atm.2018.08.21.
Piuzzi NS1,2, George J1, Khlopas A1, Klika AK1, Mont MA1,3, Muschler GF1, Higuera CA4.
1 Department of Orthopedic Surgery, Cleveland Clinic, Cleveland, OH, USA.
2 Instituto Universitario del Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
3 Department of Orthopaedic Surgery, Lenox Hill Hospital, New York, NY, USA.
4 Department of Orthopaedic Surgery, Cleveland Clinic, Weston, FL, USA.
 ASA score (from the web))
ASA score (from the web))
 ---
1. Trauma and surgery category starts with the following
{include}
---
* Fewer Complications Following Revision Hip and Knee Arthroplasty in Patients with Normal Vitamin D Levels – March 2017
* 4 fewer days in hospital after hip or knee replacement if good level of vitamin D – June 2016
* Knee surgery reduced vitamin D by 40 percent in 2 days – May 2011
* Better total hip replacement if have high vitamin D
* Vitamin D and exercise after hip fracture surgery – far fewer deaths – July 2016
* Improve your health BEFORE surgery (prehabilitation) helps your recovery - 2018
* Should Improve your health AND Vitamin D BEFORE many surgeries
---
1. Trauma and surgery category starts with the following
{include}
---
* Fewer Complications Following Revision Hip and Knee Arthroplasty in Patients with Normal Vitamin D Levels – March 2017
* 4 fewer days in hospital after hip or knee replacement if good level of vitamin D – June 2016
* Knee surgery reduced vitamin D by 40 percent in 2 days – May 2011
* Better total hip replacement if have high vitamin D
* Vitamin D and exercise after hip fracture surgery – far fewer deaths – July 2016
* Improve your health BEFORE surgery (prehabilitation) helps your recovery - 2018
* Should Improve your health AND Vitamin D BEFORE many surgeries
📄 Download the PDF from VitaminDWiki

BACKGROUND:
High rates of vitamin D insufficiency and deficiency have been demonstrated in various patient populations, including patients undergoing total joint arthroplasties (TJA). However, the risk factors associated with this condition and its seasonal variation is still to be determined in patients scheduled for elective TJA.
METHODS:
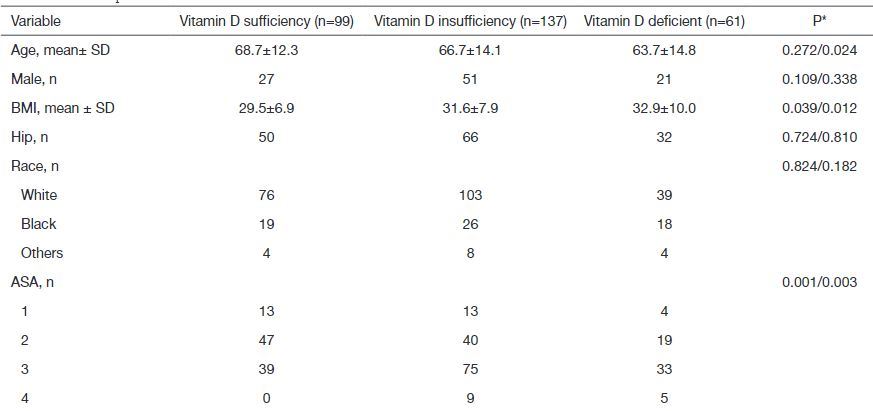
We retrospectively identified 226 (116 hips, 120 knees) patients who underwent primary TJA, and had a vitamin D measurement, at a single institution (latitude, 41° 30' N) from 2006 to 2016. Demographics, comorbidities, and perioperative data were collected from electronic medical records. Patients were stratified into vitamin D sufficient (≥30 ng/mL), insufficient (<30 ng/mL), and deficient group (<20 ng/mL). Multivariate regression analyses were used to study the risk factors for vitamin D insufficiency and deficiency.
RESULTS:
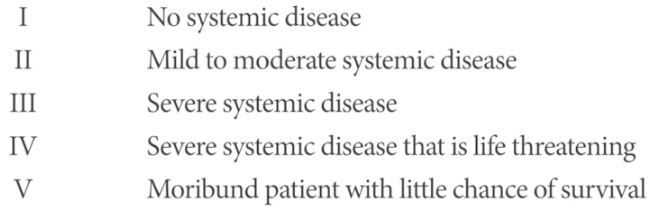
There were 99/226 (43.8%) patients in the vitamin D sufficient group, 137/226 patients (60.6%) in the insufficient group, of which 61/226 (26.9%) were in the deficient group. On multivariate analysis, an American Society of Anesthesiologists' (ASA) score ≥3 was a risk factor for vitamin D insufficiency (P<0.001), while ASA ≥3 (P<0.001) and younger age (P=0.002) were risk factors for vitamin D deficiency. Vitamin D levels varied between the quarters with lowest level seen in quarter 1 (P=0.015).
CONCLUSIONS:
There was an overall high prevalence of vitamin D insufficiency (60%) and deficiency (27%). Due to higher risk of hypovitaminosis D, particular attention should be placed in patients with an ASA score ≥3, and patients scheduled during winter season.
Conclusion from PDF
Patients scheduled for lower extremity TJA in a region of the United States, whose latitude is 41° 30' N, have an overall high prevalence of vitamin D insufficiency (60%) and deficiency (27%). Based on our findings, due to higher risk of hypovitaminosis D, particular attention should be placed in patients with an ASA score ≥3, and scheduled during winter season. Further research is needed to establish the definitive prevalence of hypovitaminosis D and the potential detrimental effect it could have on patient outcomes following TJA. Furthermore, cost-benefit analysis must determine if universal screening or treatment should be included in TJA preoperative guidelines. In summary, although we were able to identify several risk factors associated with low vitamin D insufficiency and deficiency, the effect of these conditions on patient outcomes following TJA remains to be determined, as there is a paucity of studies demonstrating causal relationship between low vitamin D levels and poor patient outcomes.
