Use of Vitamin D in Clinical practice – 2008
Cannell JJ, Hollis BW.
Alternative Medicine Review Volume 13, Number 1 2008; Review Article
(Note: bulleting and bolding by VitaminDWiki)
The recent discovery - from a meta-analysis of 18 randomized controlled trials - that supplemental cholecalciferol (vitamin D) significantly reduces all-cause mortality emphasizes the medical, ethical, and legal implications of promptly diagnosing and adequately treating vitamin D deficiency.
Not only are such deficiencies common, and probably the rule, vitamin D deficiency is implicated in most of the diseases of civilization.
Vitamin D's final metabolic product is a potent, pleiotropic, repair and maintenance, secosteroid hormone that targets more than 200 human genes in a wide variety of tissues, meaning it has as many mechanisms of action as genes it targets.
One of the most important genes vitamin D upregulates is for cathelicidin, a naturally occurring broad-spectrum antibiotic.
Natural vitamin D levels, those found in humans living in a sun-rich environment, are between 40-70 ng/mL, levels obtained by few modern humans.
Assessing serum 25-hydroxy-vitamin D (25(OH)D) is the only way to make the diagnosis and to assure treatment is adequate and safe.
Three treatment modalities exist for vitamin D deficiency:
sunlight,
artificial ultraviolet B (UVB) radiation, and
vitamin D supplementation.
Treatment of vitamin D deficiency in otherwise healthy patients with 2,000-7,000 IU vitamin D3 per day should be sufficient to maintain year-round 25(OH)D levels between 40-70 ng/mL.
In those with serious illnesses associated with vitamin D deficiency, such as cancer, heart disease, multiple sclerosis, diabetes, autism, and a host of other illnesses, doses should be sufficient to maintain year-round 25(OH)D levels between 55-70 ng/ mL.
Vitamin D-deficient patients with serious illness should not only be supplemented more aggressively than the well, they should have more frequent monitoring of serum 25(OH) D and serum calcium.
Vitamin D should always be adjuvant treatment in patients with serious illnesses and never replace standard treatment.
Theoretically, pharmacological doses of vitamin D (2,000 IU/kg/day for three days) may produce enough of the naturally occurring antibiotic cathelicidin to cure common viral respiratory infections, such as influenza and the common cold, but such a theory awaits further science.
Introduction
A recent meta-analysis of 18 randomized controlled trials (RCT) found that cholecalciferol (vitamin D) significantly reduced total mortality.1 This discovery is all the more remarkable because of the relatively low doses of vitamin D used (mean dose 528 IU (13 mcg)) and because the finding persisted across a number of subgroup analyses. In spite of the low doses used and the short duration of the trials, vitamin D's mortality reduction was seven percent.2 Indeed, the recent discovery that statins significantly increase 25-hydroxy-vitamin D (25(OH)D) levels raise the possibility that some - or all - of the mortality reduction of statins may be mediated through increases in vitamin D levels.3,4
Lappe et al recently reported the first RCT of vitamin D in preventing internal cancers and found a 60-percent reduction in such cancers by increasing baseline 25(OH)D levels from 29 ng/mL to 38 ng/mL with 1,100 IU (28 mcg) per day.5 Baseline and treatment-induced serum 25(OH)D levels were strong and independent predictors of cancer risk. Lappe et al's study left open the possibility that higher doses and higher treatment-induced 25(OH)D levels might prevent even more cancers. (Note that 25(OH)D levels are reported in the literature as either ng/mL or nmol/L; 1.0 ng/mL equals 2.5 nmol/L.)
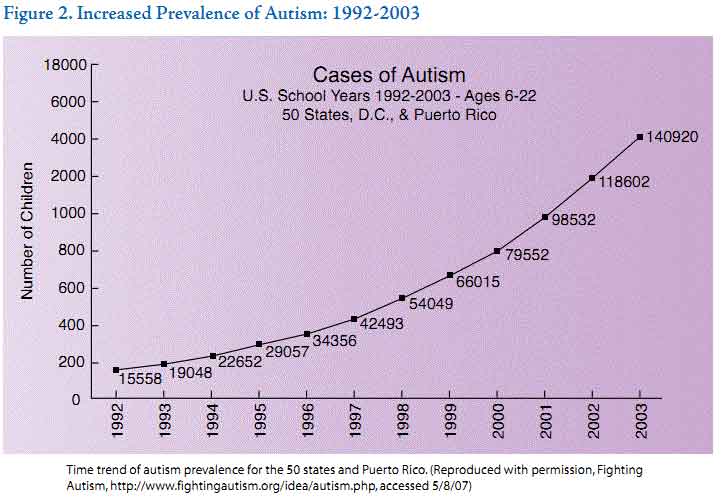
Besides cancer, vitamin D deficiency is associated with cardiovascular disease, hypertension, stroke, diabetes, multiple sclerosis, rheumatoid arthritis, inflammatory bowel disease, osteoporosis, periodontal disease, macular degeneration, mental illness, propensity to fall, and chronic pain.6-10 A recent review presented considerable evidence that influenza epidemics, and perhaps even the common cold, are brought on by seasonal deficiencies in antimicrobial peptides (AMP), such as cathelicidin, secondary to seasonal deficiencies in vitamin D.11 Results of an RCT support the theory, finding 2,000 IU of vitamin D/day for one year virtually eliminated self-reported incidence of colds and influenza (Figure 1).12 Even the current triple childhood epidemics of autism 13 (Figure 2), asthma,14 and type 1 diabetes,15 all of which blossomed after sun-avoidance advice became widespread, might be the tragic and iatrogenic sequela of gestational or early childhood vitamin D deficiencies brought on by medical advice to avoid the sun.
Claims that vitamin D may help prevent such a wide variety of diseases seem incredible until one realizes vitamin D is not a vitamin; rather, it is the only known substrate for a potent, pleiotropic, repair and maintenance, secosteroid hormone with a single endocrine function, but multiple autocrine functions.
Previously, many practitioners thought vitamin D's activity was principally its endocrine function - the regulation of serum calcium - and was thus mainly involved in bone metabolism. Indeed, the classic endocrine function of vitamin D begins when the kidney hydroxylates 25(OH)D into 1,25(OH)2D, which then acts, both directly and indirectly, to maintain serum calcium.
Figure 1. Incidence of Colds/Influenza After 2,000 IU Vitamin D Daily for One Year
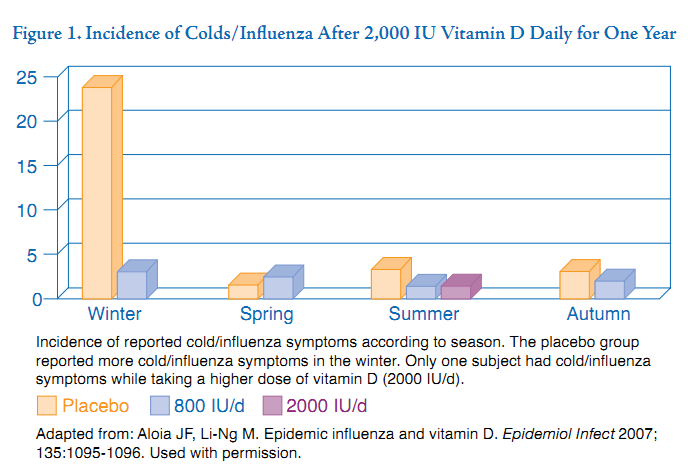
Incidence of reported cold/influenza symptoms according to season.
The placebo group reported more cold/influenza symptoms in the winter.
Only one subject had cold/influenza symptoms while taking a higher dose of vitamin D (2000 IU/d).
Adapted from: Aloia JF, Li-Ng M. Epidemic influenza and vitamin D. Epidemiol Infect 2007; 135:1095-1096. Used with permission.
Figure 2. Increased Prevalence of Autism: 1992-2003
However, in the last ten years, it has become clear the vitamin D steroid hormone system includes more than the classic endocrine pathway used to preserve calcium economy.16 The enzyme that further hydroxylates 25(OH)D to 1,25(OH)2D (activated vitamin D, the steroid hormone) is present in a wide variety of human tissues other than kidney. 1,25(OH)2D is autonomously made in tissues and directly affects numerous cells via its autocrine, and presumed paracrine, functions.17 Most organs show evidence of end organ responsiveness to 1,25(OH)2D.18 Like all steroid hormones, 1,25(OH)2D acts as a molecular switch, activating more than 200 target genes, thereby regulating gene expression. Thus, locally produced 1,25(OH)2D exists in most tissues of the body, is under autonomous autocrine control, and has as many mechanisms of action as genes it targets. This explains why the same substance may have a role in preventing cancer, influenza, autism, asthma, multiple sclerosis, and cardiovascular disease, not just curing rickets and osteomalacia (Figure 3).
Such claims leave practitioners with understandable skepticism and multiple questions.
Is vitamin D a cure-all?
When should I recommend vitamin D?
How much should I prescribe?
What form of vitamin D should I use?
How much do children need?
How much do pregnant or breastfeeding women need?
Is it appropriate to use higher doses of vitamin D as adjuvant treatment for any of the above diseases?
How do I interpret vitamin D blood tests and which tests should I order?
What is the risk of toxicity?
Another way to ask many of these questions is, "What is an ideal 25(OH)D level?"
Levels needed to optimize intestinal calcium absorption (34 ng/mL)19 are lower than those needed to optimize neuromuscular performance (38 ng/mL).20
Recent pooled meta-analyses estimate 25(OH)D levels of 52 ng/mL are needed to effect a 50-percent reduction in the incidence of breast cancer.21 Although some experts believe the lower limit of adequate 25(OH)D levels is in the low 30s, 22,23 others recommend a lower limit of 40 ng/mL; 24,25 there is certainly no scientific consensus.
Ideal levels are unknown but are probably close to levels present when the human genome evolved in sub-equatorial Africa. Natural levels, such as those found at the end of summer in 30 young men who spent the summer working outdoors, were around 50 ng/mL;26 however, these levels are obtained by only a small fraction of people.27 Furthermore, despite such summertime levels, at the end of winter 25(OH)D levels in 50 percent of these men dropped to less than 30 ng/mL, indicating a sun-induced level of 50 ng/mL at the end of summer is inadequate to maintain such a level during wintertime.
Figure 3. Autocrine and Endocrine Functions of Vitamin D
Another way to ask the "ideal 25(OH)D" question involves understanding vitamin D's unique pharmacokinetics. Unlike any other steroid hormone system, the substrate concentrations for the liver production of 25(OH)D are absolutely rate limiting. This means the liver enzymes that initially hydroxylate vitamin D to form 25(OH)D and the enzyme in tissue that generates 1,25(OH)2D operate below their Michaelis-Menten constants throughout the full range of modern human substrate concentrations; i.e., the reactions follow first-order mass action kinetics.28 The more vitamin D that is ingested, the more is converted into 25(OH)D, and the more is converted into 1,25(OH)2D in the tissues. The reaction appears to be uncontrolled; an aberrant, totally unique, and potentially dangerous situation for a steroid hormone system. Imagine, for example, if cortisol, testosterone, progesterone, or estradiol levels were entirely dependent on the intake of their substrate, cholesterol.
Hollis et al recently explained this conundrum and concluded very few humans obtain enough vitamin D even if they take several thousand units per day.29 Hollis et al studied the pharmacokinetics of the parent compound, vitamin D, and its first metabolic product, 25(OH)D, in two groups; Hawaiians with significant sun exposure and lactating women receiving 6,400 IU of supplemental vitamin D per day. They found 25(OH)D levels had to exceed a minimum of 40 ng/ mL, and often 50 ng/mL, to begin to detect the parent compound in the blood and begin to normalize the kinetics of 25(OH)D production. In other words, when 25(OH)D levels > 40 ng/mL were achieved, the parent compound began to be detectable in the blood, the reactions became saturable and controlled (like other steroid hormone systems), and thus levels above 40 ng/mL appear to represent the lower limit of "normal" 25(OH) D levels.
This implies virtually everyone has a chronic 25(OH)D substrate deficiency, at least in the winter, and the absence of the parent vitamin D compound (cholecalciferol) in the blood means all available vitamin D is used for metabolic needs and none of it is stored.
Figure 4. Seasonal Serum Levels of 25-hydroxyvitamin D
Because of this, most individuals have chronic substrate starvation, functional vitamin D deficiency, and thus, perhaps, higher risk for the "diseases of civilization."
The ideal 25(OH)D level continues to be debated in scientific circles and consensus awaits further science. However, do we wait for science to complete its work with highly seasonal 25(OH)D levels (Figure 4) that reflect sunlight deprivation, levels where vitamin D steroid pharmacokinetics are aberrant, or is it safer to wait with levels normally achieved by humans in a sun-rich environment, levels where vitamin D's kinetics are normalized (>40 ng/mL)?
Once a practitioner is comfortable with ideal 25(OH)D levels being above 40 ng/mL, the answers to the questions posed above become fairly simple. Healthy humans should be supplemented with enough vitamin D or exposed to enough ultraviolet B (UVB) radiation to achieve natural 25(OH)D levels (40-70 ng/mL) year-round, whether they are infants, children, pregnant women, lactating women, healthy young adults, or the elderly.
What role vitamin D has in treating - rather than preventing - disease is largely unknown, but given vitamin D's genetic mechanism of action, it may have a significant role. For example, vitamin D reduces cellular proliferation, induces differentiation, induces apoptosis, and prevents angioneogenesis, each a laudable goal in cancer treatment. A simple risk-versus-benefit analysis suggests patients with a potentially fatal cancer (see below) may think it wise to maintain 25(OH)D levels in the high end of natural ranges (55-70 ng/mL), ranges that assure vitamin D's kinetics are normalized. While the RCTs needed to clarify vitamin D's role in the treatment of disease are being conducted, a strong case already exists for adequately diagnosing and aggressively treating vitamin D deficiency. 22,25,30
Incidence of Vitamin D Deficiency
Adult vitamin D deficiency is the rule rather than the exception in industrialized nations.31-33 A high number of otherwise healthy children and adolescents are also vitamin D deficient.34,35 Rickets, a disease of the industrial revolution, is being diagnosed more frequently,36 especially in breast-fed infants.37 Alarmingly, given mounting animal data that gestational vitamin D deficiency causes subtle but irreversible brain damage in mammalian offspring,38,39 severe deficiencies are common in newborn infants and pregnant women, especially African-Americans.40 A population-based study of 2,972 U.S. women of childbearing age found 42 percent of African-American women had 25(OH)D levels below 15 ng/mL, and 12 percent had levels below 10 ng/mL. 41
Furthermore, the definition of vitamin D deficiency changes almost yearly as research shows the low end of ideal 25(OH)D ranges are higher than were previously thought. The aforementioned prevalence studies used outdated reference values for low-end 25(OH) D ranges and therefore underestimate the incidence of vitamin D deficiency. Obviously, the higher the low end of the 25(OH)D cutoff point, the higher the percentage of the population defined as deficient. Only 10 percent of the subjects in any of the above studies had 25(OH) D levels > 40 ng/mL.
Vitamin D Metabolism and Physiology
Perhaps because the term "vitamin D" contains the word "vitamin," most people wrongly assume they can obtain adequate amounts by eating a healthy diet. The natural diets most humans consume, however, contain minimal vitamin D, unless those diets are rich in wild-caught fatty fish, sun-dried Shitake mushrooms, or wild reindeer meat. Small amounts of vitamin D are contained in fortified foods, such as fortified milk, some orange juices, and cereals, but such sources are minor contributors to vitamin D stores. Traditionally, the human vitamin D system began in the skin, not in the mouth.
Vitamin D normally enters the circulation after UVB from sunlight strikes 7-dehydro-cholesterol in the skin, converting it to vitamin D3 or cholecalciferol (vitamin D). When taken by mouth, the body metabolizes vitamin D similarly to that generated in the skin. No matter how it arrives in the circulation, the liver readily hydroxylates vitamin D to 25(OH)D, the circulating form of vitamin D. Hundreds of tissues in the body use 25(OH)D as a substrate to make the end-product, 1,25(OH)2D, known as activated vitamin D, a pleiotro-pic seco-steroid. If enough 25(OH)D substrate is available, multiple tissues are free to autonomously produce and locally regulate the amount of steroid needed for any particular disease state.
The skin's manufacture of vitamin D is extraordinarily rapid and remarkably robust; production after only a few minutes of sunlight easily exceeds dietary sources by an order of magnitude. Incidental sun exposure, not dietary intake, is the principal source of vitamin D stores and is a function of skin surface area exposed.42,43 For example, when fair-skinned people sunbathe in the summer (one, full-body, minimal ery-themal dose of UVB), they produce about 20,000 IU of vitamin D in 30 minutes,44 the equivalent of drinking 200 glasses of milk (100 IU/8 oz. glass) or taking 50 standard multivitamins (400 IU/tablet) to obtain the same amount orally.
The fact that 20,000 IU vitamin D can be produced in the skin in 30 minutes of sun exposure, combined with vitamin D's basic genomic mechanism of action, raises profound questions. Why did nature develop a system that delivers huge quantities of a steroid precursor after only brief periods of sun exposure? Would natural selection evolve such a system if the remarkably high input that system achieved were unimportant? As humans evolved in a sun-rich environment (sub-equatorial Africa), is modern sunlight deprivation - and the resultant routinely low levels of this repair-and-maintenance steroid in tissues - a possible common cause of the diseases of civilization?
Factors Affecting Vitamin D Levels
Factors that can affect UVB exposure, and thus the skin's production of vitamin D, include
latitude,
season of the year,
time of day,
air pollution,
cloud cover,
melanin content of the skin,
use of sunblock, age, and the
extent of clothing covering the body.
When the sun is low on the horizon, ozone, clouds, and particulate air pollution deflect UVB radiation away from the earth's surface. Therefore, cutaneous vitamin D production is effectively absent early and late in the day and for the entire day during several wintertime months at latitudes above 35 degrees, and impaired anytime the skies are polluted or cloudy.
Thus, vitamin D deficiency is more common the further poleward the population. For example, Boston, Massachusetts (latitude 42 degrees), has a four-month "vitamin D winter" centered around the winter solstice, when insufficient UVB penetrates the atmosphere to trigger skin production. This becomes an even longer period when the fall and late winter months are included, when sufficient UVB only penetrates around solar noon. In northern Europe and Canada, the "vitamin D winter" can extend for six months. Furthermore, properly applied sunblock, common window glass in homes and cars, and clothing all effectively block UVB radiation - even in the summer. Those who avoid sunlight - at any latitude - are at risk of vitamin D deficiency any time of the year.
For example, a surprisingly high incidence of vitamin D deficiency exists in Miami, Florida, despite its sunny weather and subtropical latitude.45 African-Americans, the elderly, and the obese face added risk. Because melanin in the skin acts as an effective and ever-present sunscreen, dark-skinned people need much longer UVB exposure times to generate the same 25(OH)D stores as fair-skinned individuals.46 The elderly make much less vitamin D than 20-year-olds after exposure to the same amount of sunlight.47 Body fat absorbs vitamin D, thus obesity is a major risk factor for deficiency, with obese African-Americans at an even higher risk.48 Anyone who works indoors, lives at higher latitudes, wears excessive clothing, regularly uses sunblock, is dark-skinned, obese, aged, or who consciously avoids the sun is at high risk for vitamin D deficiency.
Diagnosis of Vitamin D Deficiency
In the absence of a metabolic bone disease such as rickets, osteomalacia, or osteoporosis, most practitioners assume vitamin D deficiency is asymptomatic, although that may be changing. Complaints endemic to every practitioner's office, such as muscular weakness, a feeling of heaviness in the legs, chronic musculoskeletal pain, fatigue, or easy tiring may be symptoms of vitamin D deficiency.49 Such complaints are extremely common, difficult to treat, and easy to dismiss, but they may indicate symptomatic vitamin D deficiency.
Physical examination is usually unremarkable but may reveal undue pain on sternal or tibial pressure if deficiency is severe. The vast majority of cases appear normal on exam, although frequent infections, autoimmune illness, diabetes, cancer, heart disease, major depression, and a host of other "diseases of civilization" may be warning signs that deficiency has been present for many years.22,25
The aged may be wheelchair-bound secondary to vitamin D deficiency-induced myopathy, yet they typically recover mobility after treatment.50 The recent strong association of low mood and cognitive impairment in the aged with vitamin D deficiency 51 suggests depressed mood and/or impaired cognition may be presenting symptoms. A blinded intervention trial found 4,000 IU vitamin D per day improved the mood of endocrinology outpatients,52 but there are no interventional studies of its effects on cognition.
Even without physical signs or symptoms, the physician should screen those at risk. Obtaining and properly interpreting a serum 25(OH)D level is the only way to make the diagnosis. A 25(OH)D level should be obtained at least twice yearly on any patient at risk, once in the early spring for the nadir and once in the late summer for a peak level.53 We recommend 25(OH)D levels be kept above 40 ng/mL year-round (Figure 5).
It is crucial to remember that serum 1,25(OH)2D levels play no role in diagnosing vitamin D deficiency. The kidney tightly controls serum 1,25(OH)2D levels, which are often normal or even elevated in vitamin D deficiency. Therefore, a patient with normal or high 1,25(OH)2D serum levels but low 25(OH)D levels is vitamin D deficient despite high serum levels of the active hormone. Practitioners who rely on serum 1,25(OH)2D levels to make the diagnosis of vitamin D deficiency will routinely miss it.25
Treatment of Vitamin D Deficiency
Three options exist for treatment of vitamin D deficiency: sunlight, artificial UVB light, and vitamin D supplements. An exposure of 10-15 minutes of full-body summer noon-day sun or artificial UVB radiation (such as tanning beds) will input more than 10,000 IU of vitamin D into the systemic circulation of most light-skinned adults. One or two such exposures per week
Author's recommendations for serum 25(OH) vitamin D levels.
should maintain 25(OH)D levels in an ideal range, but adequacy should be assured by 25(OH)D blood levels. Those who choose UVB light for vitamin D repletion, from either sunlight or artificial sources, should avoid sunburn, which is associated with malignant melanoma. Furthermore, they should understand that regular UV exposure ages the skin and increases the risk of non-melanoma skin cancers.
The treatment of choice for vitamin D deficiency is vitamin D, cholecalciferol, also known as vitamin D3. Oral vitamin D treatment is more challenging than treatment with UVB light for several reasons. First, unexpectedly high doses of vitamin D are usually needed to achieve adequate serum 25(OH)D levels. One of the problems with vitamin D terminology is the archaic method used to express dose, international units or IU. One thousand IU of vitamin D sounds like a lot; in fact, it is only .025 mg or 25 micrograms; i.e., one mcg is 40 IU. Second, the amount of vitamin D needed varies with body weight, body fat, age, skin color, season, latitude, and sunning habits. Third, unlike sun exposure, toxicity is possible with oral supplementation - although it is extraordinarily rare.
Cholecalciferol is available over-the-counter and via the Internet in 400, 1,000, 2,000 and (recently) 5,000, 10,000, and 50,000 IU capsules. Supplementation with 1,000 IU per day will usually result in about a 10-ng/mL elevation of serum 25(OH)D when given over 3-4 months. Therefore, a normal weight, healthy adult with an initial level of 10 ng/mL would generally require about 2,000 IU per day to achieve a level of 30 ng/mL in the absence of cutaneous UVB exposure. However, its kinetics are not linear; 1,000 IU per day will substantially raise low baseline levels but a similar dose will not increase higher baseline levels by a similar increment (that is, 2,000 IU per day may not raise 30 ng/mL to 50 ng/mL).
In the absence of significant UVB exposure, input from diet and supplements of approximately 1,000 IU (25 mcg) per day for every 15 kg of body weight may be needed; i.e., an obese 150-kg adult may require up to 10,000 IU per day to achieve a 25(OH)D level of 50 ng/mL. Patients with serious diseases may need more if the metabolic clearance of 25(OH)D is increased (see below).
The only prescription vitamin D preparation available in the United States is the vitamin D analogue ergocalciferol (vitamin D2) , available as 50,000 IU (1.25 mg) capsules. However, ergocalciferol is not human vitamin D, it may be a weaker agonist, it is not normally present in humans, and its consumption results in metabolic by-products not normally found in humans.54 It is also less effective than cholecalciferol in raising 25(OH) D levels.55,56
Recently, 50,000 IU capsules of vitamin D3 became available in retail outlets. Grey at al treated 21 vitamin D-deficient patients with 50,000 IU cholecalciferol weekly for four weeks, then 50,000 IU monthly for one year.57 Blood levels rose from a mean of 11 ng/ mL at baseline to 30 ng/mL at six months and to 31 ng/ mL at one year, indicating monthly doses of 50,000 IU of vitamin D3 do not achieve natural 25(OH)D levels and such levels do not continue to rise after six months of such treatment. If such intermittent high doses of cholecalciferol are used, maintenance requirements are probably 50,000 IU every 1-2 weeks in most adults, although such supplementation studies have not been done.
Cod liver oil contains a variable amount of vitamin D, but usually contains high amounts of vitamin A. Consumption of pre-formed retinols, even in amounts consumed in multivitamins, may be causing low-grade, but widespread, bone toxicity.58 Vitamin A antagonizes the action of vitamin D,59 and high retinol intake thwarts vitamin D's protective effect on distal colorectal adenoma.60 The authors do not recommend cod liver oil.
Neither the regular consumption of officially recommended amounts of vitamin D (e.g., 400 IU in a multivitamin), nor the regular consumption of vitamin D fortified foods (e.g., 100 IU per 8 oz. glass of milk), effectively prevent vitamin D deficiency.61,62 Furthermore, 2,000 IU/day for one year failed to achieve a 32 ng/mL target 25(OH)D concentration in 40 percent of 104 African-American women studied.63 The administration of 4,000 IU/day for more than six months to middle-age Canadian endocrinology outpatients resulted in average 25(OH)D levels of 44 ng/mL and produced no side effects other than improved mood.52 Heaney estimates 3,000 IU/day is required to assure that 97 percent of Americans obtain levels greater than 35 ng/mL 23 Healthy adult men utilize up to 5,000 IU of vitamin D per day, if it is available. 64
In general, the more a patient weighs, the more vitamin D will be required, and large amounts of body fat further increase requirements. Not only are baseline 25(OH)D levels lower in the obese, the obese require higher doses of oral supplements or UV radiation than lean individuals in order to obtain the same increases in 25(OH)D blood levels.65 Fat malabsorption syndromes may increase oral requirements or necessitate the use of ultraviolet radiation. Advancing age impairs the skin's ability to make vitamin D, so older persons generally need higher supplemental doses than younger ones. Therefore, dark-skinned, large, obese, or older patients often require higher maintenance doses than fair-skinned, small, thin, or younger ones.
Loading doses of 50,000 IU (1.25 mg) of cholecalciferol per day for a week, or at the most two, are safe to use before beginning maintenance therapy.
Cytochrome P-450 enzymes are responsible for both the initial metabolism and subsequent catabolism of vitamin D. Therefore, drugs dependent on cytochrome P-450 enzymes - and there are many - may affect vitamin D metabolism. What clinically relevant interactions these substances - including cardiac drugs, erythromycins, psychotropics, and even grapefruit juice - have on the metabolism of vitamin D is an area awaiting further research. Of the research done on drug/vitamin D interactions, anticonvulsants, corticosteroids, cimetidine, anti-tuberculosis agents, theophylline, and orlistat may lower 25(OH)D levels, while thiazide diuretics and statins increase 25(OH)D levels.66,67 Patients on medications of any kind should have frequent testing of 25(OH)D levels when being treated with doses above 2,000 IU per day.
The authors recommend parents supplement breast-fed infants with at least 800 IU of vitamin D daily, while formula fed infants need 400 IU per day. Infants and toddlers may be at extremely high risk of deficiency during weaning. Around 12-18 months, many stop drinking vitamin D-fortified infant formula and begin consuming unfortified juices, which - interestingly - is also the time many autistic children rapidly deteriorate. Toddlers and young children who do not get regular sun exposure should take 1,000-2,000 IU daily year-round, depending on body weight, keeping in mind that current Food and Nutrition Board recommendations state doses up to 2,000 IU per day are safe for children over the age of one. In the summer, children who spend time in the sun without wearing sunblock will need little or none. Parents can easily open 1,000 IU capsules containing powdered vitamin D and dissolve the contents in juice or food for easy delivery to children and infants.
Vitamin D deficiency in pregnancy is an ongoing epidemic,68 and animal evidence continues to accumulate that maternal vitamin D deficiency permanently injures fetal brains. 38,39,69 Pregnant women - or women thinking of becoming pregnant - should have 25(OH)D levels checked every three months and be adequately treated, often with 5,000 IU or more per day, as outlined above.70 Lactating women require even more, up to 7,000 IU per day, to assure breast milk is a rich source of vitamin D.71 Infants being breast fed by supplementing mothers will not require additional supplementation, but will require adequate supplementation during and after weaning.
Treatment of Disease
By far the most common reason to treat with vitamin D is osteoporosis, but the dose needed remains controversial because the lowest effective dose (800 IU/ day) is known, but the ideal dose is not.72 Currently, virtually all of the evidence that vitamin D is an effective adjuvant for the treatment of other serious medical conditions is anecdotal, implied by epidemiological studies, from open trials, or inferred from vitamin D's mechanism of action.
For example, there is an anecdotal report that pharmacological doses of vitamin D are effective in treating - not just preventing - viral respiratory infections. 73 Doses of 2,000 IU/kg body weight for three days (200,000 IU per day for three days for a 100-kg adult) may seem excessive to those unfamiliar with vitamin D's pharmacology and toxicity. In fact, such doses are common in many parts of the world simply to prevent or treat vitamin D deficiency.
For example, single injections of 600,000 IU (15 mg) vitamin D raised 25(OH)D levels from 2 ng/ mL to 22 ng/mL at two weeks and to 27 ng/mL at six weeks in 10 elderly subjects, with no evidence of toxicity.74 Indeed, a single injection of 600,000 IU of vitamin D is not only safe; such doses were recently recommended in the autumn for the elderly, simply to prevent wintertime vitamin D deficiency.75 Likewise, there was no evidence of toxicity in young men taking 50,000 IU of vitamin D per day for six weeks (although such a dose would become toxic if taken over a longer period).76 In 32 severely vitamin D-deficient elderly patients, 50,000 IU/day for 10 days showed no evidence of toxicity and only raised 25(OH)D levels by an average of 5 ng/mL three months after administration. In no patient did levels increase more than 11 ng/mL at three months.77
Treatment of colds and influenza with pharmacological doses of vitamin D may only be the tip of the infectious disease iceberg. As Aloia and Li-Ng have pointed out,12 it is intriguing that vitamin D-sensitive antimicrobial peptides (AMP) inhibit the HIV virus and there is evidence that vitamin D plays a role in HIV.78 Invasive pneumococcal disease, meningococcal disease, and group A streptococcal disease are more common when vitamin D levels are lowest (winter)79-81 and all three bacteria are sensitive to AMP,82-84 raising the possibility that pharmacological doses of vitamin D would be an effective adjuvant treatment. In fact, the dramatically increased production of AMPs by vitamin D and the broad spectrum of action of AMP make it reasonable to hypothesize that pharmacological doses of vitamin D are effective adjuvants in treating a large number of infections.
In a recent report, 12 patients in active phases of multiple sclerosis were treated with progressively increasing weekly doses of vitamin D3 (the equivalent of starting with 4,000 IU per day and increasing to 40,000 IU per day) and calcium.85 Mean serum concentrations of 25(OH)D initially were 31 ng/mL and rose to a mean of 154 ng/mL at the end of 28 weeks, with no abnormalities in serum or urine calcium detected in the 12 subjects. The number of MS lesions per patient on brain scan decreased from an initial mean of 1.75 at the beginning to a mean of 0.83 (p=0.03) at the end of the study. However, doses of 40,000 IU per day may cause toxicity if given for longer periods; certainly, such doses flirt with toxicity. Doses of 10,000 IU per day may well have achieved the same result without the risk of toxicity.
Both epidemiological evidence and vitamin D's mechanism of action suggest it may have a treatment effect in early cancer. For example, a study of recurrence-free survival in early-stage, non-small-cell lung cancer patients found those with the highest vitamin D input had double the five-year recurrence-free survival and much better overall survival than those with the lowest.86 This strongly implies a vitamin D treatment effect, i.e., untreated vitamin D deficiency in non-small-cell lung cancer patients is a risk factor for early death.
Season of diagnosis has a survival effect on numerous cancers; i.e., cancer patients live longer if the diagnosis is made in the summer rather than the winter.87,88 Although no one has proven vitamin D causes this summer-season treatment effect, vitamin D's anticancer mechanism of action is basic to all cancers. Thus, it is reasonable to hypothesize a general cancer treatment effect, at least in cancer's early stages, when aberrant cells are more likely to retain both the vitamin D receptor and the enzyme needed to activate vitamin D.
Practitioners who treat type-2 diabetic or hypertensive patients with physiological doses of vitamin D should be prepared for the possibility of either hypoglycemia or hypotension, especially after several months of treatment. Theoretically, such doses of vitamin D should eventually lower both blood sugar and blood pressure, although blood sugars may worsen for several weeks after initiation or increase of vitamin D. Should either hypoglycemia or hypotension occur, the diabetic and/or hypertensive medication should be lowered, not the vitamin D.
Although modern science knows little or nothing about the metabolic clearance of vitamin D in different disease states, it is reasonable to predict that vitamin D is cleared more rapidly in some disease states. For example, patients with diabetes, HIV, or cancer may rapidly use 25(OH)D as substrate to make large amounts of 1,25(OH)2D to fight their disease. Therefore, a patient with cancer may require significantly higher doses of vitamin D to maintain 25(OH)D levels of 55-70 ng/ mL than a healthy adult of similar weight and body fat. Practitioners should supplement such patients (assuming they are not hypercalcemic) to high natural levels, even if it means taking 10,000 IU or more per day. Frequent monitoring of 25(OH)D and calcium levels should guide dosing in patients with cancer and other serious illnesses, and such treatment should be adjunc-tive and never take the place of standard treatment.
The authors believe that those who claim the lack of RCTs showing vitamin D's effectiveness as adjuvant cancer treatment means it should never be so used miss an important point. For example, recent studies show a high incidence of vitamin D deficiency in patients undergoing treatment for cancer.89 Even at the end of summer, 48 percent of cancer patients in Boston had levels less than 20 ng/mL.89 In another study, 72 percent of 60 cancer patients had 25(OH)D levels less than 30 ng/mL, and virtually none had natural levels.90 A 1998 study of inpatients at Massachusetts General Hospital found 57 percent had 25(OH)D levels less than 15 ng/mL.91
Thus, the question should not be, "Should cancer (or multiple sclerosis, septic, cardiac, HIV, or hepatitis B ) patients be treated with vitamin D?" The better question is, "Should practitioners routinely screen and aggressively treat vitamin D deficiency in patients with serious or potentially fatal illnesses, or should such patients combat their disease vitamin D deficient?" As referenced above, the vast majority of such patients probably expire severely vitamin D deficient.
Vitamin D Toxicity
Vitamin D toxicity is exceedingly rare and few practitioners ever see it, 92 although that could change with the recent availability of 50,000 IU capsules. Toxicity is secondary to the unbridled effects of hypercalcemia. In chronic toxicity, first urine calcium and then serum calcium will begin to gradually increase when 25(OH)D levels exceed some level above 150 ng/mL. Such levels must be associated with hypercalcemia in order to indict vitamin D. Chronic vitamin D toxicity results when hypercalcemia goes undetected and calcifies internal organs, especially the kidneys. In order to produce hypercalcemia, most adults would have to take in excess of 10,000 IU per day for many months or even years. Most patients with vitamin D toxicity recover fully by simply stopping the vitamin D and practicing strict sun-avoidance.
Credible evidence of vitamin D toxicity in those chronically consuming 10,000 IU of supplemental cholecalciferol daily is absent in the literature. In fact, the literature contains few cases of cholecalciferol toxicity from supplement use; virtually all the reported cases of hypercalcemia are from faulty industrial production, labeling errors, dosing errors, and patients treated medically with pharmacological doses of ergocalciferol.
The current Adequate Intakes and Upper Limits are for medically unsupervised intake by adults and children, set by the Institute of Medicine's Food and Nutrition Board (FNB) in 1997, and do not apply to medically supervised treatment.
Surprisingly, the FNB says Adequate Intake is the same 200 IU/day for the smallest infant as it is for the largest pregnant woman. Likewise, the FNB's Upper Limit for both one-year-old children and forty-year-old adults is 2,000 IU/day, a limit based on old and faulty literature.93 The current official recommendations are illogical; for example, how can 200 IU/day be the adequate intake for both a 3-kg infant and a 60-kg pregnant woman, and 2,000 IU/day be the Upper Limit for both a 10-kg child and a 150-kg adult?
Although a 2,000-IU Upper Limit is probably appropriate for infants and young children, such a limit in older children, adolescents, and adults has the effect of both limiting effective treatment of vitamin D deficiency and impairing dose-appropriate interventional research. However, the current 2,000-IU per day Upper Limit does not impair a practitioner's ability to treat vitamin D deficiency with higher doses just as the comparable Upper Limit for calcium does not impair the practitioner's ability to treat hypocalcemia with calcium doses above the Upper Limit once hypocalcemia is properly diagnosed.
(Note: Upper limit was raised to 4,000 IU after this paper was published)
Practitioners who use doses above 2,000 IU per day should periodically monitor serum 25(OH)D levels, especially if patients are on other medications. Periodic monitoring will also educate the practitioner not only to the safety of supplementation, but to the surprisingly high oral dose required to achieve and maintain adequate serum 25(OH)D levels, especially in the fall and winter.
Absolute and Relative Contraindications to Treatment
The only absolute contraindication to vitamin D supplementation is vitamin D toxicity or allergy to vitamin D, although no reports in the literature were found of acute allergic reactions to vitamin D supplements.
Contraindications to sunlight or artificial UV radiation include a number of
dermatological conditions (porphyrias, xeroderma pigmentosum, albinism), as well as various
photosensitizers (sulfonamides, phenothiazines, tetracyclines, psoralens).
Previous skin cancers, especially cutaneous melanoma, are contraindications to excessive UV exposure, although a recent study found reduced mortality in melanoma patients who continued exposure to sunlight.94 Nevertheless, oral treatment is recommended for patients who have had any type of skin cancer.
Although the liver initially metabolizes vitamin D, liver disease is not a contraindication to treatment of deficiency. The liver conserves the ability to hydroxylate vitamin D despite advanced liver disease.95 A recent study of patients with advanced noncholestatic chronic liver disease recommended treatment of concomitant vitamin D deficiency after finding serum 25(OH)D levels of less than 10 ng/mL predicted coagulopathy, hyperbilirubinemia, hypoalbuminemia, anemia, and thrombocytopenia.96
Vitamin D hypersensitivity syndromes - often confused with vitamin D toxicity - occur when extrarenal tissues produce 1,25(OH)2D in an unregulated manner, causing hypercalcemia.97 These syndromes are diagnosed by measuring serum calcium (elevated), 25(OH)D (normal or low), and 1,25(OH)2D (elevated).
Vitamin D hypersensitivity syndromes can occur in some of the granulomatous diseases (especially sarcoidosis and tuberculosis), and in some cancers (especially non-Hodgkin's lymphoma and oat cell carcinoma of the lung). Such conditions may be unmasked by vitamin D treatment; for example, sarcoidosis may become clinically evident after summer sun exposure.
Therefore, hypercalcemia is a relative contraindication to vitamin D, sunlight, and artificial UVB radiation. The practitioner should carefully evaluate any hypercalcemic patient for the cause of hypercalcemia. Once the cause is clear, should the practitioner decide to treat concomitant vitamin D deficiency - despite the hypercalcemia - it should only be if the hypercalcemia is mild to moderate (<12 mg/dL) and should proceed cautiously, with frequent monitoring of clinical condition, urine and serum calcium, 25(OH)D, and 1,25(OH)2D. Vitamin D, especially in large doses, could theoretically precipitate a worsening clinical course in such patients.
Summary
Vitamin D deficiency is endemic and is associated with numerous diseases. Understanding vitamin D's physiology and having a high index of suspicion are keys to determining the diagnosis. Serum 25(OH)D levels less than 40 ng/mL are seldom found in those living in a sun-rich environment and such levels are needed to assure normalization of the pharmacokinetics of vitamin D. Treatment with sunlight or artificial UVB radiation is simple but increases the risk of non-melanoma skin cancers and ages the skin. Sunburn increases the risk of malignant melanoma. Adequate oral supplementation will require doses that might make a practitioner initially uncomfortable, as physiological doses of vitamin D, in the absence of sun exposure, probably range between 400 IU/day for premature infants to 10,000 IU/day for the morbidly obese.
Treatment of vitamin D deficiency in otherwise healthy patients must be individualized due to the numerous factors affecting 25(OH)D levels, and doses should be adequate to maintain serum 25(OH)D levels between 40-70 ng/mL. Patients with chronic diseases associated with vitamin D deficiency, especially internal cancers, should be supplemented with doses adequate to maintain 25(OH)D levels in the higher normal range, 55-70 ng/mL. Caution is required in any patient with hypercalcemia. The use of short-term pharmacological doses of vitamin D as treatment for the common cold or flu - 2,000 IU/kg/day for several days - while theoretically promising, awaits further study.
