First episode psychosis associated with a 33 percent lower vitamin D in 3 races
Vitamin D deficiency in first episode psychosis: A case-control study.
Schizophr Res. 2013 Sep 20. pii: S0920-9964(13)00472-6. doi: 10.1016/j.schres.2013.08.036.
Crews M, Lally J, Gardner-Sood P, Howes O, Bonaccorso S, Smith S, Murray RM, Di Forti M, Gaughran F.
Bromley Assertive Outreach and Rehabilitation Team, Oxleas NHS Foundation Trust, London, United Kingdom; Institute of Psychiatry, King's College London, London, United Kingdom.
BACKGROUND: Vitamin D deficiency is seen in a high proportion of people with established psychotic disorders, but it is not known if this is present at onset of the illness. We set out to examine vitamin D levels in people with their first episode of psychosis (FEP).
METHOD: We conducted a matched case-control study to examine vitamin D levels and rates of vitamin D deficiency in sixty nine patients presenting with their FEP and sixty nine controls matched for age, sex and ethnicity. Differences between groups were tested using student's-t tests, paired t-tests and odds ratios for further analysis.
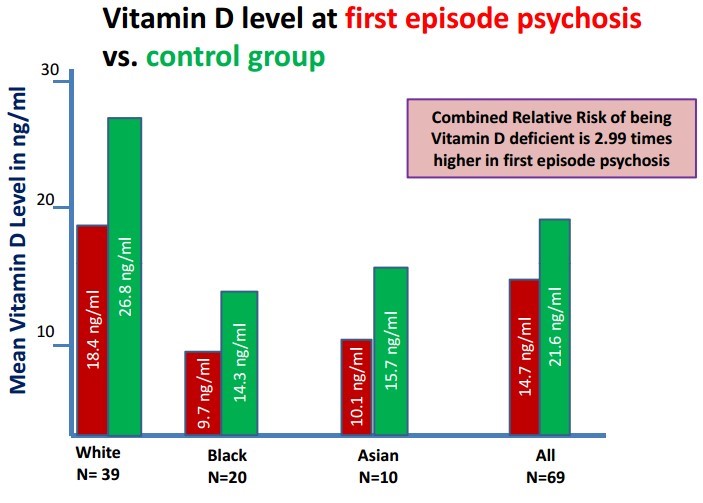
RESULTS: Vitamin D levels were significantly lower in cases than in controls (p<0.001). The odds ratio of being vitamin D deficient was 2.99 in the FEP group relative to the control group. There was no correlation between vitamin D levels and length of hospitalisation in the patient group (r=-0.027, p=0.827).
CONCLUSIONS: We found higher rates of vitamin D deficiency in people with FEP compared to matched controls. Given that vitamin D is neuroprotective; that developmental vitamin D deficiency may be a risk factor for psychosis, and that incipient psychosis may affect lifestyle factors and diet, future studies are required to examine this association further. In the meantime, there is a need for more widespread testing of vitamin D levels in FEP and for the development of appropriate management strategies.
© 2013 Elsevier B.V. All rights reserved.
PMID: 24060571
References
Almeras L, Eyles D, Benech P, Laffite D, Villard C, Patatian A, et al. Developmental vitamin D deficiency alters brain protein expression in the adult rat: implications for neuropsychiatric disorders. Proteomics. 2007;7(5):769–780
Amminger GP, Schafer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, et al. Long-chain omega−3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch. Gen. Psychiatry. 2010;67(2):146–154
Bebbington PE, Nayani T. The Psychosis Screening Questionnaire. Int. J. Methods Psychiatr. Res. 1995;5:11–19
Berg AO, Melle I, Torjesen PA, Lien L, Hauff E, Andreassen OA. A cross-sectional study of vitamin D deficiency among immigrants and Norwegians with psychosis compared to the general population. J. Clin. Psychiatry. 2010;71(12):1598–1604
Berk M, Jacka FN, Williams LJ, Ng F, Dodd S, Pasco JA. Is this D vitamin to worry about? Vitamin D insufficiency in an inpatient sample. Aust. N. Z. J. Psychiatry. 2008;42(10):874–878
Bischoff-Ferrari HA. Optimal serum 25-hydroxyvitamin D levels for multiple health outcomes. Adv. Exp. Med. Biol. 2008;624:55–71
Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am. J. Clin. Nutr. 2006;84(1):18–28
Boonen S, Bischoff-Ferrari HA, Cooper C, Lips P, Ljunggren O, Meunier PJ, et al. Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcif. Tissue Int. 2006;78(5):257–270
Brot C, Jorgensen NR, Sorensen OH. The influence of smoking on vitamin D status and calcium metabolism. Eur. J. Clin. Nutr. 1999;53(12):920–926
Chang C-K, Hayes RD, Perera G, Broadbent MTM, Fernandes AC, Lee WE, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One. 2011;6(5):1–6
Cutillas-Marco E, Fuertes-Prosper A, Grant WB, Morales-Suarez-Varela M. Vitamin D deficiency in South Europe: effect of smoking and aging. Photodermatol. Photoimmunol. Photomed. 2012;28(3):159–161
Eyles DW, Burne TH, McGrath JJ. Vitamin D, effects on brain development, adult brain function and the links between low levels of vitamin D and neuropsychiatric disease. Front. Neuroendocrinol. 2013;34(1):47–64
Ford L, Graham V, Wall A, Berg J. Vitamin D concentrations in an UK inner-city multicultural outpatient population. Ann. Clin. Biochem. 2006;43(Pt 6):468–473
Fuller KE, Casparian JM. Vitamin D: balancing cutaneous and systemic considerations. South. Med. J. 2001;94(1):58–64
Gama R, Waldron JL, Ashby HL, Cornes MP, Bechervaise J, Razavi C, et al. Hypovitaminosis D and disease: consequence rather than cause?. BMJ. 2012;345:(e5706-e5706)
Grandi NC, Breitling LP, Brenner H. Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Prev. Med. 2010;51(3–4):228–233
Groves NJ, Kesby JP, Eyles DW, McGrath JJ, Mackay-Sim A, Burne TH. Adult vitamin D deficiency leads to behavioural and brain neurochemical alterations in C57BL/6J and BALB/c mice. Behav. Brain Res. 2013;241:120–131
Harvey NC, Cooper C. Vitamin D: some perspective please. BMJ. 2012;345:e4695;(Jul 19)
Hermann AP, Brot C, Gram J, Kolthoff N, Mosekilde L. Premenopausal smoking and bone density in 2015 perimenopausal women. J. Bone Miner. Res. 2000;15(4):780–787
Hewison M. Vitamin D and innate and adaptive immunity. Vitam. Horm. 2011;86:23–62
Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am. J. Clin. Nutr. 2004;80(6 Suppl.):1678S–1688S
Holick MF. Diabetes and the vitamin D connection. Curr. Diab. Rep. 2008;8(5):393–398
Honasoge M, Rao DS. Metabolic bone disease in gastrointestinal, hepatobiliary, and pancreatic disorders and total parenteral nutrition. Curr. Opin. Rheumatol. 1995;7(3):249–254
Humble MB, Gustafsson S, Bejerot S. Low serum levels of 25-hydroxyvitamin D (25-OHD) among psychiatric out-patients in Sweden: relations with season, age, ethnic origin and psychiatric diagnosis. J. Steroid Biochem. Mol. Biol. 2010;121(1–2):467–470
Hypponen E, Power C. Hypovitaminosis D in British adults at age 45y: nationwide cohort study of dietary and lifestyle predictors. Am. J. Clin. Nutr. 2007;85(3):860–868
Iuliano-Burns S, Wang XF, Ayton J, Jones G, Seeman E. Skeletal and hormonal responses to sunlight deprivation in Antarctic expeditioners. Osteoporos. Int. 2009;20(9):1523–1528
Klontz KC, Acheson DW. Dietary supplement-induced vitamin D intoxication. N. Engl. J. Med. 2007;357(3):308–309
Lally J, Gardner-Sood P, Howes O, Smith S, Atakan Z, Greenwood K, et al. Vitamin D Deficiency in Schizophrenia—A Need for Increased Vigilance?. In: International Congress on Schizophrenia Research (ICOS-R), Orlando, Florida. 2013;
Looker AC, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR. Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone. 2002;30(5):771–777; Full-Text PDF (116 KB)
Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000–2004. Am. J. Clin. Nutr. 2008;88(6):1519–1527
McCann JC, Ames BN. Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction?. FASEB J. 2008;22(4):982–1001
McGrath J. Hypothesis: is low prenatal vitamin D a risk-modifying factor for schizophrenia?. Schizophr. Res. 1999;40(3):173–177; Full-Text PDF (74 KB)
McGrath J, Saari K, Hakko H, Jokelainen J, Jones P, Jarvelin MR, et al. Vitamin D supplementation during the first year of life and risk of schizophrenia: a Finnish birth cohort study. Schizophr. Res. 2004;67(2–3):237–245; Full-Text PDF (124 KB)
McGrath JJ, Burne TH, Féron F, Mackay-Sim A, Eyles DW. Developmental vitamin D deficiency and risk of schizophrenia: a 10-year update. Schizophr. Bull. 2010;36(6):1073–1078
McGrath JJ, Eyles DW, Pedersen CB, Anderson C, Ko P, Burne TH, et al. Neonatal vitamin D status and risk of schizophrenia: a population-based case–control study. Arch. Gen. Psychiatry. 2010;67(9):889–894
McGrath J, Brown A, St Clair D. Prevention and schizophrenia—the role of dietary factors. Schizophr. Bull. 2011;37(2):272–283
Meaney AM, Smith S, Howes OD, O'brien M, Murray RM, O'keane V. Effects of long-term prolactin-raising antipsychotic medication on bone mineral density in patients with schizophrenia. Br. J. Psychiatry. 2004;184(6):503–508
Menkes DB, Lancaster K, Grant M, Marsh RW, Dean P, du Toit SA. Vitamin D status of psychiatric inpatients in New Zealand's Waikato region. BMC Psychiatry. 2012;12:68
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B. Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol. Psychiatry. 2011;70(7):663–671; Full-Text PDF (326 KB)
Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos. Int. 2009;20(11):1807–1820
Orton SM, Ramagopalan SV, Para AE, Lincoln MR, Handunnetthi L, Chao MJ, et al. Vitamin D metabolic pathway genes and risk of multiple sclerosis in Canadians. J. Neurol. Sci. 2011;305(1–2):116–120
Pack AM, Gidal B, Vazquez B. Bone disease associated with antiepileptic drugs. Cleve. Clin. J. Med. 2004;71(2):S42–S48
Pearce SH, Cheetham TD. Diagnosis and management of vitamin D deficiency. BMJ. 2010;11(340):142–147
Rosen CJ. Clinical practice. Vitamin D insufficiency. N. Engl. J. Med. 2011;364(3):248–254
Skversky AL, Kumar J, Abramowitz MK, Kaskel FJ, Melamed ML. Association of glucocorticoid use and low 25-hydroxyvitamin D levels: results from the National Health and Nutrition Examination Survey (NHANES): 2001–2006. J. Clin. Endocrinol. Metab. 2011;96(12):3838–3845
Tiangga E, Gowda A, Dent JA. Vitamin D deficiency in psychiatric in-patients and treatment with daily supplements of calcium and ergocalciferol. Psychiatr. Bull. 2008;32(10):390–393
Verrotti A, Coppola G, Parisi P, Mohn A, Chiarelli F. Bone and calcium metabolism and antiepileptic drugs. Clin. Neurol. Neurosurg. 2010;112(1):1–10; Full-Text PDF (217 KB)
Vimaleswaran KS, Berry DJ, Lu C, Tikkanen E, Pilz S, Hiraki LT, et al. Causal relationship between obesity and vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med. 2013;10(2):1–13
Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503–511
Wang L, Song Y, Manson JE, Pilz S, Marz W, Michaelsson K, et al. Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: a meta-analysis of prospective studies. Circ. Cardiovasc. Qual. Outcomes. 2012;5(6):819–829
Wharton B, Bishop N. Rickets. Lancet. 2003;362(9393):1389–1400; Full-Text PDF (311 KB)
White T, Anjum A, Schulz C. The schizophrenia prodrome. Am. J. Psychiatry. 2006;163:376–380
Wood H. Multiple sclerosis: sunlight and vitamin D influence multiple sclerosis risk independently of HLA-DRB1[ast]15 status. Nat. Rev. Neurol. 2012;8(3):122-122
World Health Organisation . WHO Scientific Group on the Prevention and Management of Osteoporosis: Report of a WHO Scientific Group. Geneva: World Health Organisation; 2003;
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 2000;72(3):690–693
Zadshir A, Tareen N, Pan D, Norris K, Martins D. The prevalence of hypovitaminosis D among US adults: data from the NHANES III. Ethn. Dis. 2005;15(Suppl. 4-5):97–101
See also VitaminDWiki
Search Psychosis in VitaminDWiki 217 items Dec 2017
ADHD, Autism, Early Psychosis and Omega-3 – review Dec 2017
Psychosis in dark skinned people 3.5 X higher if low level of vitamin D – May 2012
Vitamin D3 associated with fewer psychotic episodes, D2 with more – July 2012
Psychiatric disorders 4X more likely in teens if low vitamin D - Nov 2011
99 percent of psychiatric population had less than 30 ng of vitamin D – June 2013
Overview Schizophrenia and Vitamin D contains the following summary
- {include}
See also web
Vitamin D status: Connection to first episode of psychosis?
Vitamin D Council review of this study, Oct 2013, Behind a $5 a month paywall
Nanogram/ml levels
| Whites | Blacks | Asians | |
| Cases: | 18 | 9.6 | 10 |
| Controls: | 27 | 14 | 16 |
- Vitamin D insufficiency in psychiatric inpatients.
- J Psychiatr Pract. 2013 Jul;19(4):296-300. doi: 10.1097/01.pra.0000432599.24761.c1.
- The mean vitamin D level on admission was 22.3 ng/mL, with a range of 4-79.2 ng/mL. The incidence of vitamin D insufficiency (defined as levels < 30 ng/mL) was 75%.
- Ethnic minority position and risk for psychotic disorders (in Netherlands)
- Curr Opin Psychiatry. 2013 Mar;26(2):166-71. doi: 10.1097/YCO.0b013e32835d9e43.
- A meta-analysis found that both first and second-generation migrants have on average a two-fold increase in risk for psychotic disorders.
- (That is, dark skinned people, which typically have lower vitamin D, were 2X more likely to have psychotic disorders)
- Vitamin D deficiency and psychotic features in mentally ill adolescents: a cross-sectional study .
- BMC Psychiatry. 2012 May 9;12:38. doi: 10.1186/1471-244X-12-38.
- The association for vitamin D deficiency and psychotic features was substantial (OR 3.5; 95% CI 1.4-8.9; p <0.009).
- Race was independently associated with vitamin D deficiency and independently associated with psychosis for those who were Asian or biracial vs. white (OR=3.8; 95% CI 1.1‒13.4; p<0.04).
Review of the study in MedScape
- Previous research has shown that individuals with psychotic disorders often have vitamin D deficiency. However, this could be caused by long periods of hospitalization, use of anticonvulsant medications, or poor diet, note the investigators.
- 69 adult inpatients (39% men; 56% white, 29% black, 14% Asian; mean age, 31 years
- 14.6 ng vs 21.5 ng, Deficiency 36.2% vs 15.9%
They note 3 possible causes for the association:
During the often long prodromal phase, many patients with schizophrenia withdraw from normal activities, and this might result in a reduction in sunlight exposure.
Having low levels of vitamin D over a long period may be a risk factor for developing psychosis.
Because vitamin D is a negative acute-phase reactant, levels can decrease during an inflammatory response.
- Comment on MedScape: My clinical experience shows that "sick" patients require a lot more vit D3 supplements than usual and than healthier patients to maintain the same blood levels . It seems that the active phases of illness consume this vitamin in a fashion similar to how patients with colds can tolerate higher levels of vitamin C supplementation before they get loose stools when compared to their tolerated level when healthy.
- New research links vitamin D deficiency with serious mental disorders Dec 2013, review of study on this page
- Arctic hysteria.=“piblokto.” (Eskimos) = “cabin fever.”
