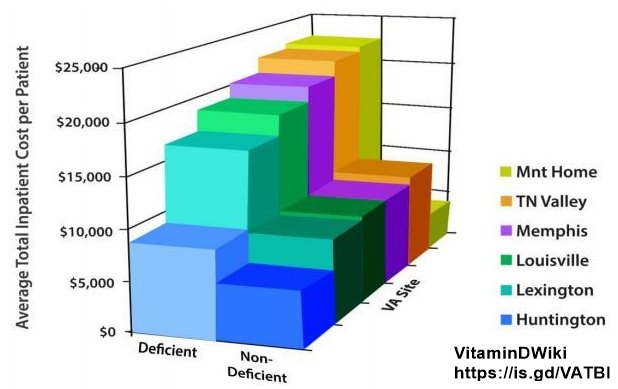
40 percent less likely to die if vitamin D was prescribed (10,000 VA patients, no surprise)
The Effects of Vitamin D Supplementation and 25-Hydroxyvitamin D Levels on the Risk of Myocardial Infarction and Mortality
J Endocr Soc. 2021 Jul 15;5(10):bvab124. doi: 10.1210/jendso/bvab12
Prakash Acharya 1, Tarun Dalia 1, Sagar Ranka 1, Prince Sethi 1, Olurinde A Oni 2, Maya S Safarova 1, Deepak Parashara 1 2 3, Kamal Gupta 1, Rajat S Barua 1 2 3

 Click on image to see study from 2012
---
1. Mortality starts with:
{include}
1. Likewise higher D ==> less COVID death - perhaps >40 ng is needed for COVID
* COVID-19 mortality was associated with vitamin D deficiency of 47 countries – July 2021
* COVID-19 death in hospital 5X more likely if low vs high vitamin D – preprint June 2021
* COVID-19 deaths 1.5X less likely if more than 40 ng of vitamin D – US VA – April 2021 Note: VA
* Risk of COVID-19 death was 4.9 X higher if very low vitamin D – March 31, 2021
* Poor COVID-19 prognosis was 6 X more likely if low vitamin D – Jan 21, 2021
Click on image to see study from 2012
---
1. Mortality starts with:
{include}
1. Likewise higher D ==> less COVID death - perhaps >40 ng is needed for COVID
* COVID-19 mortality was associated with vitamin D deficiency of 47 countries – July 2021
* COVID-19 death in hospital 5X more likely if low vs high vitamin D – preprint June 2021
* COVID-19 deaths 1.5X less likely if more than 40 ng of vitamin D – US VA – April 2021 Note: VA
* Risk of COVID-19 death was 4.9 X higher if very low vitamin D – March 31, 2021
* Poor COVID-19 prognosis was 6 X more likely if low vitamin D – Jan 21, 2021
📄 Download the PDF from VitaminDWiki
Objective: The aim of the study was to examine the effects of the vitamin D (Vit-D) treatment and nontreatment on Vit-D-deficient patients without a prior history of myocardial infarction (MI).
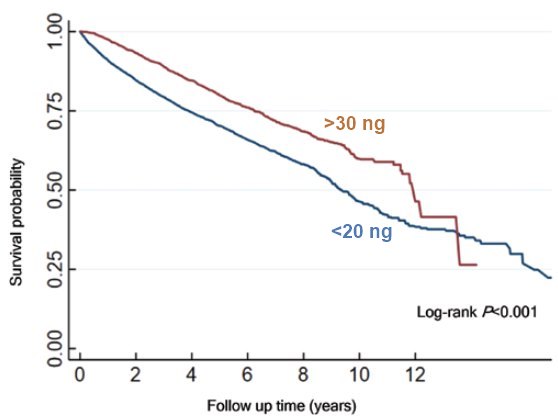
Materials and methods: This was a retrospective, observational, nested case-control study of patients (N = 20 025) with low 25-hydroxyvitamin D ([25-OH]D) levels (<20 ng/mL) who received care at the Veterans Health Administration from 1999 to 2018. Patients were divided into 3 groups:
Group A (untreated, levels ≤20 ng/mL),
Group B (treated, levels 21-29 ng/mL), and
Group C (treated, levels ≥30 ng/mL).
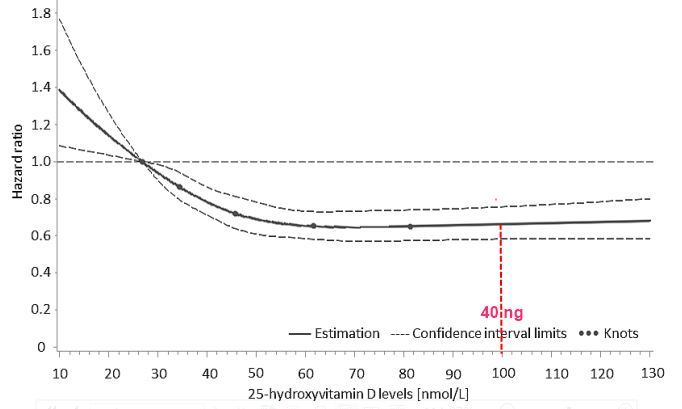
The risk of MI and all-cause mortality were compared utilizing propensity score-weighted Cox proportional hazard models.
Results: Among the cohort of 20 025 patients, the risk of MI was significantly lower in Group C than in Group B (hazard ratio [HR] 0.65, 95% CI 0.49-0.85, P = .002) and Group A (HR 0.73, 95% CI 0.55-0.96), P = .02). There was no difference in the risk of MI between Group B and Group A (HR 1.14, 95% CI 0.91-1.42, P = 0.24).
Compared with Group A, both
Group B (HR 0.59, 95% CI 0.54-0.63, P < .001) and
Group C (HR 0.61, 95% CI 0.56-0.67, P < .001)
had significantly lower all-cause mortality.
There was no difference in all-cause mortality between Group B and Group C (HR 0.99, 95% CI 0.89-1.09, P = .78).
Conclusions: In patients with Vit-D deficiency and no prior history of MI, treatment to the (25-OH)D level of >20 ng/mL and >30 ng/mL was associated with a significantly lower risk of all-cause mortality. The lower risk of MI was observed only in individuals maintaining (25-OH)D levels ≥30 ng/mL.
Short URL= https://is.gd/acharya2021
